This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
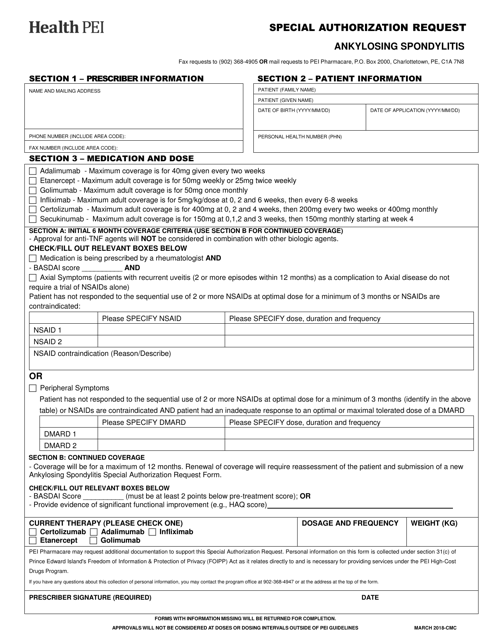
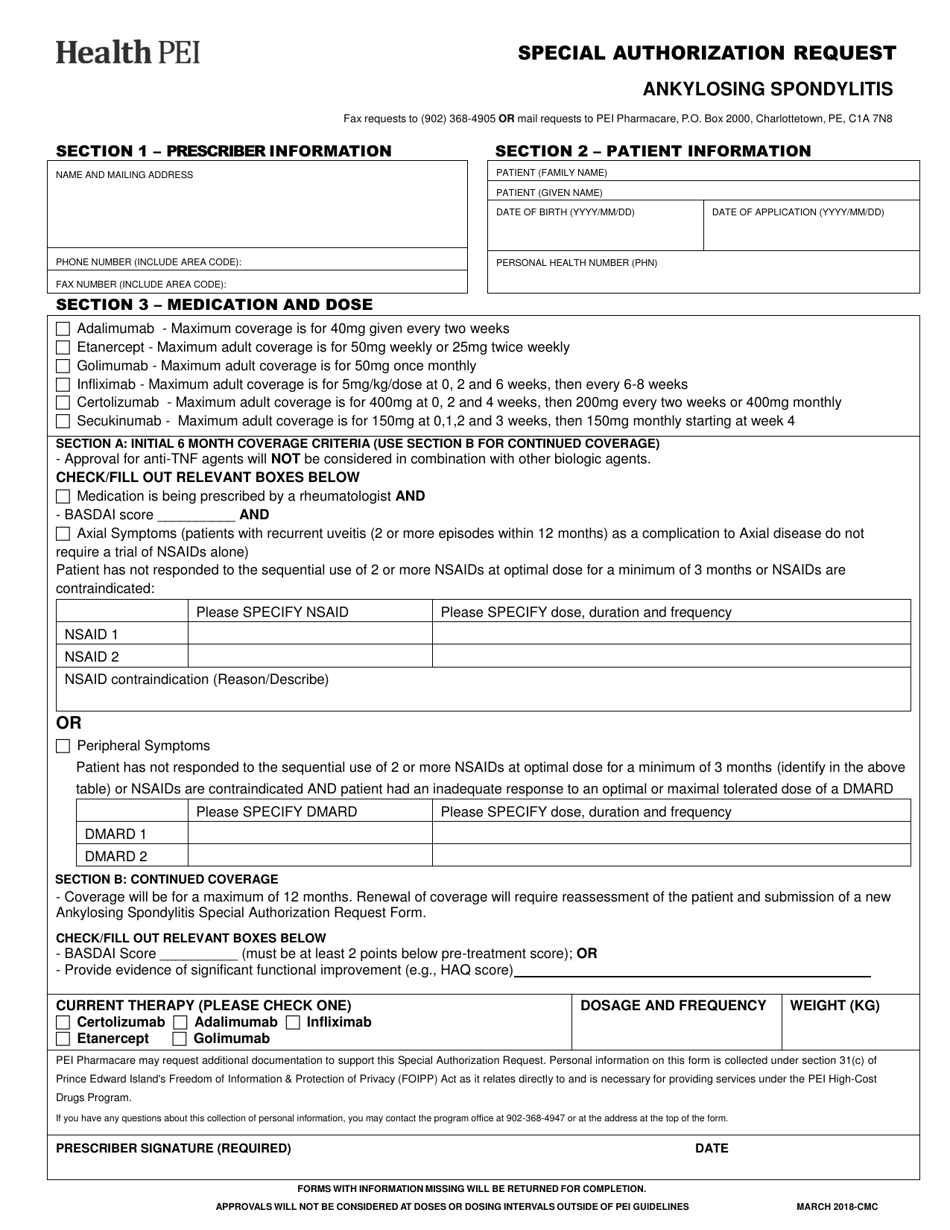
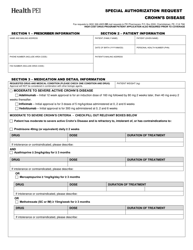
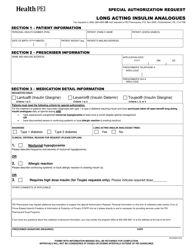
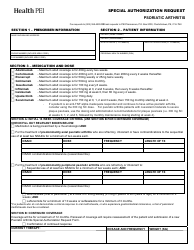
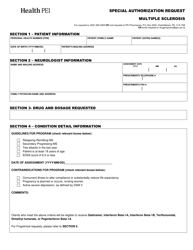
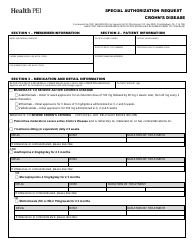
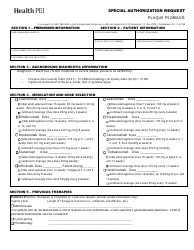
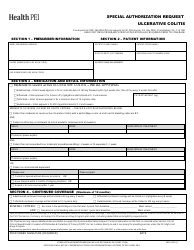
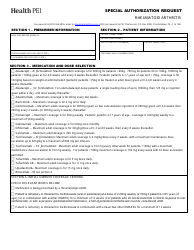
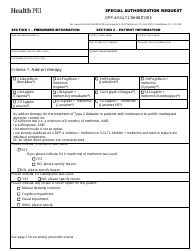
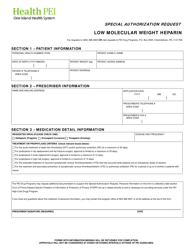
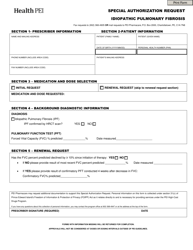
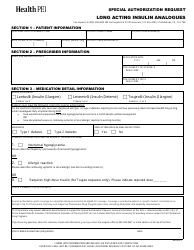
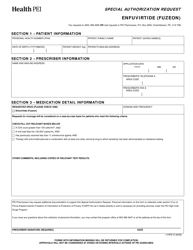
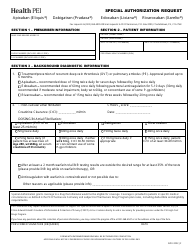
Ankylosing Spondylitis Special Authorization Request - Prince Edward Island, Canada
Ankylosing Spondylitis Special Authorization Request in Prince Edward Island, Canada is a document used for requesting special authorization for the treatment of Ankylosing Spondylitis, a type of arthritis that mainly affects the spine. It is used to obtain approval for specific medications or therapies that may be necessary for managing this condition.
The Ankylosing Spondylitis Special Authorization Request in Prince Edward Island, Canada is filed by the prescribing healthcare provider.
FAQ
Q: What is Ankylosing Spondylitis?
A: Ankylosing Spondylitis is a type of arthritis that primarily affects the spine.
Q: What is a Special Authorization Request?
A: A Special Authorization Request is a process where healthcare providers can request coverage for medications or treatments that may not be covered under the regular drug benefit program.
Q: Why would someone need a Special Authorization for Ankylosing Spondylitis?
A: Someone may need a Special Authorization for Ankylosing Spondylitis if their healthcare provider believes that a specific medication or treatment is necessary for their condition, but it is not normally covered under the regular drug benefit program.
