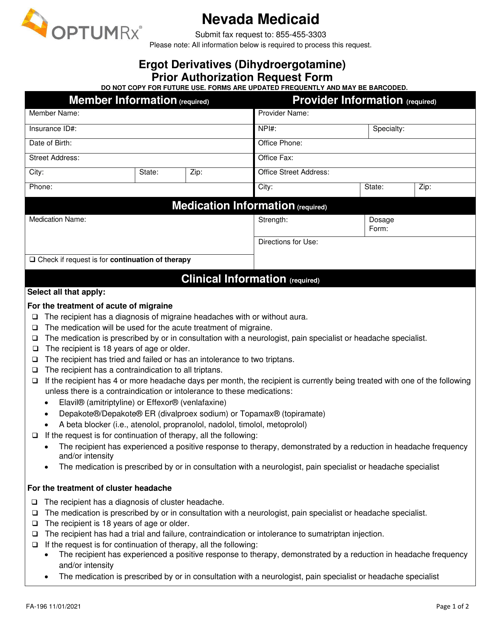
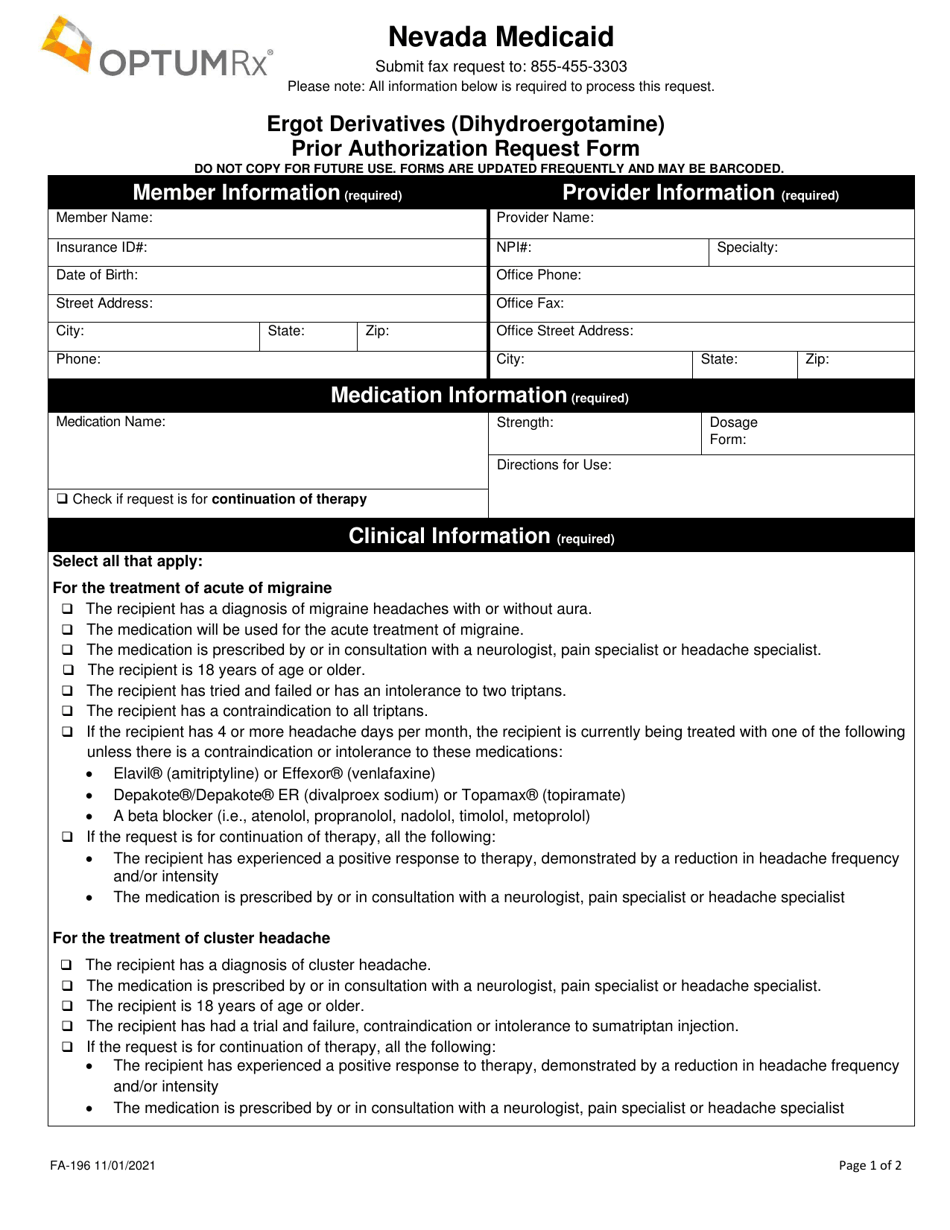
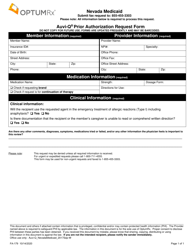
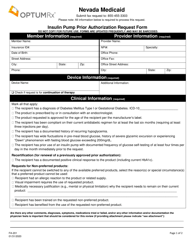
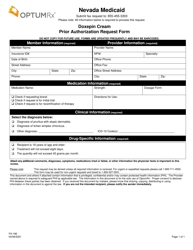
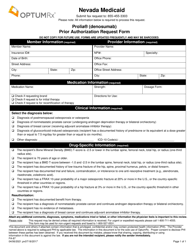
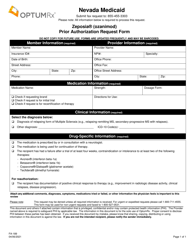
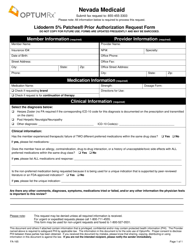
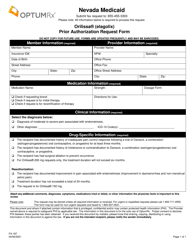
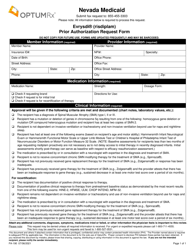
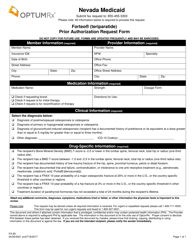
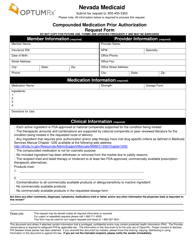
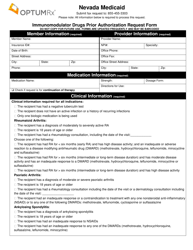
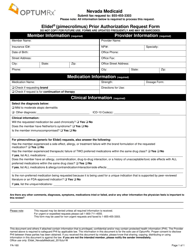
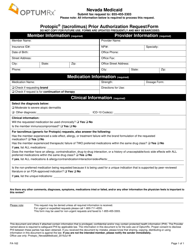
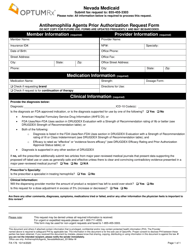
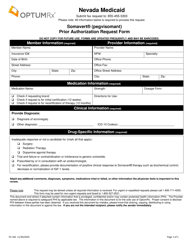
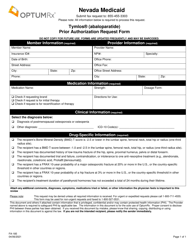
Form FA-196 Ergot Derivatives (Dihydroergotamine) Prior Authorization Request Form - Nevada
What Is Form FA-196?
This is a legal form that was released by the Nevada Department of Health and Human Services - a government authority operating within Nevada. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form FA-196?
A: Form FA-196 is a Prior Authorization Request Form specific to Nevada.
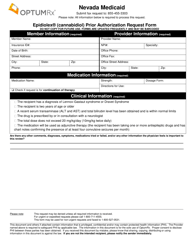
Q: What are Ergot Derivatives?
A: Ergot Derivatives are medications that contain dihydroergotamine, which is used to treat migraines.
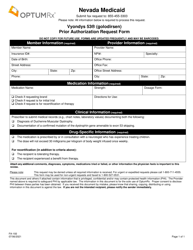
Q: What is Prior Authorization?
A: Prior Authorization is a process where the insurance company must approve certain medications before they will cover the cost.
Q: Why do I need to fill out Form FA-196?
A: You need to fill out Form FA-196 to request prior authorization for dihydroergotamine in Nevada.
Q: Can I use this form in other states?
A: No, this form is specific to Nevada.
Q: Who should complete this form?
A: This form should be completed by the prescribing healthcare provider.
Q: What information is required on Form FA-196?
A: The form requires information such as patient details, medical diagnosis, medication information, and supporting documentation.
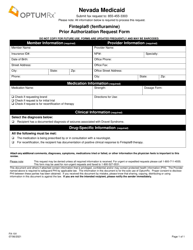
Q: How long does the prior authorization process take?
A: The length of time for the prior authorization process may vary, but typically within a few days.
Q: Do I need to renew the prior authorization?
A: Yes, prior authorizations usually have an expiration date, so you may need to renew it after a certain period of time.
Form Details:
- Released on November 1, 2021;
- The latest edition provided by the Nevada Department of Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of Form FA-196 by clicking the link below or browse more documents and templates provided by the Nevada Department of Health and Human Services.