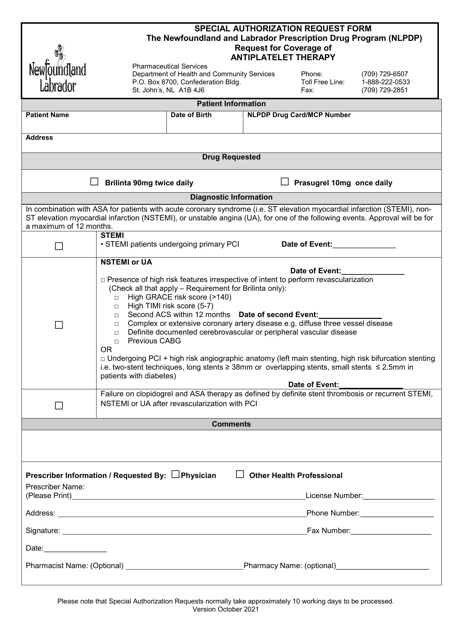
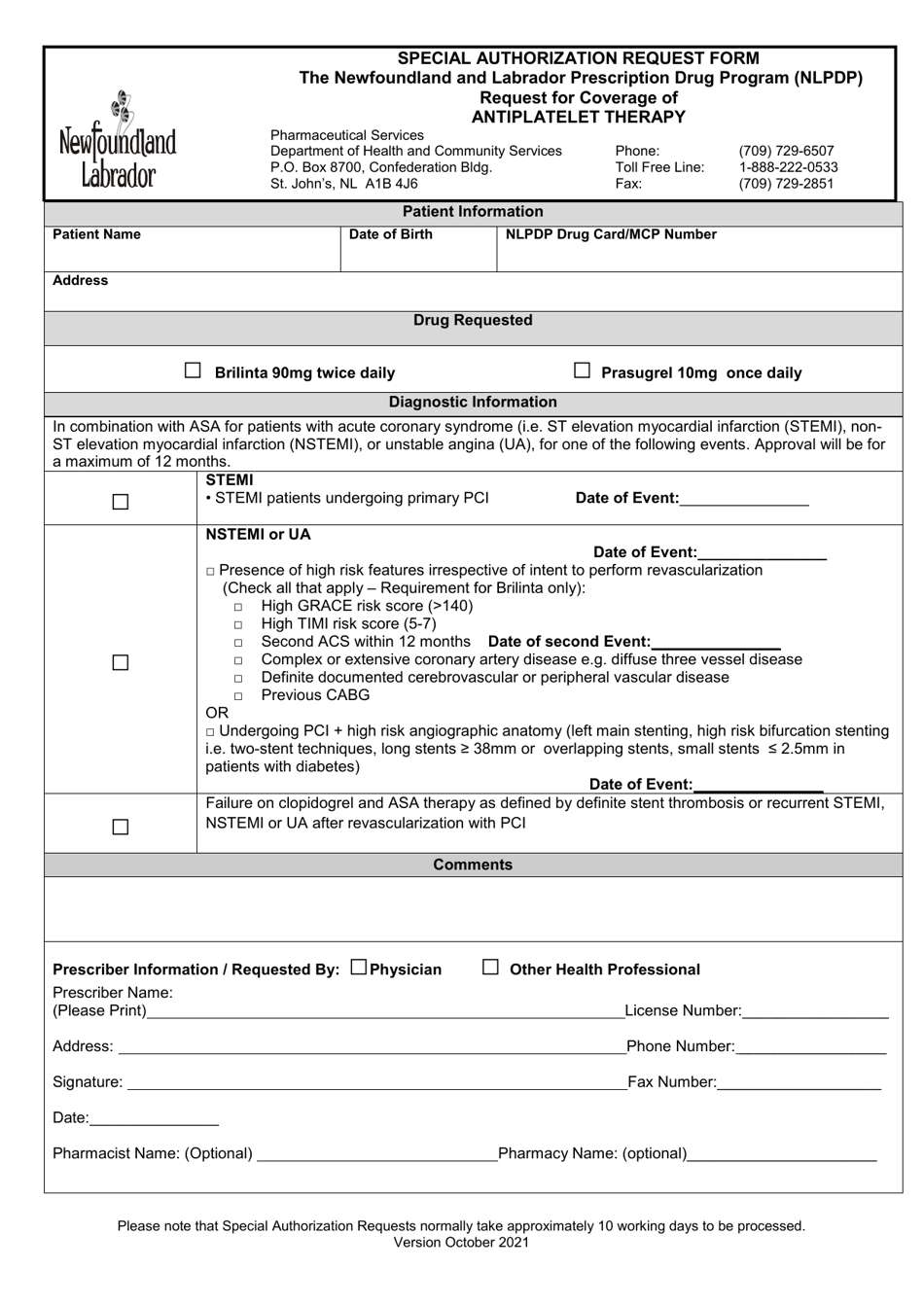
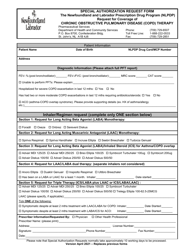
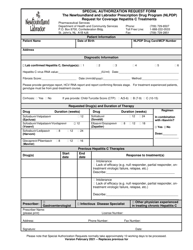
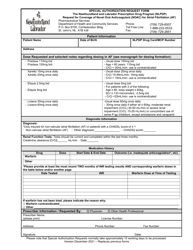
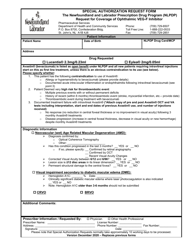
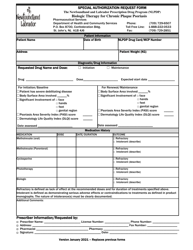
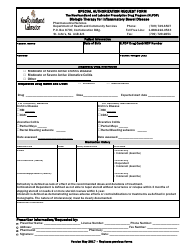
Special Authorization Request Form - Request for Coverage of Antiplatelet Therapy - Newfoundland and Labrador, Canada
The Special Authorization Request Form - Request for Coverage of Antiplatelet Therapy in Newfoundland and Labrador, Canada is used to request coverage for antiplatelet therapy, which is a type of medication to prevent blood clots. This form helps individuals in Newfoundland and Labrador apply for coverage for this particular type of therapy.
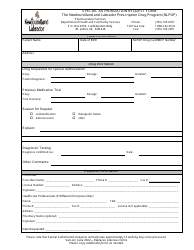
The Special Authorization Request Form for coverage of antiplatelet therapy in Newfoundland and Labrador, Canada is typically filed by the patient's healthcare provider or hospital.
FAQ
Q: What is the Special Authorization Request Form?
A: The Special Authorization Request Form is a form used to request coverage of antiplatelet therapy in Newfoundland and Labrador, Canada.
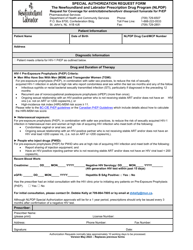
Q: What is antiplatelet therapy?
A: Antiplatelet therapy is a type of medication used to prevent blood clots.
Q: Why would someone need to request coverage for antiplatelet therapy?
A: Someone would need to request coverage for antiplatelet therapy if it is not automatically covered by their insurance or if they require a specific type or brand of antiplatelet medication.