Q: How can I apply for a Special Authorization Request for Ankylosing Spondylitis in Prince Edward Island?
A: To apply for a Special Authorization Request for Ankylosing Spondylitis in Prince Edward Island, you will need to work with your healthcare provider who will complete the necessary forms and submit them to the appropriate authority.
Q: Is there a specific form for the Special Authorization Request?
A: Yes, there is a specific form for the Special Authorization Request for Ankylosing Spondylitis in Prince Edward Island. Your healthcare provider will have access to this form and will help you complete it.
Q: What information is required for the Special Authorization Request?
A: The Special Authorization Request form will typically require information such as your personal details, medical history, medication/treatment information, and supporting documentation from your healthcare provider.
Q: How long does the Special Authorization Request process take?
A: The length of time for the Special Authorization Request process can vary. It may take a few days to several weeks to receive a decision.
Q: What happens if my Special Authorization Request is approved?
A: If your Special Authorization Request is approved, you may be eligible to receive the requested medication or treatment with coverage from the drug benefit program.
Q: What happens if my Special Authorization Request is denied?
A: If your Special Authorization Request is denied, you may need to discuss alternative treatment options with your healthcare provider or consider other sources of funding for the requested medication or treatment.
Q: Can I appeal a denial of a Special Authorization Request?
A: Yes, it is possible to appeal a denial of a Special Authorization Request. You should consult with your healthcare provider or contact the appropriate authority for more information on the appeal process.