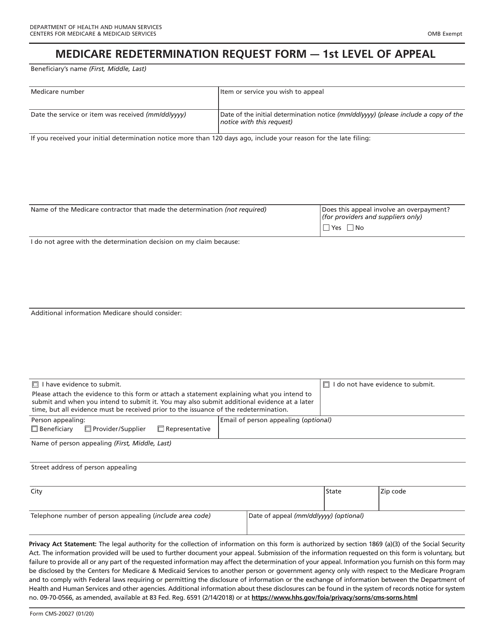
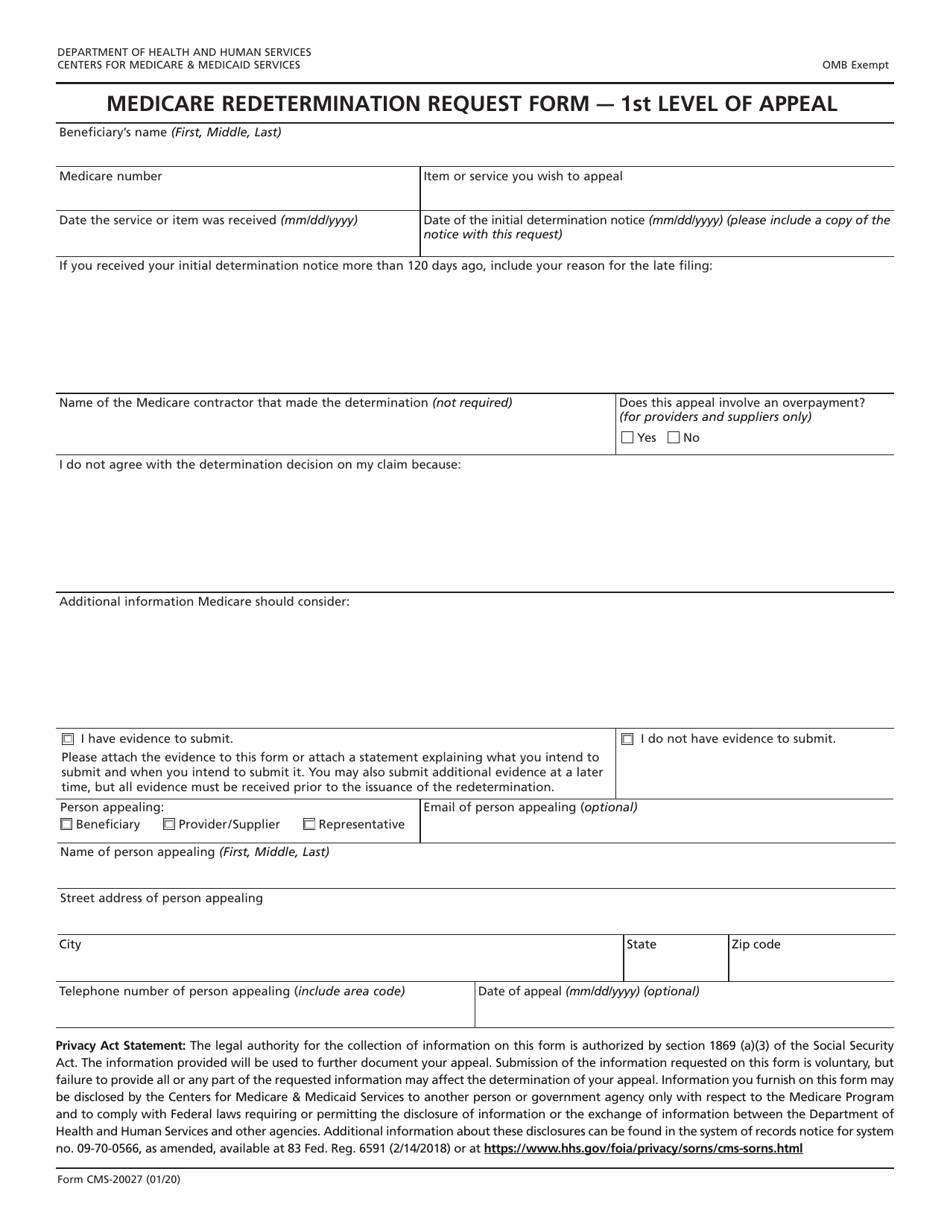
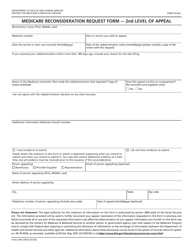
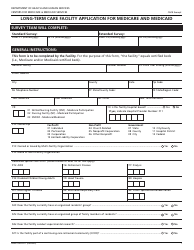
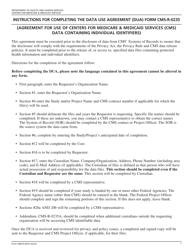
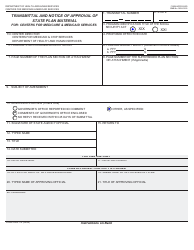
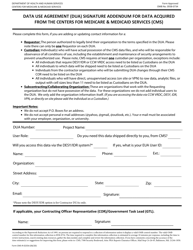
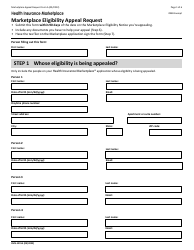
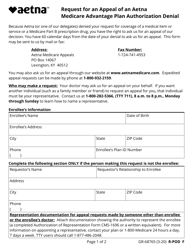
Form CMS-20027 Medicare Redetermination Request Form - 1st Level of Appeal
What Is Form CMS-20027?
This is a legal form that was released by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services on January 1, 2020 and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form CMS-20027?
A: Form CMS-20027 is the Medicare Redetermination Request Form for the 1st Level of Appeal.
Q: What is the purpose of Form CMS-20027?
A: The purpose of Form CMS-20027 is to request a redetermination for denied Medicare claims.
Q: Who can use Form CMS-20027?
A: Medicare beneficiaries or their authorized representatives can use Form CMS-20027.
Q: What is a redetermination?
A: Redetermination is the first level of appeal for denied Medicare claims.
Q: How do I submit Form CMS-20027?
A: Form CMS-20027 can be submitted by mail or fax to the Medicare Administrative Contractor (MAC) listed on the denial notice.
Q: What information do I need to include on Form CMS-20027?
A: You need to include your name, Medicare number, date of service, reason for the appeal, and any supporting documentation.
Q: What is the deadline for submitting Form CMS-20027?
A: The deadline for submitting Form CMS-20027 is generally 120 days from the date of the initial denial.
Q: What happens after I submit Form CMS-20027?
A: After you submit Form CMS-20027, the MAC will review your request and make a determination.
Q: Can I appeal further if my redetermination request is denied?
A: Yes, if your redetermination request is denied, you can proceed to the second level of appeal, which is a reconsideration.
Form Details:
- Released on January 1, 2020;
- The latest available edition released by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form CMS-20027 by clicking the link below or browse more documents and templates provided by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services.