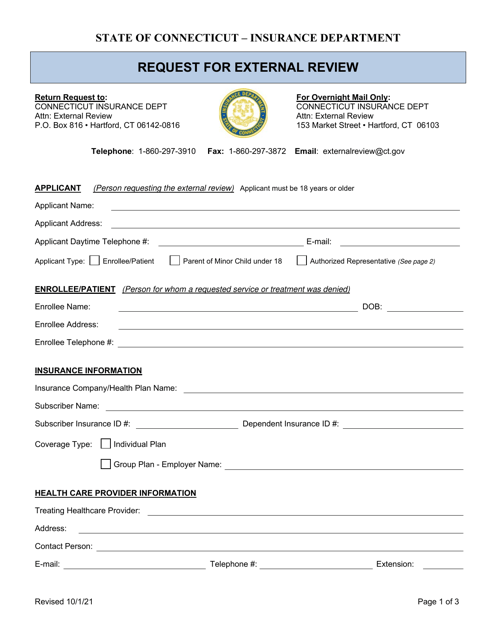
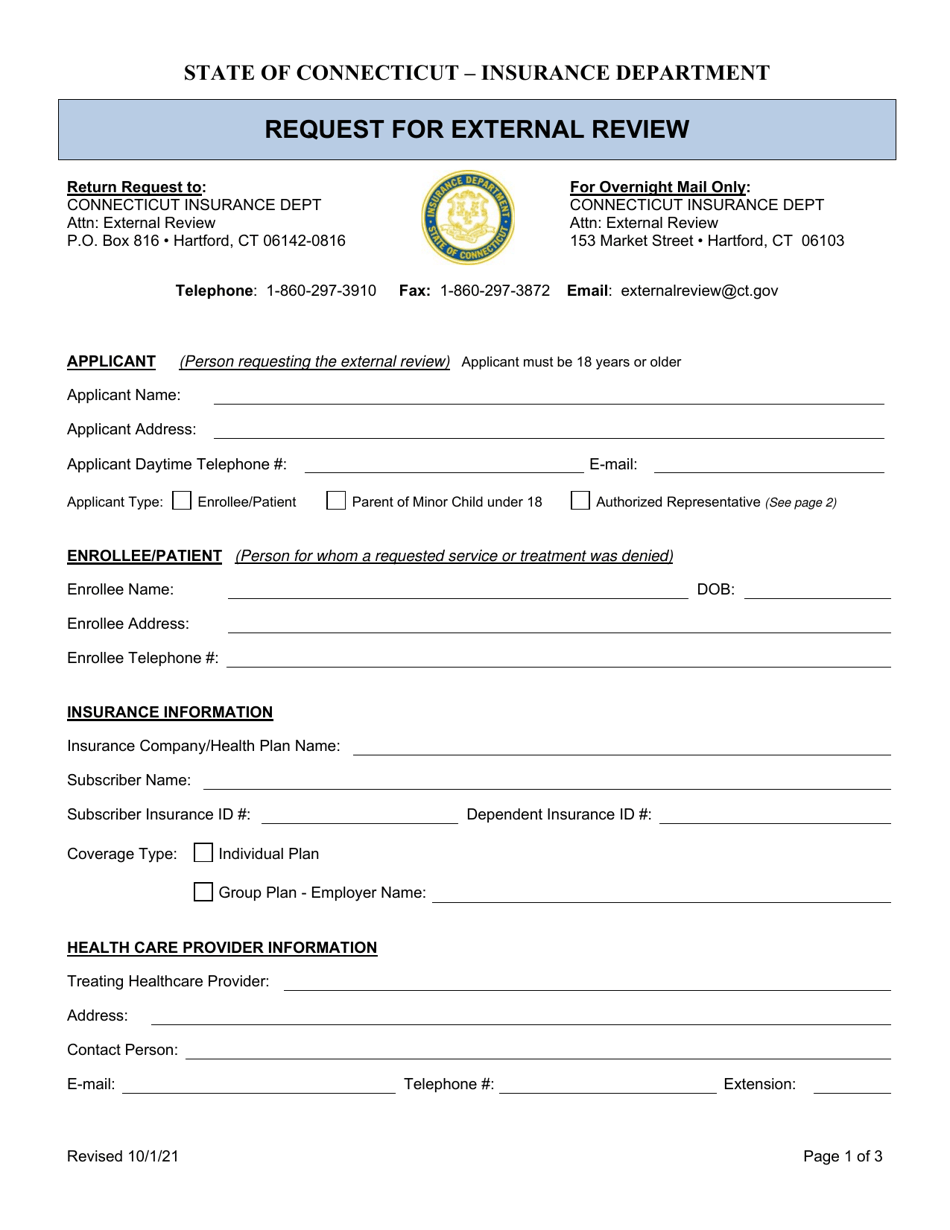
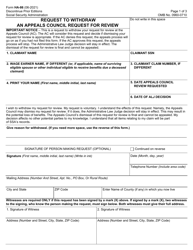
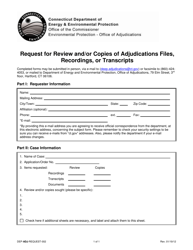
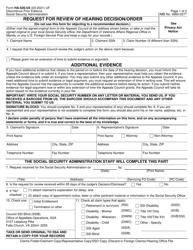
Request for External Review - Connecticut
Request for External Review is a legal document that was released by the Connecticut Insurance Department - a government authority operating within Connecticut.
