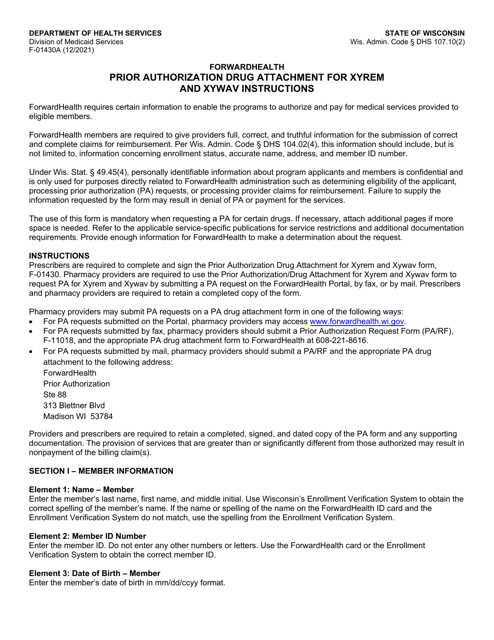
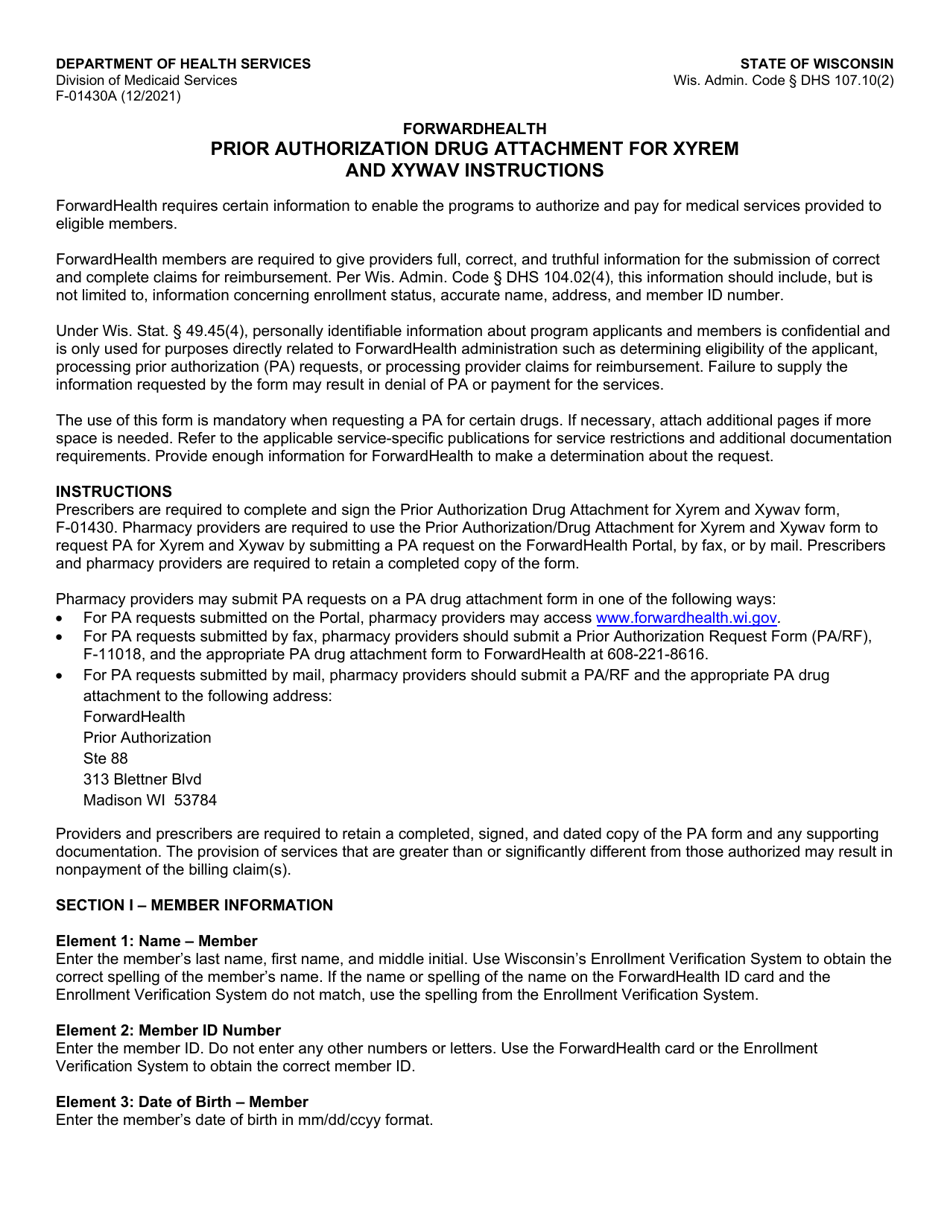
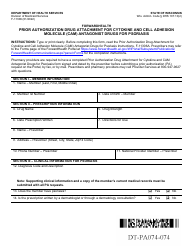
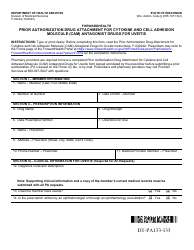
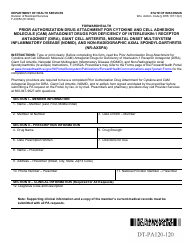
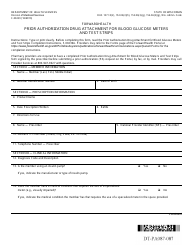
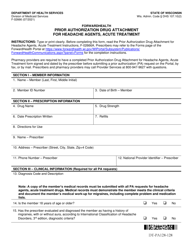
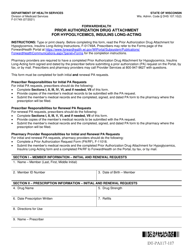
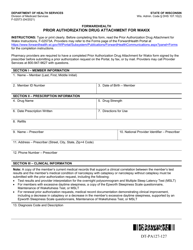
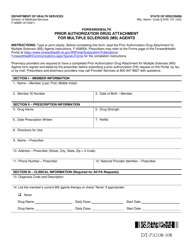
Instructions for Form F-01430 Prior Authorization Drug Attachment for Xyrem and Xywav - Wisconsin
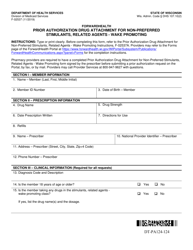
This document contains official instructions for Form F-01430 , Prior Authorization Drug Attachment for Xyrem and Xywav - a form released and collected by the Wisconsin Department of Health Services. An up-to-date fillable Form F-01430 is available for download through this link.
FAQ
Q: What is Form F-01430?
A: Form F-01430 is a prior authorization drug attachment specifically for Xyrem and Xywav in the state of Wisconsin.
Q: What is Xyrem and Xywav?
A: Xyrem and Xywav are medications used to treat a sleep disorder called narcolepsy.
Q: What is a prior authorization?
A: A prior authorization is a process where your healthcare provider requests approval from your insurance company before certain medications are covered.
Q: Why do I need to fill out Form F-01430?
A: You need to fill out Form F-01430 if you want your insurance to cover Xyrem or Xywav.