Q: Who can use the Special Authorization Request Form?
A: The Special Authorization Request Form can be used by residents of Newfoundland and Labrador, Canada.
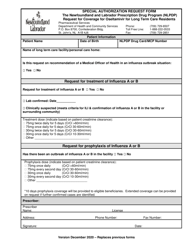
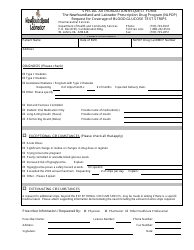
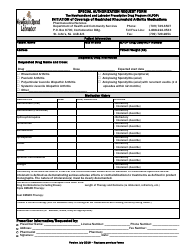
Q: What information is required on the Special Authorization Request Form?
A: The Special Authorization Request Form typically requires information such as the patient's personal details, medical history, and a justification for the request.
Q: Is there a cost associated with submitting the Special Authorization Request Form?
A: There may be a cost associated with submitting the Special Authorization Request Form, such as a processing fee. This information can be found on the form or by contacting the relevant healthcare authority.
Q: How long does it take to receive a decision on the Special Authorization Request?
A: The time it takes to receive a decision on the Special Authorization Request can vary, but it is typically within a few weeks.
Q: What happens if the Special Authorization Request is approved?
A: If the Special Authorization Request is approved, the patient's antiplatelet therapy will be covered by their insurance.
Q: What happens if the Special Authorization Request is denied?
A: If the Special Authorization Request is denied, the patient may need to explore other options for obtaining coverage for their antiplatelet therapy, such as appealing the decision or discussing alternative treatments with their healthcare provider.