This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
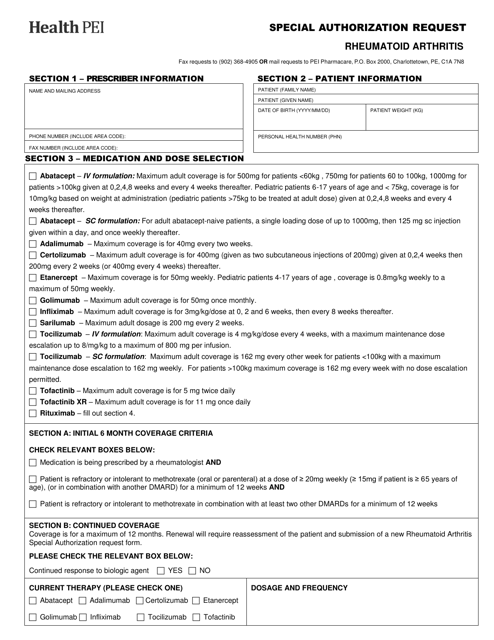
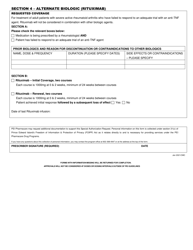
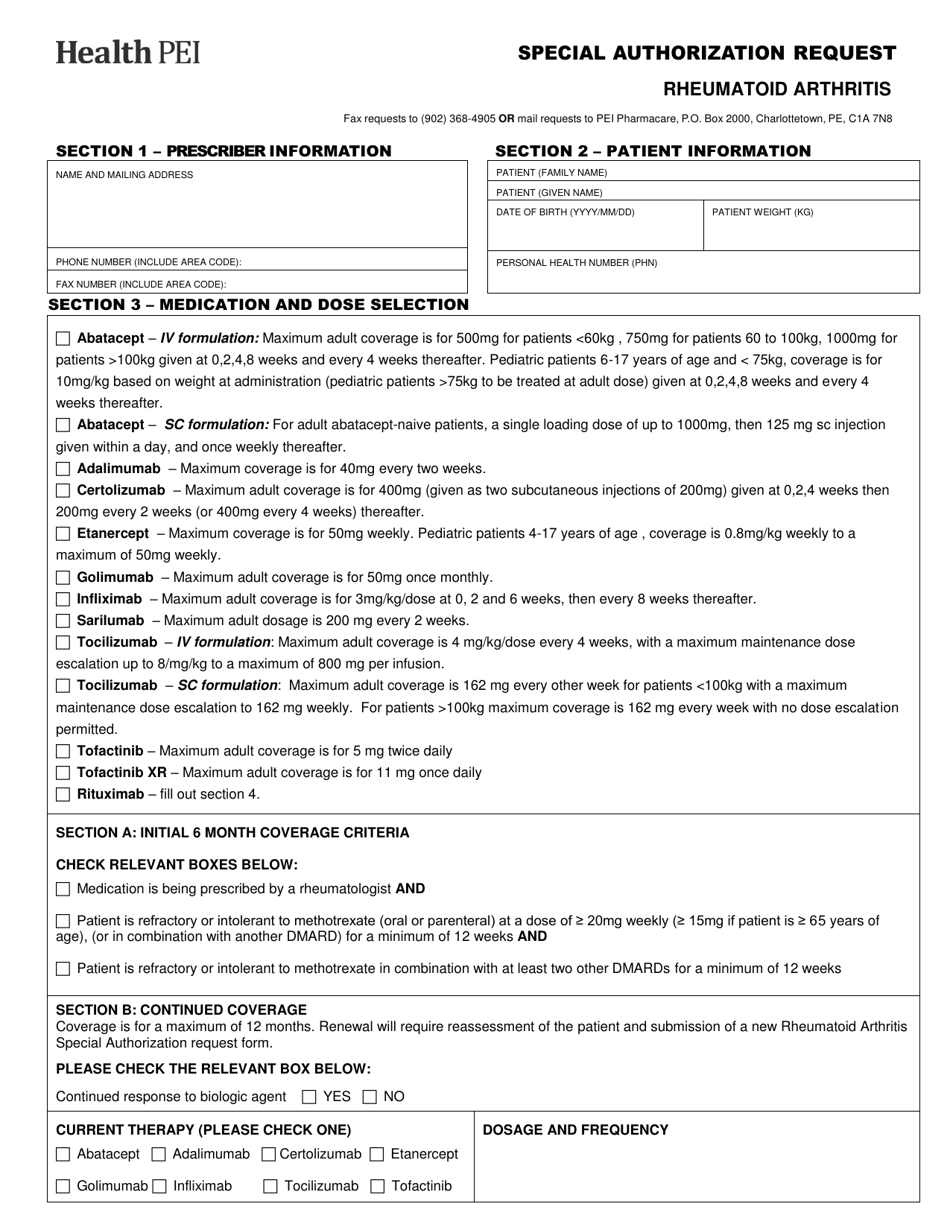
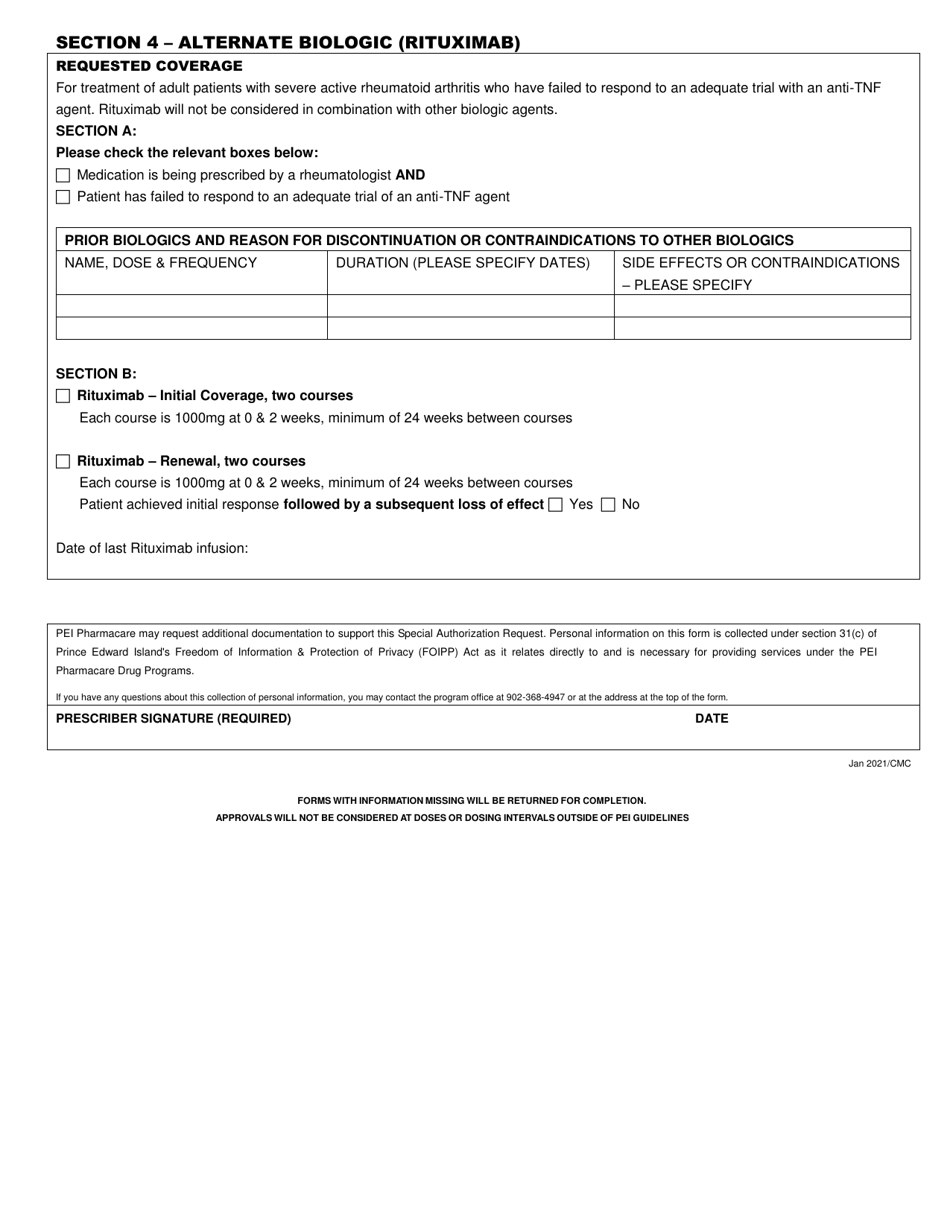
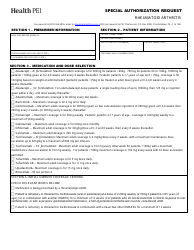
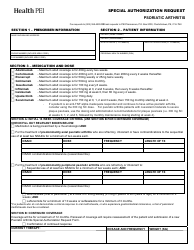
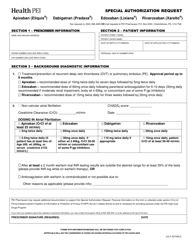
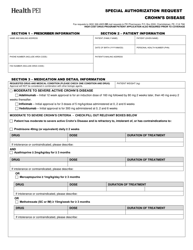
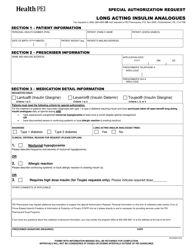
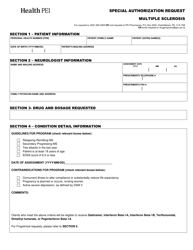
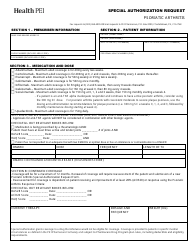
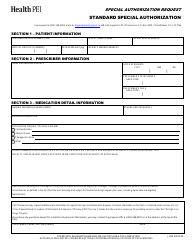
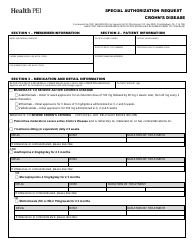
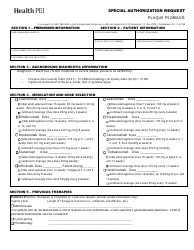
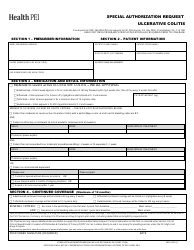
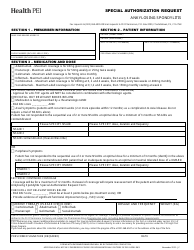
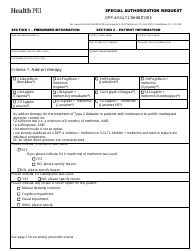
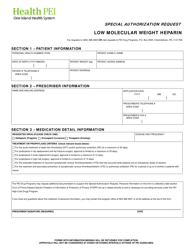
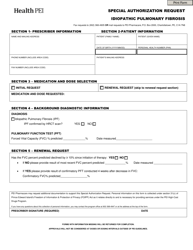
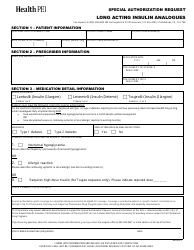
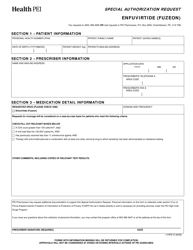
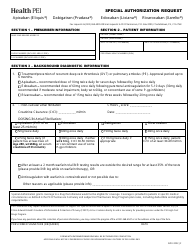
Special Authorization Request - Rheumatoid Arthritis - Prince Edward Island, Canada
The Special Authorization Request for Rheumatoid Arthritis in Prince Edward Island, Canada is a process to request approval for specific medications or treatments for individuals with Rheumatoid Arthritis. It allows healthcare providers to seek coverage for medications that may not be on the standard formulary or require additional approval.