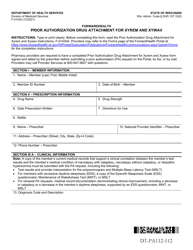
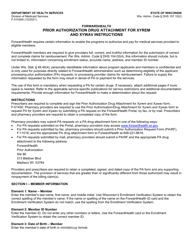
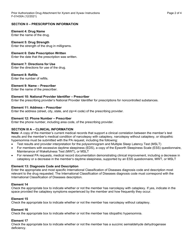
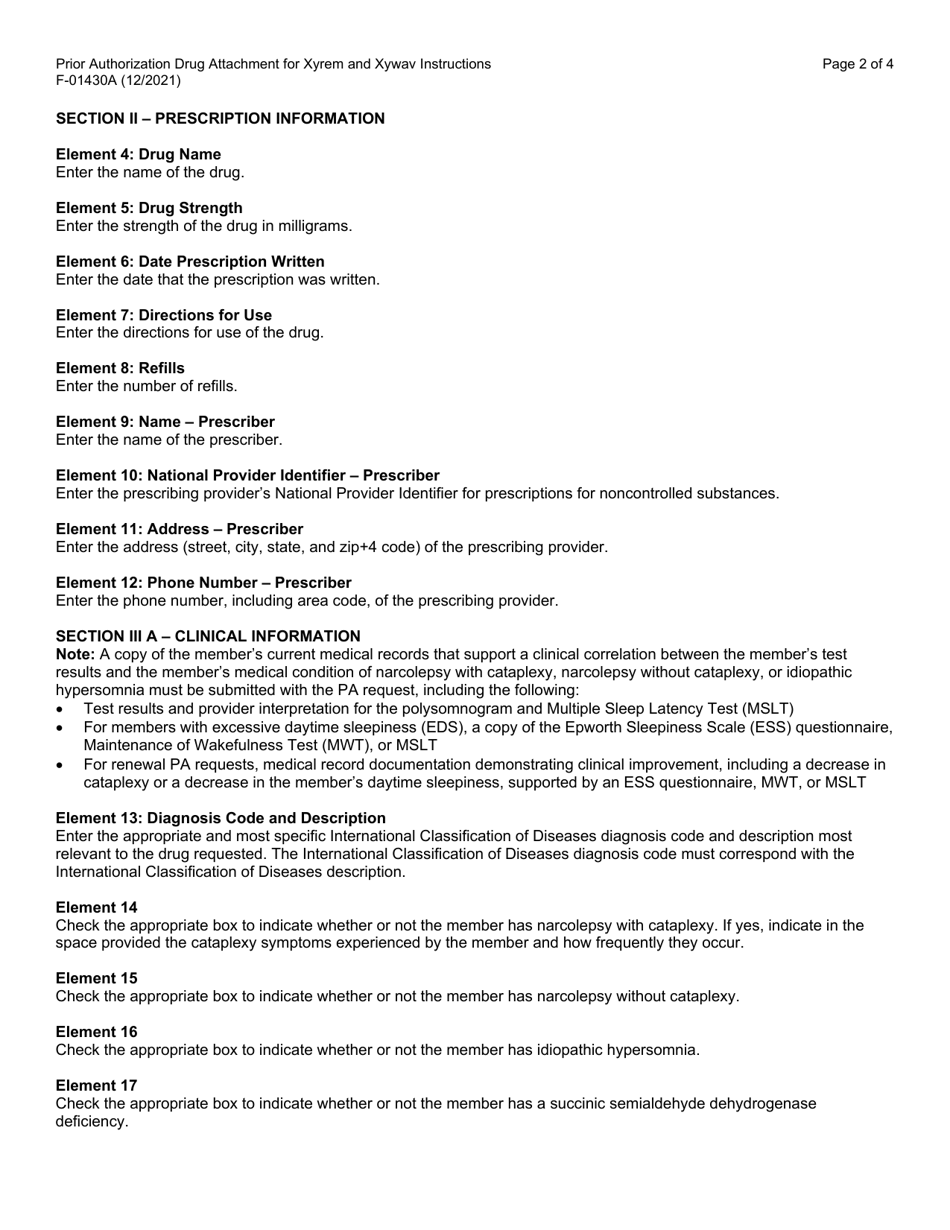
Q: What information do I need to provide on Form F-01430?
A: You will need to provide your personal information, healthcare provider's information, and details about your medical condition and prescription.
Q: How long does it take to process a prior authorization?
A: The processing time may vary, but it typically takes around 5-7 business days.
Q: What should I do if my prior authorization is denied?
A: If your prior authorization is denied, you can appeal the decision or discuss alternative medications with your healthcare provider.
Q: Do I need to submit Form F-01430 for every refill?
A: No, you only need to submit Form F-01430 once unless your insurance company specifically requests an updated form.
Instruction Details:
- This 4-page document is available for download in PDF;
- Actual and applicable for the current year;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of forms released by the Wisconsin Department of Health Services.