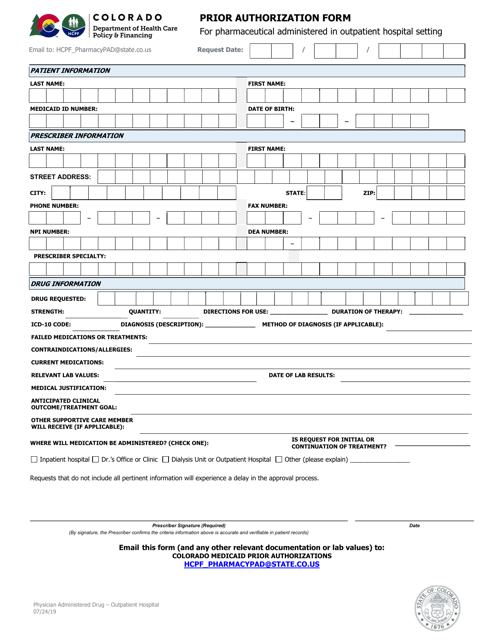
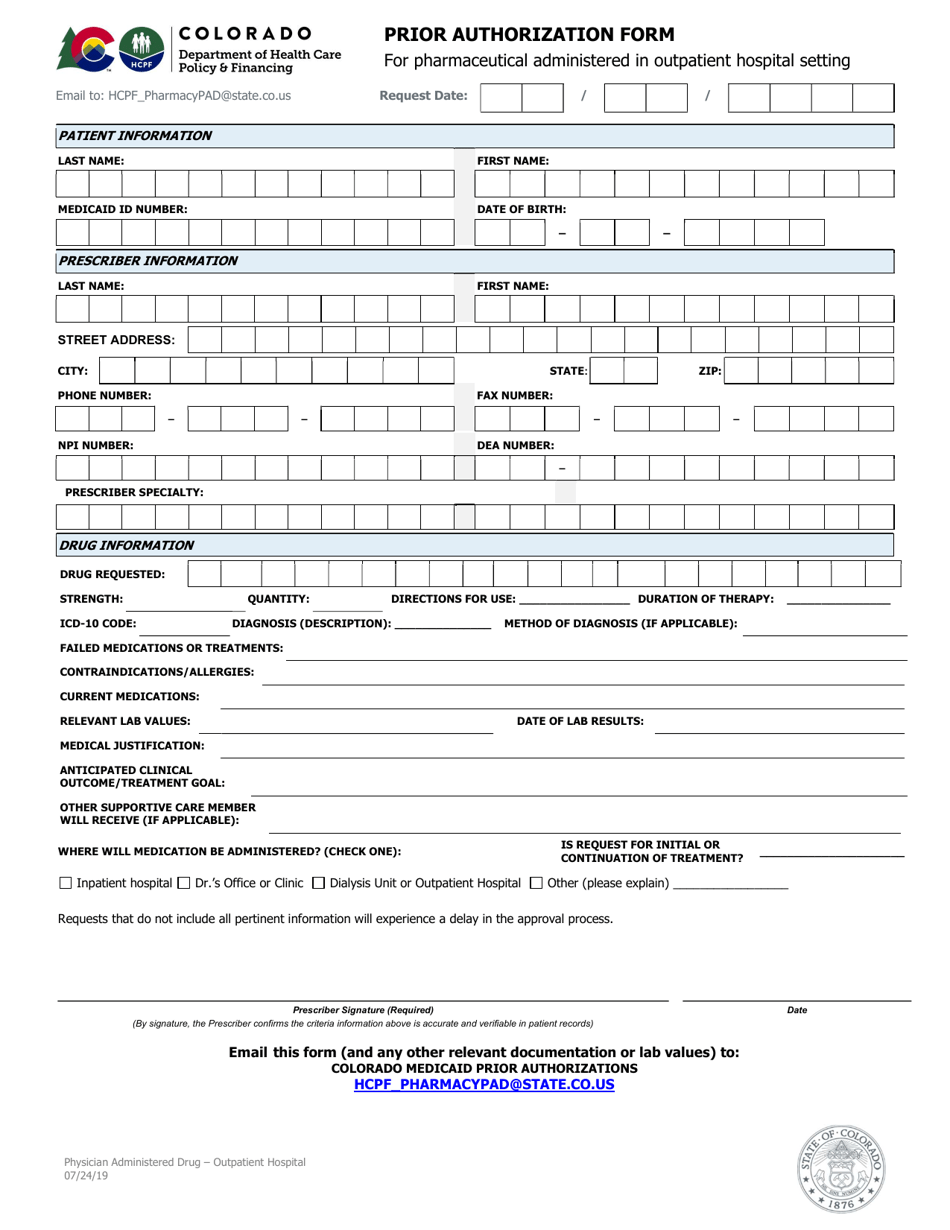
Prior Authorization Form for Pharmaceutical Administered in Outpatient Hospital Setting - Colorado
Prior Authorization Form for Pharmaceutical Administered in Outpatient Hospital Setting is a legal document that was released by the Colorado Department of Health Care Policy and Financing - a government authority operating within Colorado.
FAQ
Q: What is a prior authorization form?
A: A prior authorization form is a document that must be filled out by a healthcare provider to request approval from an insurance company to cover a specific medication or treatment.
Q: What is the purpose of a prior authorization form?
A: The purpose of a prior authorization form is to ensure that the requested medication or treatment meets the insurance company's criteria for coverage before it is administered.
Q: Who should fill out a prior authorization form?
A: A healthcare provider, such as a doctor or pharmacist, should fill out a prior authorization form.
Q: What is an outpatient hospital setting?
A: An outpatient hospital setting refers to a hospital or clinic where patients receive medical treatment without being admitted to the hospital overnight.
Q: Why might a prior authorization be required for pharmaceuticals administered in an outpatient hospital setting?
A: A prior authorization may be required to ensure that the medication being administered in the outpatient hospital setting is medically necessary and meets the insurance company's criteria for coverage.
Q: What information is typically included in a prior authorization form?
A: A prior authorization form typically includes information about the patient, the healthcare provider, the medication or treatment being requested, and any supporting documentation or rationale for the request.
Form Details:
- Released on July 24, 2019;
- The latest edition currently provided by the Colorado Department of Health Care Policy and Financing;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Colorado Department of Health Care Policy and Financing.