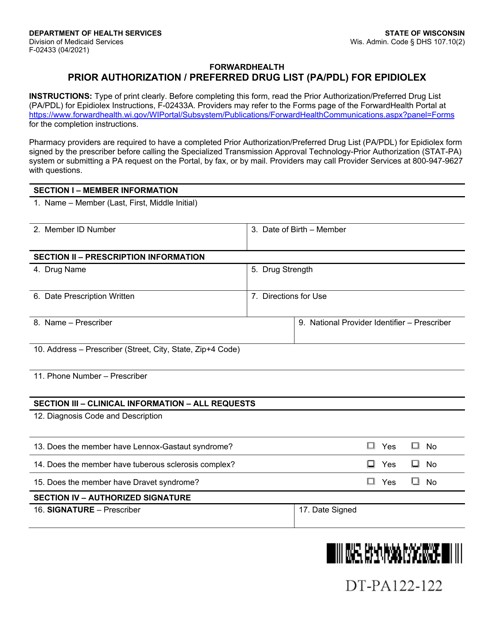
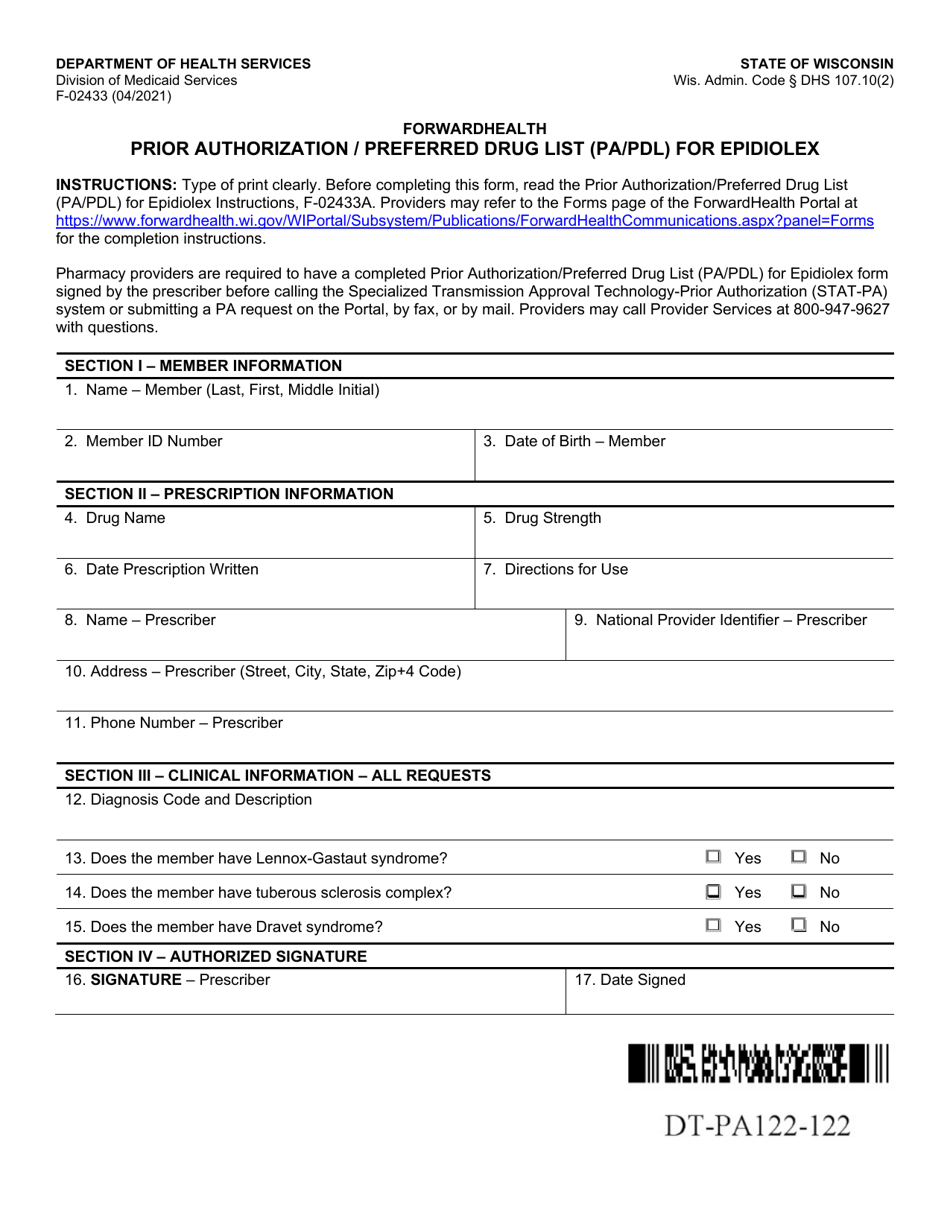
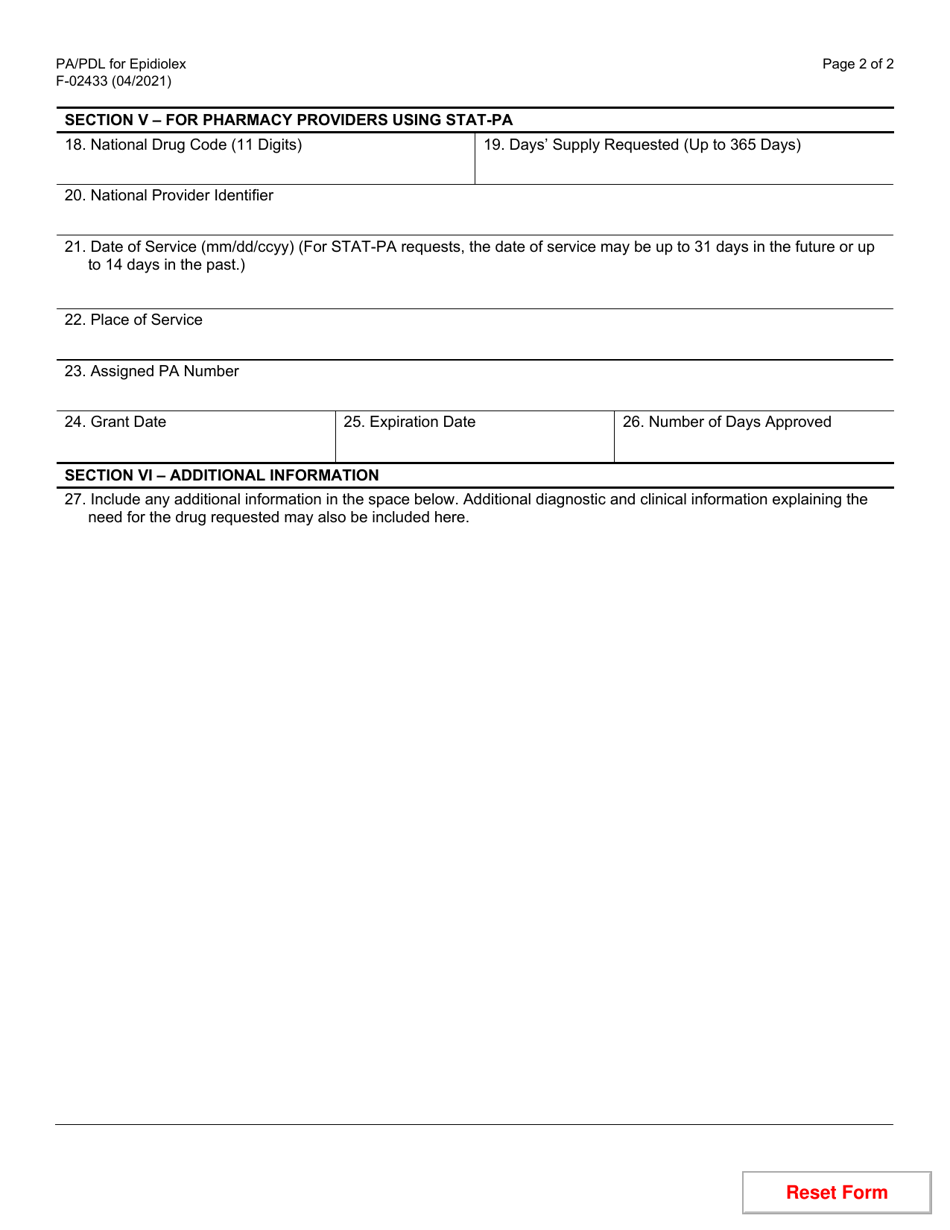
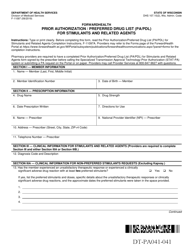
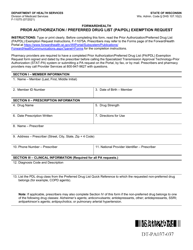
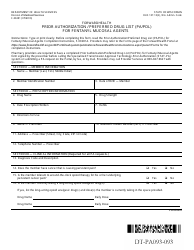
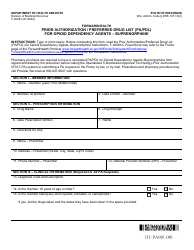
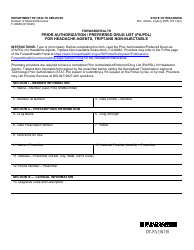
Form F-02433 Prior Authorization / Preferred Drug List (Pa / Pdl) for Epidiolex - Wisconsin
What Is Form F-02433?
This is a legal form that was released by the Wisconsin Department of Health Services - a government authority operating within Wisconsin. Check the official instructions before completing and submitting the form.
FAQ
Q: What is Form F-02433?
A: Form F-02433 is a Prior Authorization/Preferred Drug List (Pa/Pdl) for Epidiolex in Wisconsin.
Q: What is Prior Authorization?
A: Prior Authorization is a process where you need approval from your insurance company before they will cover the cost of a medication.
Q: What is a Preferred Drug List?
A: A Preferred Drug List is a list of medications that are preferred by your insurance plan, usually because they are cost-effective or have been proven to be effective.
Q: What is Epidiolex?
A: Epidiolex is a medication that contains cannabidiol (CBD) and is used to treat certain types of seizures.
Q: Why do I need to fill out Form F-02433?
A: You need to fill out Form F-02433 if you want your insurance to cover the cost of Epidiolex.
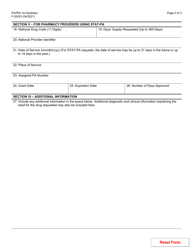
Q: What information do I need to provide on Form F-02433?
A: You will need to provide information about your healthcare provider, your diagnosis, and any previous medications you have tried.
Q: How long does the prior authorization process take?
A: The length of time for the prior authorization process can vary, but it is usually within a few days to a few weeks.
Q: Will my insurance cover the cost of Epidiolex?
A: Coverage for Epidiolex depends on your insurance plan and whether or not it is listed on the Preferred Drug List. Filling out Form F-02433 increases your chances of getting coverage.
Q: Can I appeal if my prior authorization request is denied?
A: Yes, you can appeal the decision if your prior authorization request for Epidiolex is denied. Your insurance company will provide instructions on how to appeal.
Form Details:
- Released on April 1, 2021;
- The latest edition provided by the Wisconsin Department of Health Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form F-02433 by clicking the link below or browse more documents and templates provided by the Wisconsin Department of Health Services.