The Special AuthorizationRequest for Rheumatoid Arthritis in Prince Edward Island, Canada is filed by the attending physician or rheumatologist.
FAQ
Q: What is a Special Authorization Request?
A: A Special Authorization Request is a formal request made by a healthcare provider to the government or the insurance company for coverage of a specific medication or treatment that is not automatically covered.
Q: What is Rheumatoid Arthritis?
A: Rheumatoid Arthritis is a chronic autoimmune disease that causes inflammation and pain in the joints.
Q: How can a Special Authorization Request help someone with Rheumatoid Arthritis in Prince Edward Island?
A: A Special Authorization Request can help someone with Rheumatoid Arthritis in Prince Edward Island by requesting the coverage of specific medications or treatments that may be necessary for their condition.
Q: Who can make a Special Authorization Request?
A: A healthcare provider, such as a doctor or nurse practitioner, can make a Special Authorization Request on behalf of their patient.
Q: What information is usually required in a Special Authorization Request?
A: A Special Authorization Request typically requires documentation from the healthcare provider, such as medical records and supporting evidence, to justify the need for the requested medication or treatment.
Q: How long does it take for a Special Authorization Request to be processed?
A: The processing time for a Special Authorization Request can vary, but it typically takes several weeks to be reviewed and a decision to be made.
Q: What happens if a Special Authorization Request is approved?
A: If a Special Authorization Request is approved, the requested medication or treatment will be covered by the government or insurance company.
Q: What happens if a Special Authorization Request is denied?
A: If a Special Authorization Request is denied, the healthcare provider and patient may need to explore alternative options, such as appealing the decision or considering different medications or treatments.
Q: Is there a fee for submitting a Special Authorization Request?
A: There is usually no fee for submitting a Special Authorization Request, but it is best to check with the specific government or insurance provider for any applicable fees or requirements.