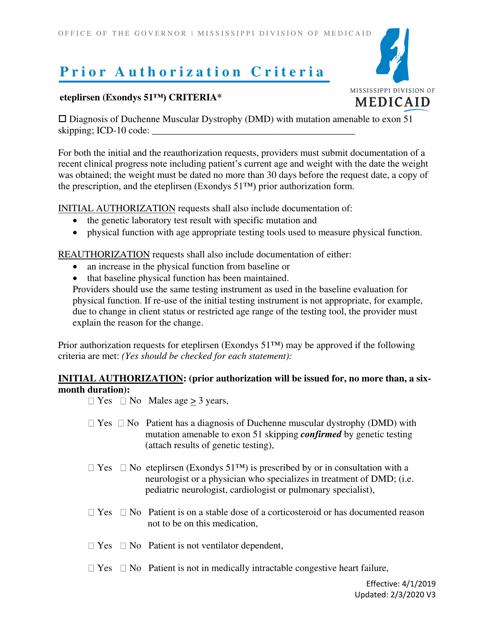
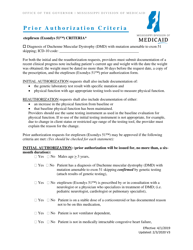
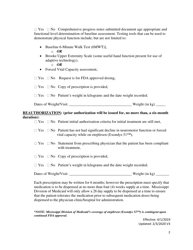
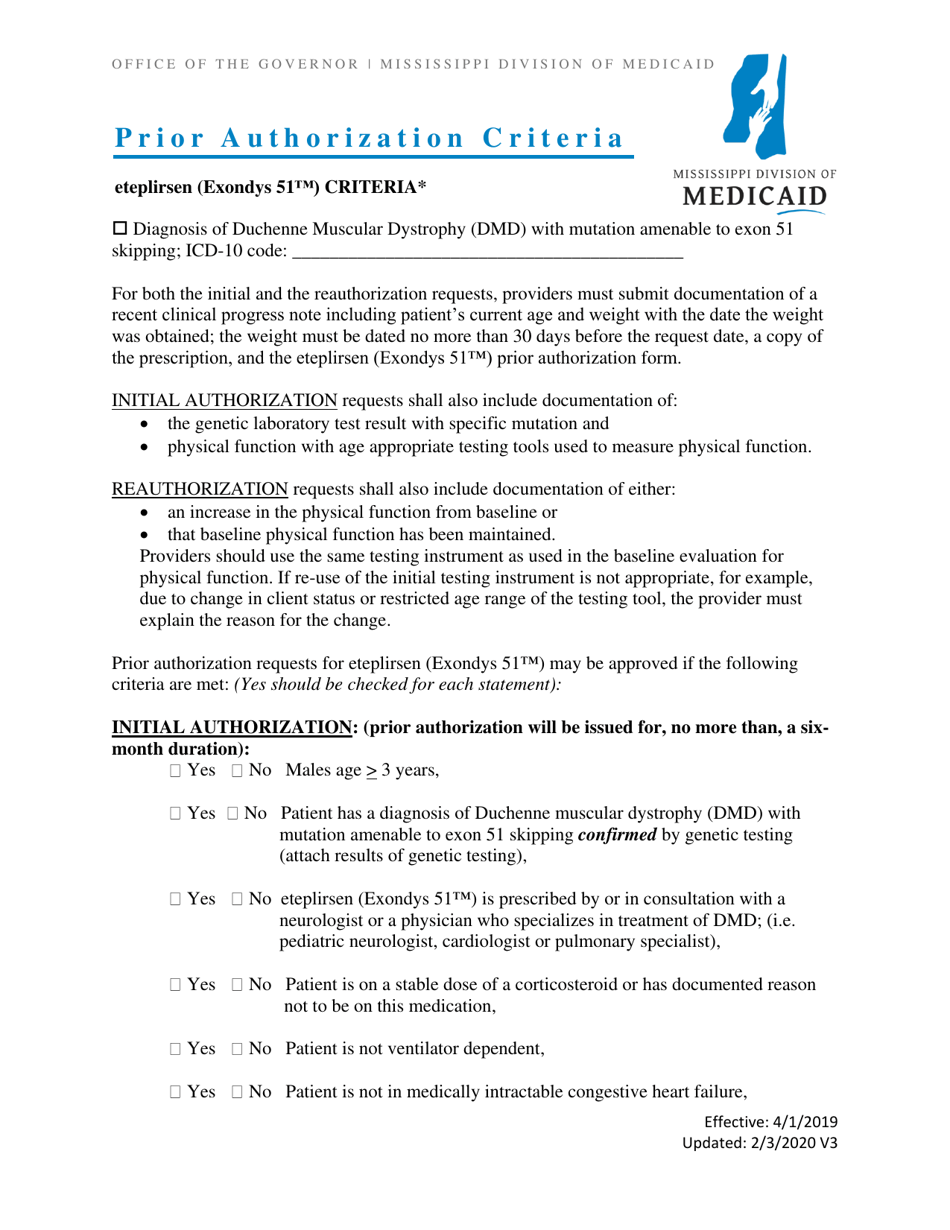
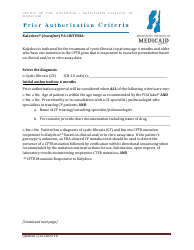
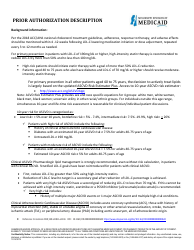
Prior Authorization Criteria - Eteplirsen (Exondys 51) - Mississippi
Prior Authorization Criteria - Eteplirsen (Exondys 51) is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is Eteplirsen?
