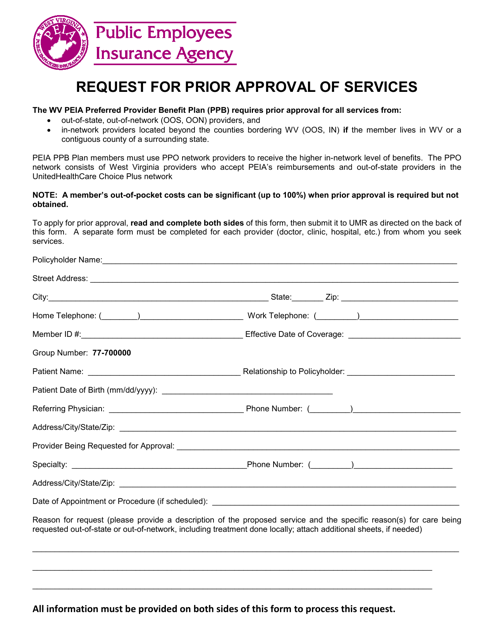
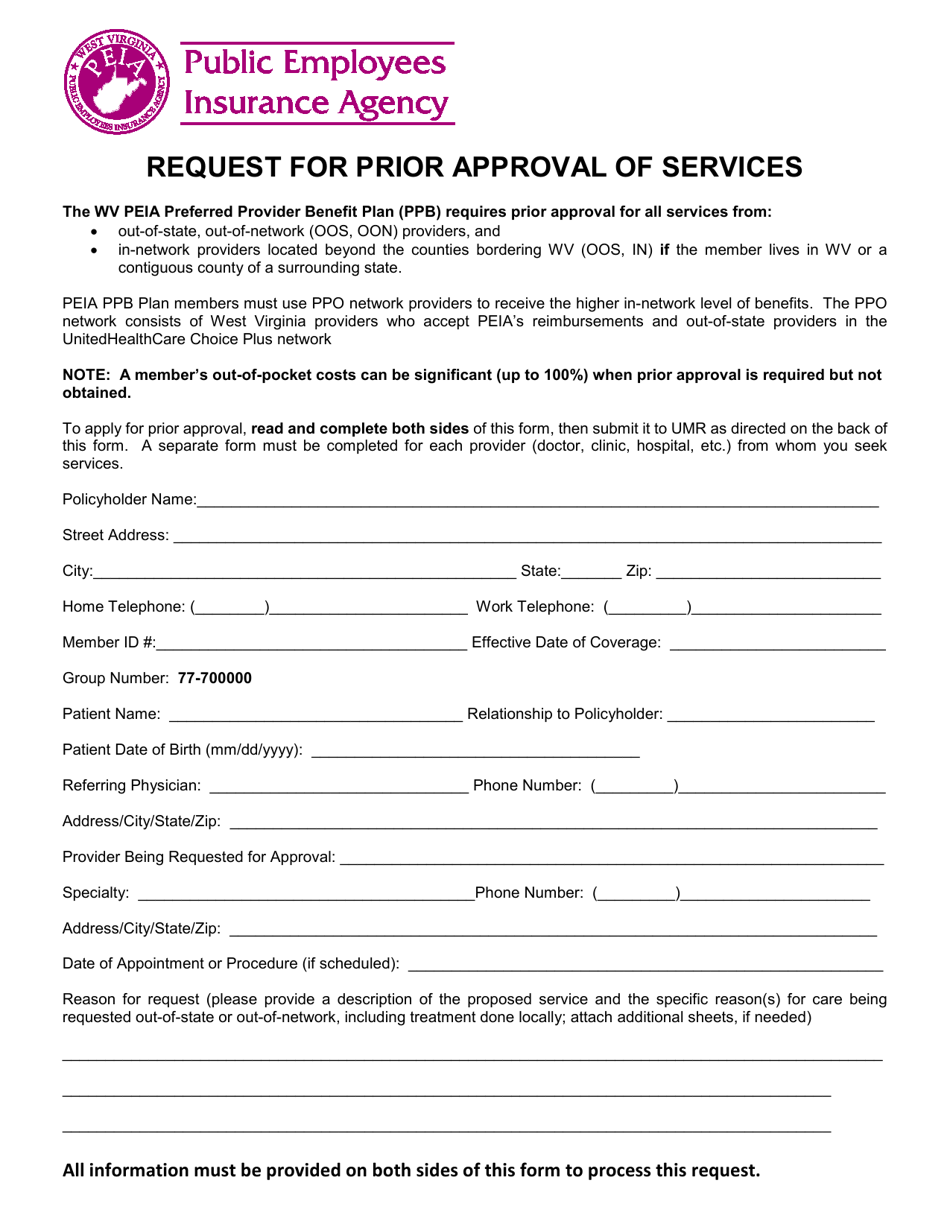
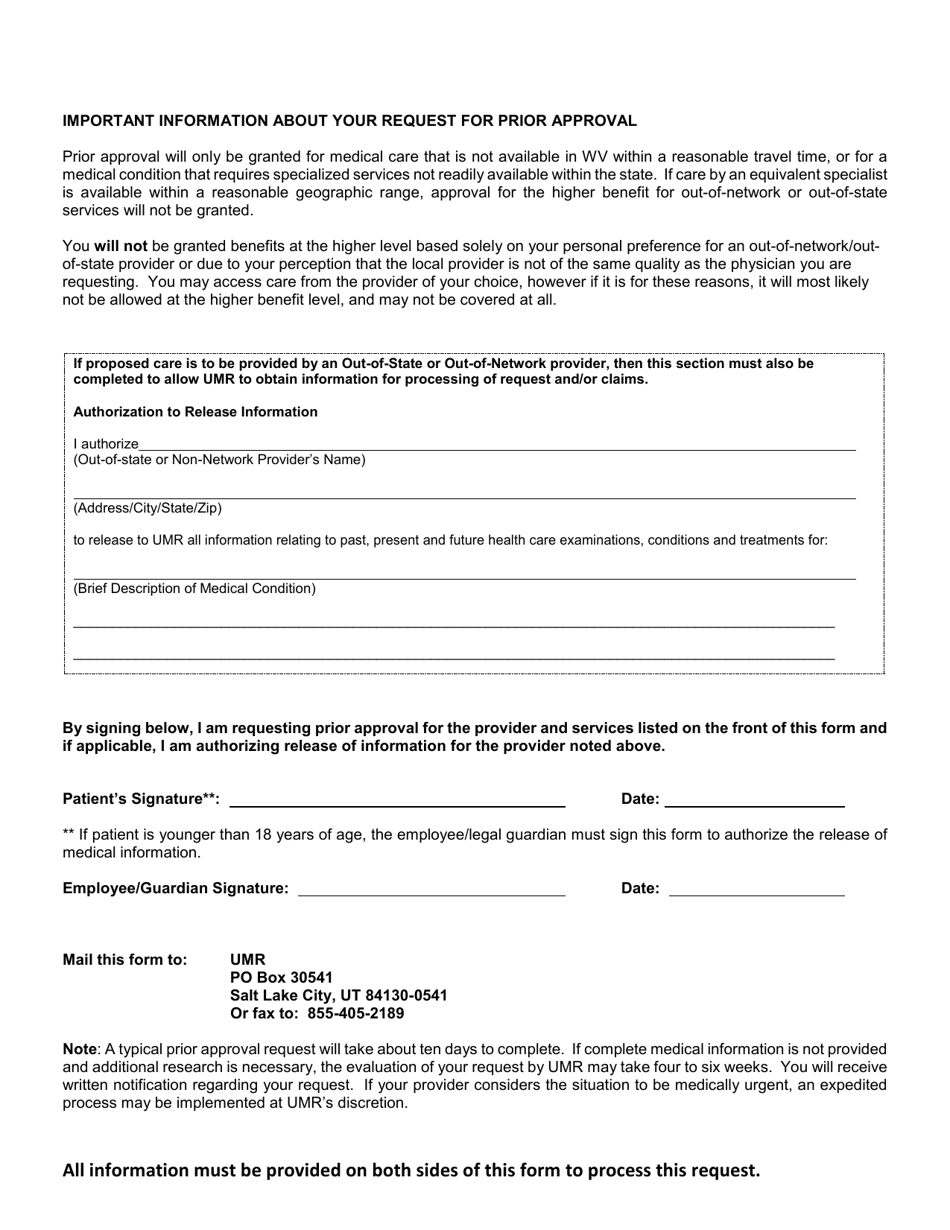
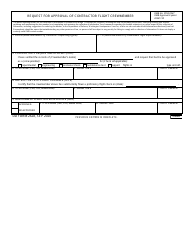
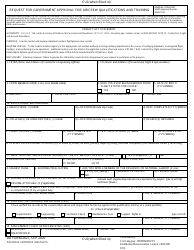
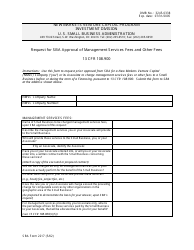
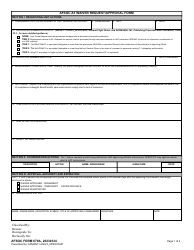
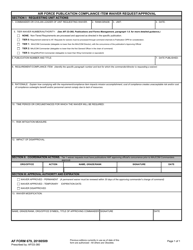
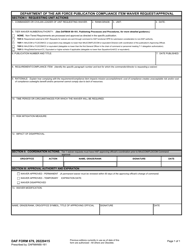
Request for Prior Approval of Services - West Virginia
Request for Prior Approval of Services is a legal document that was released by the West Virginia Public EmployeesInsurance Agency - a government authority operating within West Virginia.
