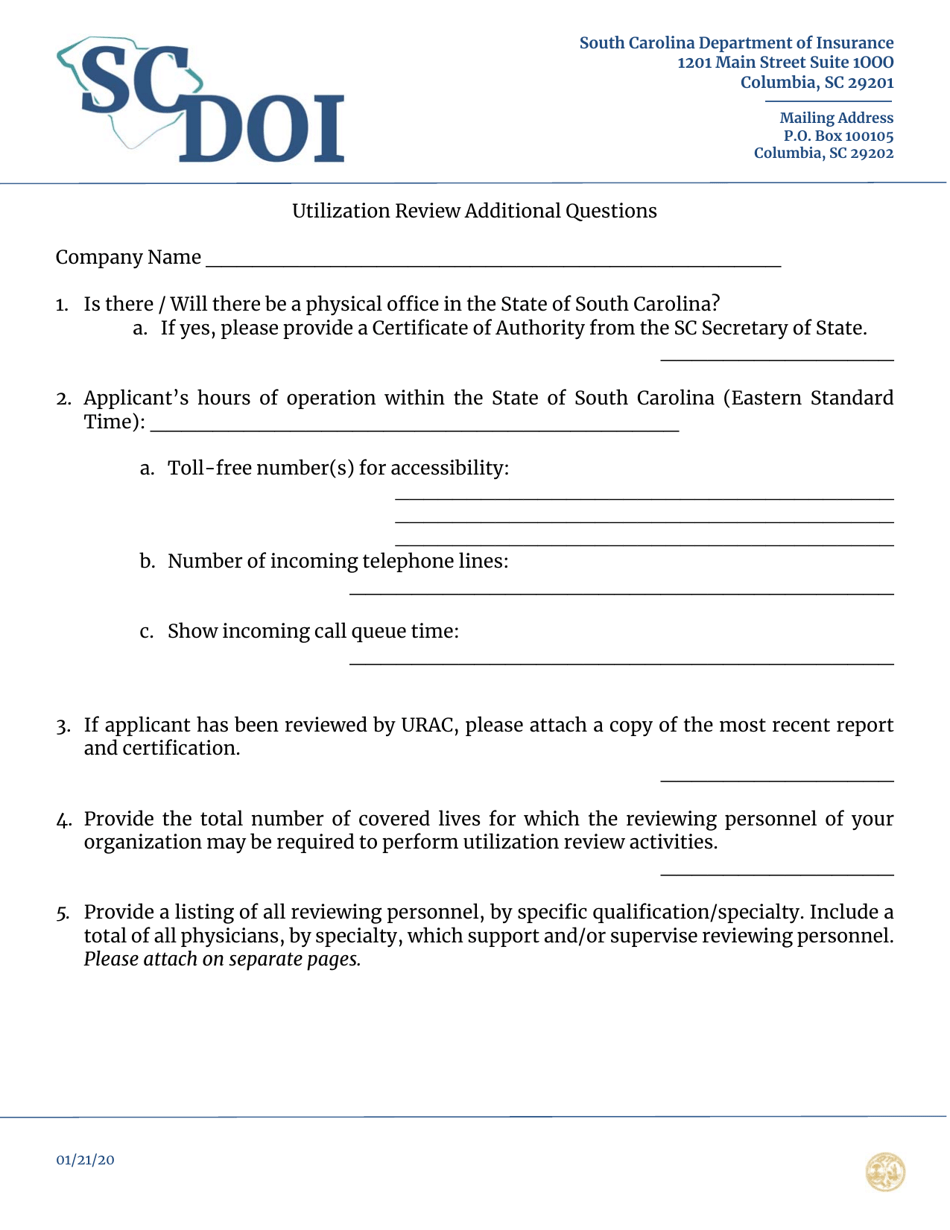
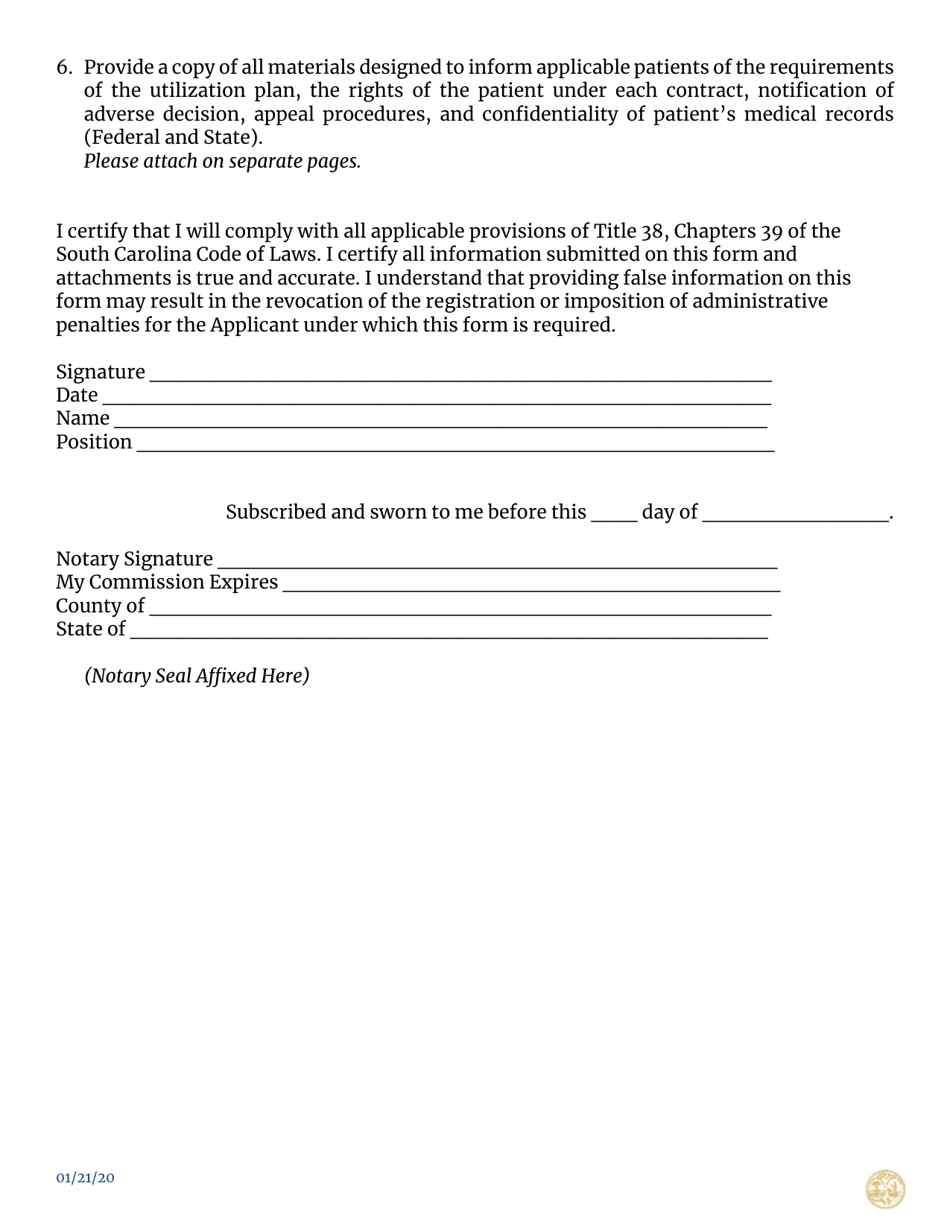
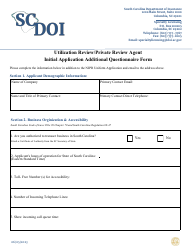
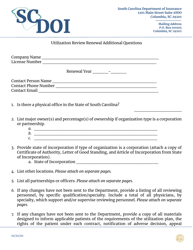
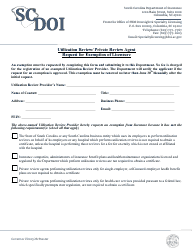
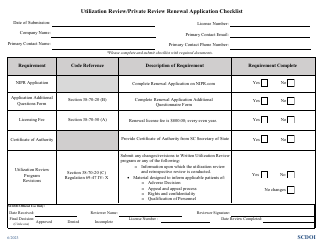
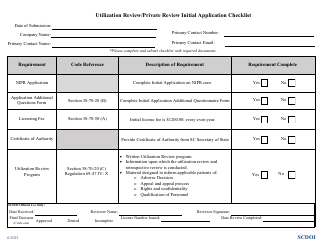
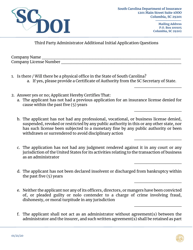
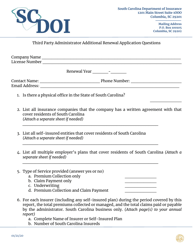
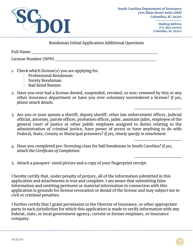
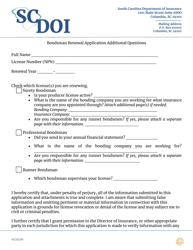
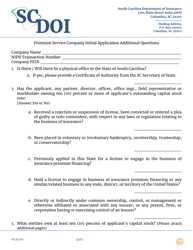
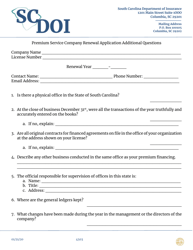
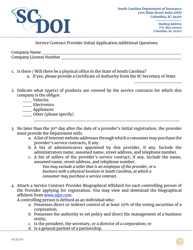
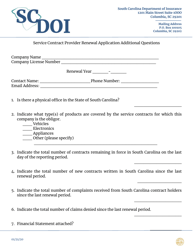
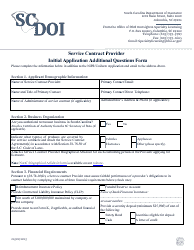
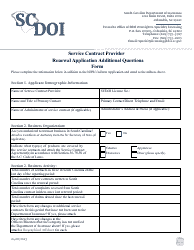
Utilization Review Additional Questions - South Carolina
Utilization Review Additional Questions is a legal document that was released by the South Carolina Department of Insurance - a government authority operating within South Carolina.
FAQ
Q: What is utilization review?
A: Utilization review is a process used by insurance companies to review and evaluate the medical necessity, appropriateness, and efficiency of healthcare services.
Q: Why is utilization review done?
A: Utilization review is done to ensure that the healthcare services being provided are necessary, appropriate, and cost-effective.
Q: Who performs utilization review?
A: Utilization review can be performed by insurance companies, healthcare providers, or third-party organizations contracted by insurance companies.
Q: What is the purpose of utilization review?
A: The purpose of utilization review is to ensure that appropriate healthcare services are being provided and to control healthcare costs.
Q: How does utilization review work?
A: Utilization review involves the review of medical records, treatment plans, and other relevant information to determine the necessity and appropriateness of healthcare services.
Form Details:
- Released on January 21, 2020;
- The latest edition currently provided by the South Carolina Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the South Carolina Department of Insurance.