FAQ
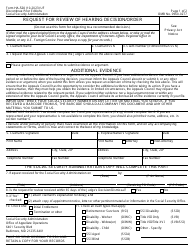
Q: What is the Request forExternal Review in Connecticut?
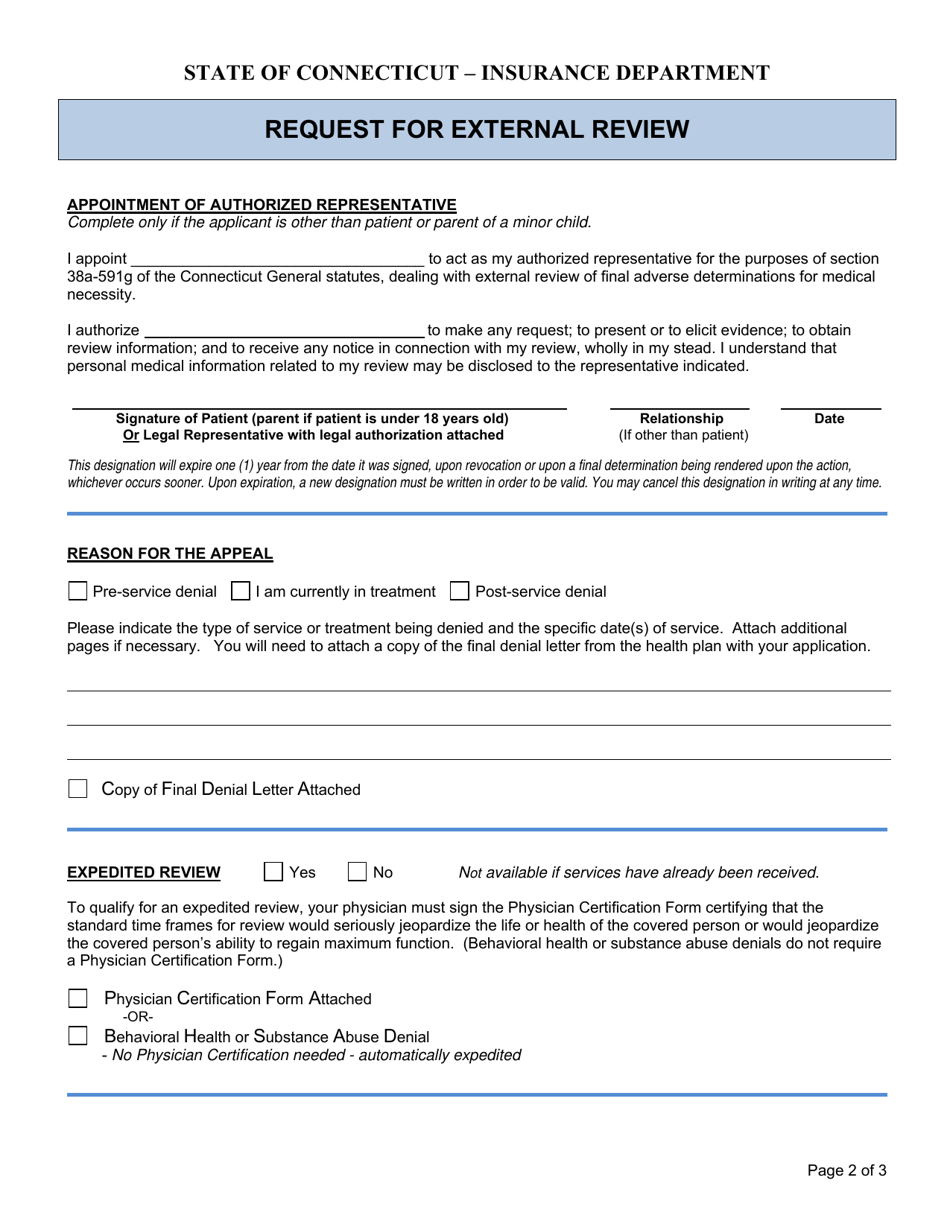
A: The Request for External Review is a process in Connecticut where individuals can request an independent review of certain denied health insurance claims.
Q: Who can submit a Request for External Review in Connecticut?
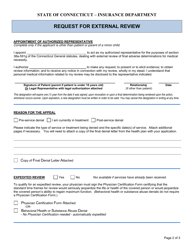
A: Any individual who has had a health insurance claim denied and has exhausted the internal appeals process can submit a Request for External Review in Connecticut.
