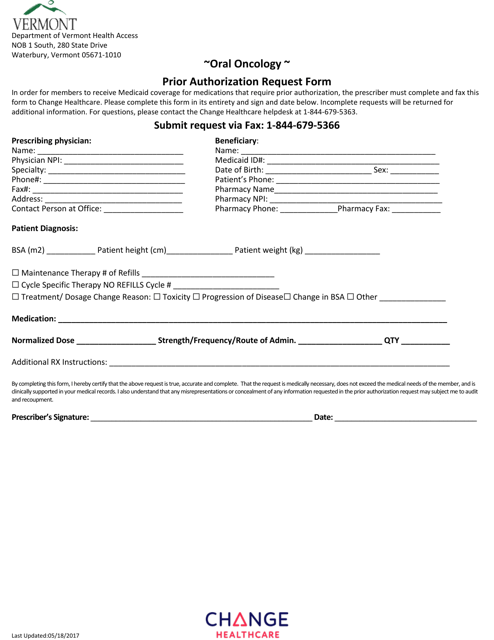
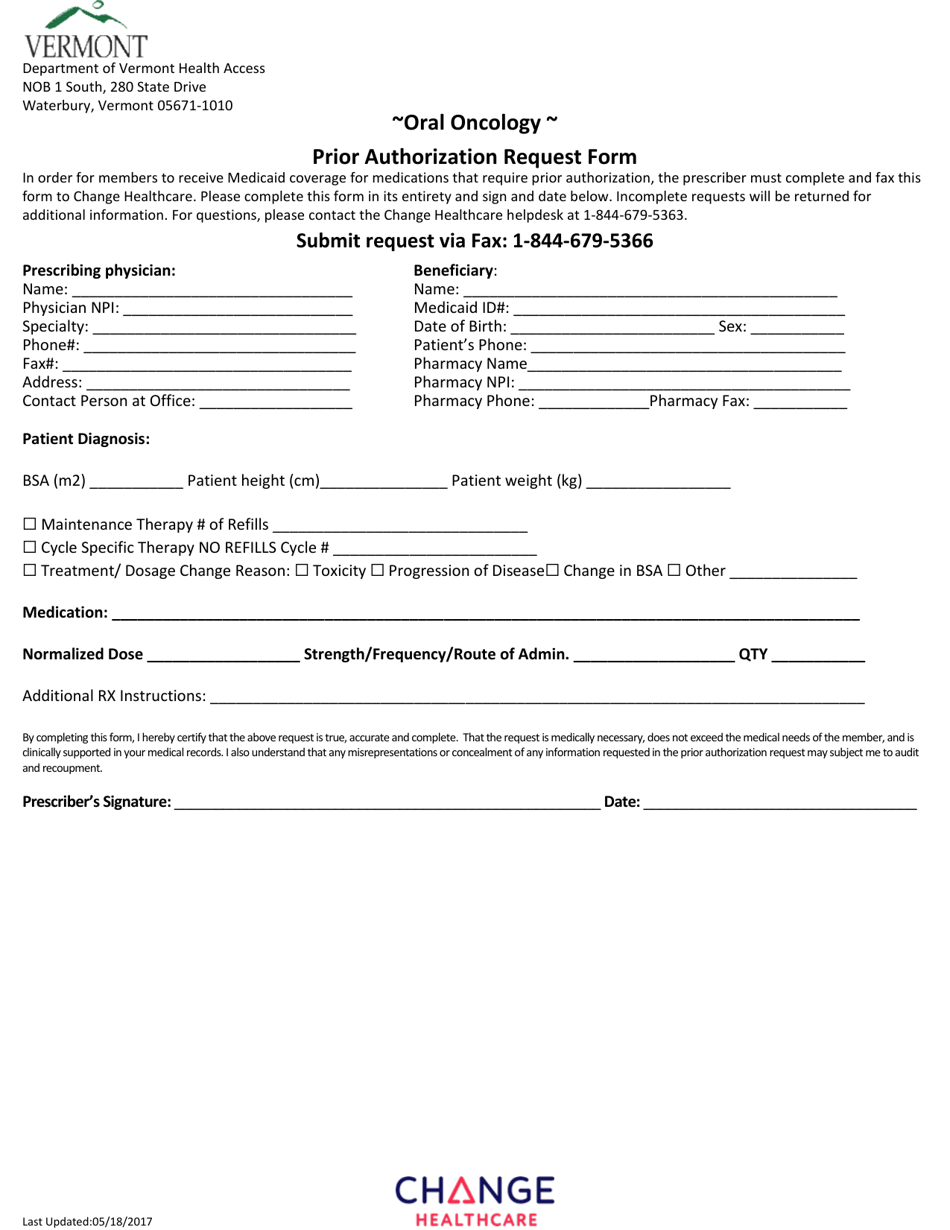
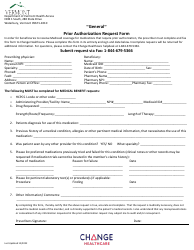
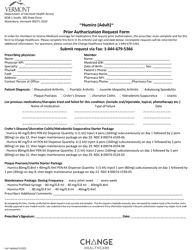
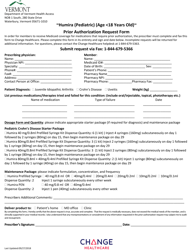
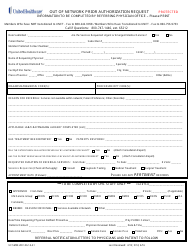
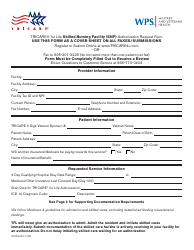
Oral Oncology Prior Authorization Request Form - Vermont
Oral Oncology Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is the Oral Oncology Prior Authorization Request Form?
A: The Oral Oncology Prior Authorization Request Form is a document used in Vermont to request prior authorization for oral oncology medications.
Q: Why is prior authorization required for oral oncology medications?
A: Prior authorization is required for oral oncology medications to ensure appropriate use and cost-effectiveness.
Q: What information is needed on the Oral Oncology Prior Authorization Request Form?
A: The form requires information such as patient details, prescribing physician information, medication details, and clinical documentation.
Q: How long does it take to process a prior authorization request for oral oncology medications?
A: The processing time for prior authorization requests may vary, but typically takes a few days to a week.
Q: Who can help me fill out the Oral Oncology Prior Authorization Request Form?
A: Your healthcare provider or their office staff can assist you in completing the form.
Q: What happens after the Oral Oncology Prior Authorization Request Form is submitted?
A: The form is reviewed by the insurance company to determine if the requested medication is covered under the plan and meets the necessary criteria.
Q: Can I appeal the decision if my prior authorization request is denied?
A: Yes, you have the right to appeal the decision if your prior authorization request is denied. The process for appeal may vary by insurance company.
Q: Are all oral oncology medications subject to prior authorization?
A: Not all oral oncology medications may require prior authorization. The specific requirements may vary depending on the insurance plan.
Q: Can I start taking the oral oncology medication while waiting for the prior authorization decision?
A: It is important to wait for the prior authorization decision before starting the medication, as insurance coverage cannot be guaranteed without prior authorization approval.
Form Details:
- Released on May 18, 2017;
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.