FAQ
Q: What is a Request for Prior Approval of Services?
A: A Request for Prior Approval of Services is a formal request made by individuals or providers to obtain approval for certain healthcare services in West Virginia.
Q: Who can submit a Request for Prior Approval of Services?
A: Both individuals seeking healthcare services and healthcare providers can submit a Request for Prior Approval of Services in West Virginia.
Q: What is the purpose of a Request for Prior Approval of Services?
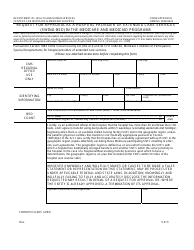
A: The purpose of a Request for Prior Approval of Services is to seek approval from the healthcare insurance provider before receiving certain healthcare services, procedures, or treatments. This ensures that the services meet the coverage criteria and are medically necessary.
Q: What services require prior approval in West Virginia?
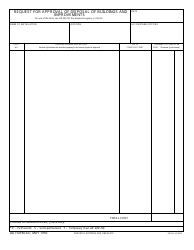
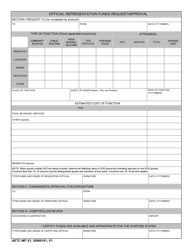
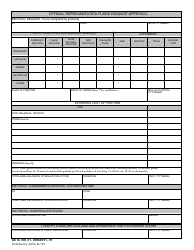
A: Specific healthcare services, procedures, or treatments that require prior approval vary depending on the insurance plan. Common examples include surgeries, certain medications or therapies, durable medical equipment, and out-of-network services.
Q: How can I submit a Request for Prior Approval of Services?
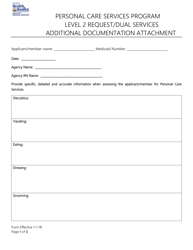
A: To submit a Request for Prior Approval of Services in West Virginia, individuals or healthcare providers typically need to complete a form provided by the insurance company. This form includes information about the requested services, medical necessity, and supporting documentation.
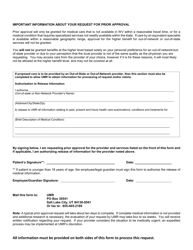
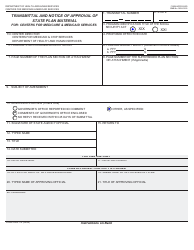
Q: What happens after submitting a Request for Prior Approval of Services?
A: After submitting a Request for Prior Approval of Services, the insurance provider will review the request and determine whether to approve or deny the requested services. They may request additional information or documentation to support the request.
Q: What should I do if my Request for Prior Approval of Services is denied?
A: If a Request for Prior Approval of Services is denied, individuals or healthcare providers have the right to appeal the decision. This involves providing additional evidence or justification for the requested services and requesting a review of the denial.
Q: Are all healthcare services subject to prior approval in West Virginia?
A: Not all healthcare services require prior approval in West Virginia. The coverage and prior approval requirements vary depending on the specific insurance plan and policy terms. It is important to review the plan documents or contact the insurance provider for information regarding specific services.
Form Details:
- The latest edition currently provided by the West Virginia Public Employees Insurance Agency;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the West Virginia Public Employees Insurance Agency.