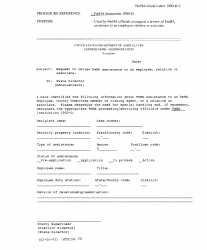
Q: What is the purpose of the External Review in Connecticut?
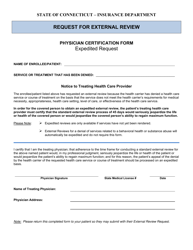
A: The purpose of the External Review is to provide an independent evaluation of denied health insurance claims and ensure that individuals receive a fair and impartial decision.
Q: What types of claims can be reviewed through the External Review process in Connecticut?
A: The External Review process in Connecticut can review claims related to medical necessity, experimental or investigational treatment, and the appropriateness of care.
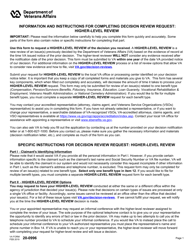
Q: Is there a fee to submit a Request for External Review in Connecticut?
A: No, there is no fee to submit a Request for External Review in Connecticut.
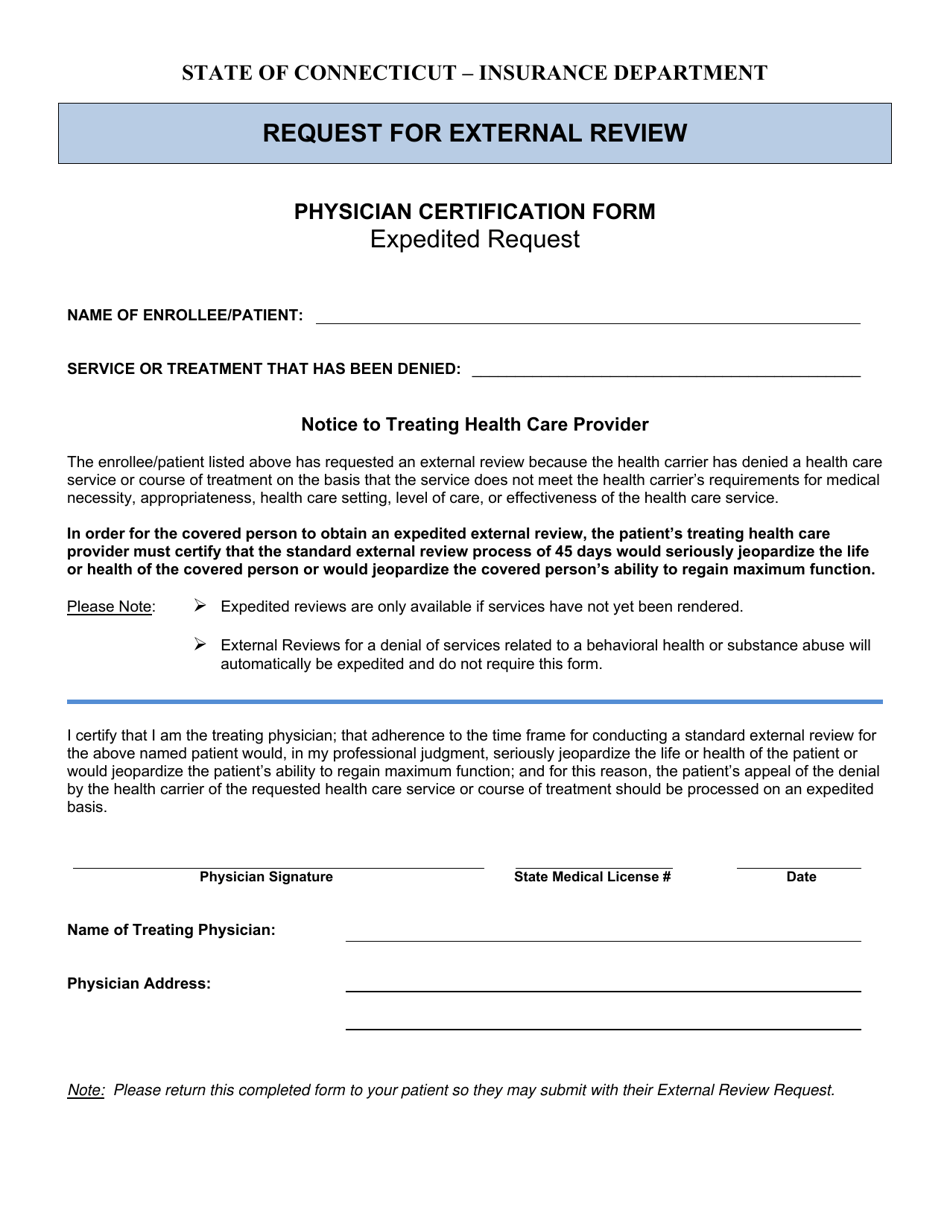
Q: How long does the External Review process in Connecticut take?
A: The External Review process in Connecticut typically takes 30 days for urgent requests and 45 days for standard requests.
Form Details:
- Released on October 1, 2021;
- The latest edition currently provided by the Connecticut Insurance Department;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Connecticut Insurance Department.