A: Eteplirsen is a medication used in treating certain types of Duchenne muscular dystrophy.
Q: What is Exondys 51?
A: Exondys 51 is the brand name for eteplirsen.
Q: What is Duchenne muscular dystrophy?
A: Duchenne muscular dystrophy is a genetic disorder characterized by progressive muscle degeneration and weakness.
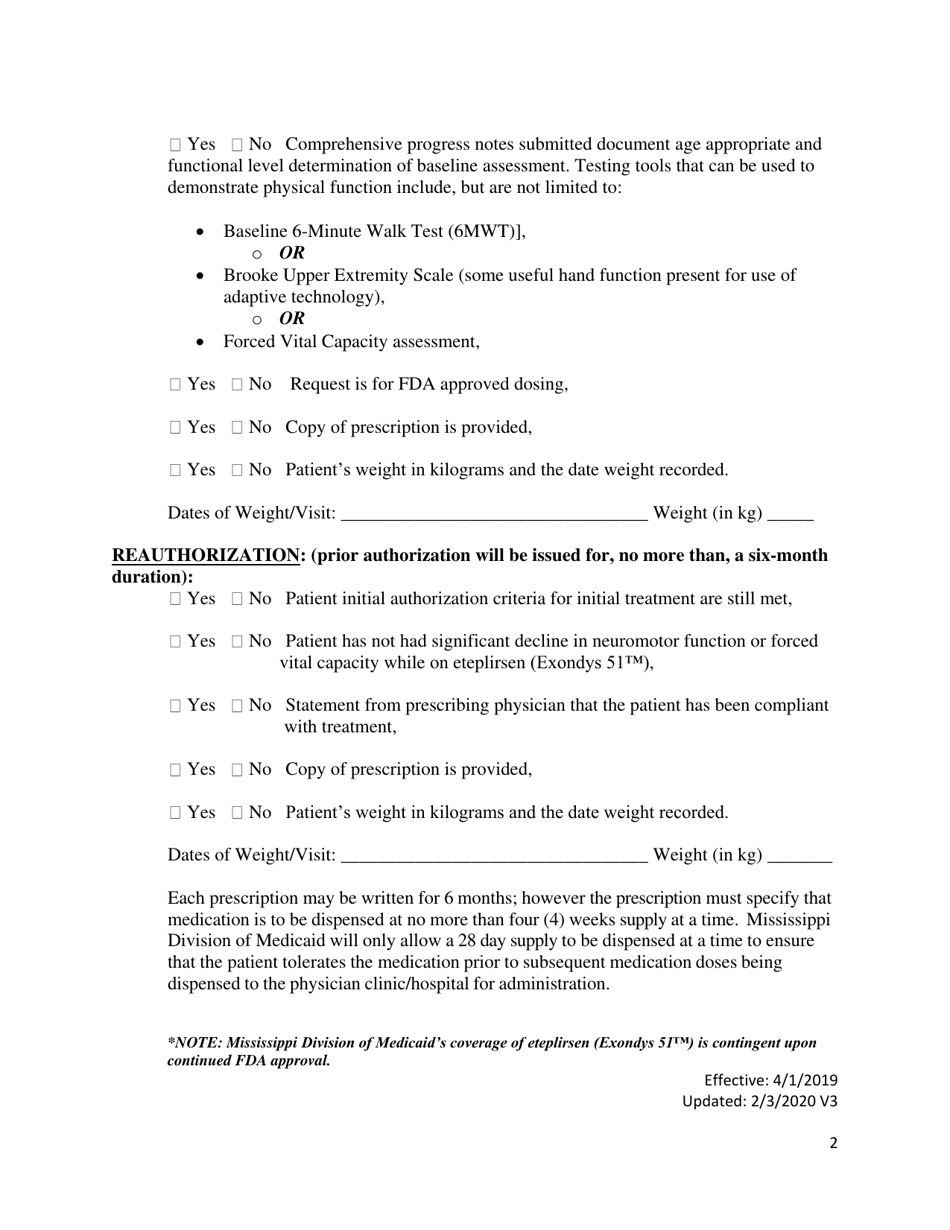
Q: Does Mississippi require prior authorization for Eteplirsen?
A: Yes, Mississippi requires prior authorization for Eteplirsen.
Q: What are prior authorization criteria?
A: Prior authorization criteria refer to the specific requirements that must be met for insurance coverage of a medication, such as Eteplirsen.
Q: Who is eligible for Eteplirsen?
A: Individuals with certain types of Duchenne muscular dystrophy may be eligible for Eteplirsen treatment.
Q: Why is prior authorization required for Eteplirsen?
A: Prior authorization helps ensure that the medication is being used appropriately and according to established guidelines.
Q: What should I do if my insurance company denies coverage for Eteplirsen?
A: If your insurance company denies coverage for Eteplirsen, you can file an appeal or seek assistance from your healthcare provider or patient advocacy organizations.
Q: Are there any alternative treatments for Duchenne muscular dystrophy?
A: There are other medications and treatments available for Duchenne muscular dystrophy. It is best to consult with a healthcare provider for personalized recommendations and options.
Form Details:
- Released on February 3, 2020;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.