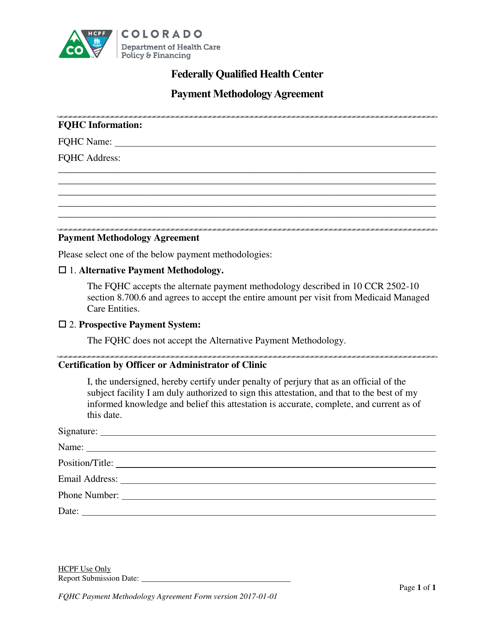
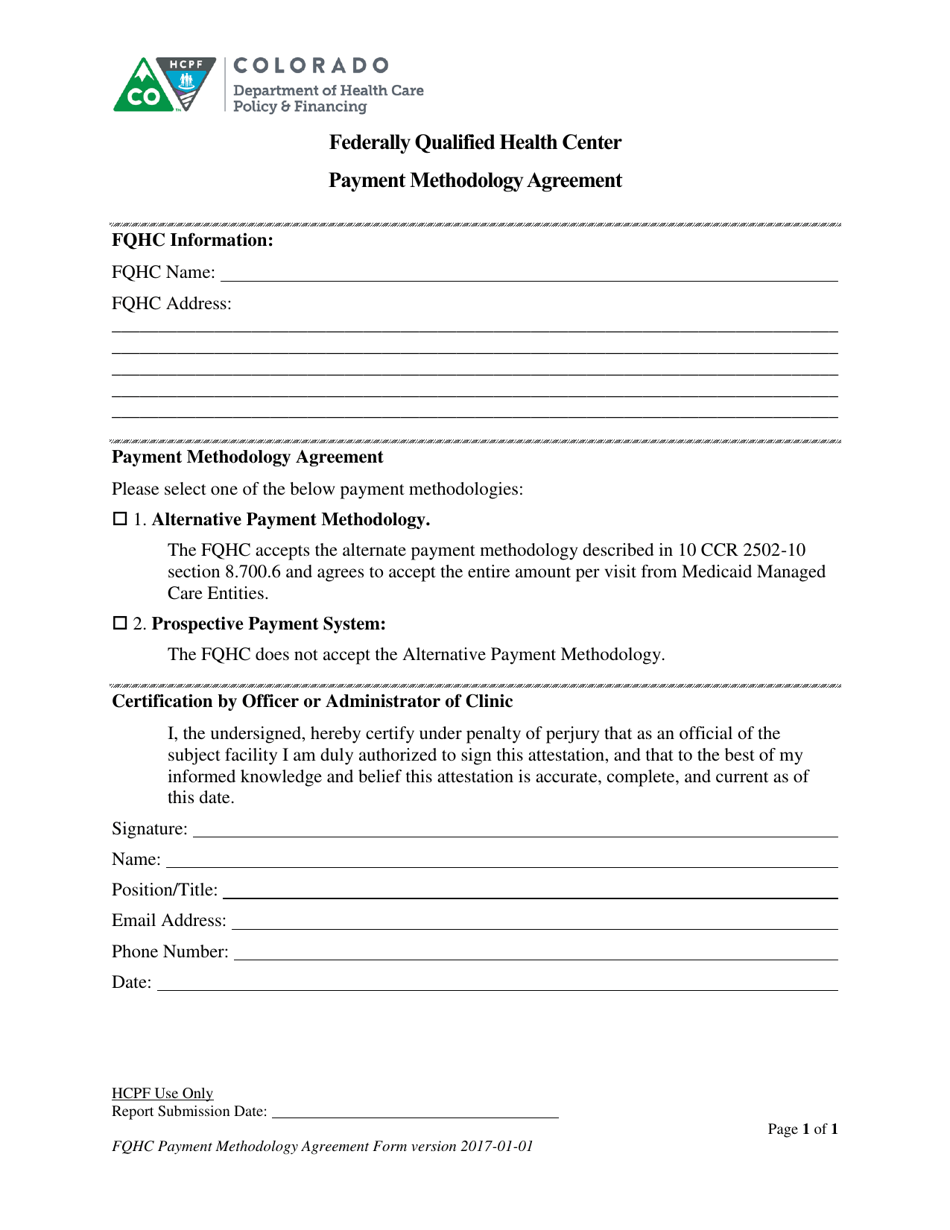
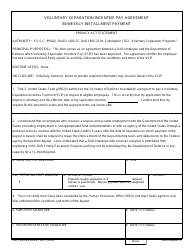
Payment Methodology Agreement - Federally Qualified Health Center - Colorado
Payment Methodology Agreement - Federally Qualified Health Center is a legal document that was released by the Colorado Department of Health Care Policy and Financing - a government authority operating within Colorado.
FAQ
Q: What is a Federally Qualified Health Center (FQHC)?
A: A Federally Qualified Health Center (FQHC) is a community-based healthcare provider that receives funding from the federal government to offer comprehensive primary care services to underserved populations.
Q: What is the purpose of a Payment Methodology Agreement?
A: The purpose of a Payment Methodology Agreement is to establish the payment terms and conditions between a Federally Qualified Health Center (FQHC) and the entity responsible for reimbursing the center for its services.
Q: Why is a Payment Methodology Agreement important for an FQHC?
A: A Payment Methodology Agreement is important for an FQHC because it ensures that the center receives proper reimbursement for the services it provides, and it helps maintain financial stability for the center.
Q: Who is involved in a Payment Methodology Agreement?
A: The entities involved in a Payment Methodology Agreement are the Federally Qualified Health Center (FQHC) and the organization responsible for reimbursing the center, such as a Medicaid agency or a managed care organization.
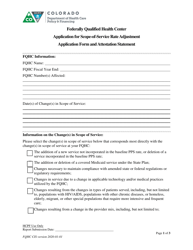
Q: What are the key components of a Payment Methodology Agreement?
A: The key components of a Payment Methodology Agreement typically include the reimbursement rates and methods, the scope of services covered, performance measures and reporting requirements, and dispute resolution procedures.
Q: How are reimbursement rates determined in a Payment Methodology Agreement?
A: Reimbursement rates in a Payment Methodology Agreement are typically determined based on factors such as the center's costs, the complexity of services provided, and the healthcare needs of the population served.
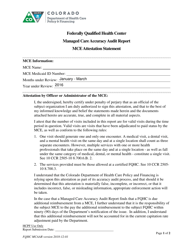
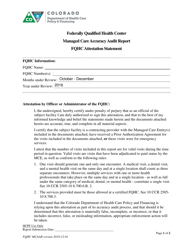
Q: What is the role of performance measures in a Payment Methodology Agreement?
A: Performance measures in a Payment Methodology Agreement help assess the quality and efficiency of services provided by the Federally Qualified Health Center (FQHC). They may include measures related to patient outcomes, access to care, and cost-effectiveness.
Q: What happens if there is a dispute between the parties in a Payment Methodology Agreement?
A: If there is a dispute between the parties in a Payment Methodology Agreement, there are typically procedures outlined in the agreement for resolving the dispute, such as mediation or arbitration.
Form Details:
- Released on January 1, 2017;
- The latest edition currently provided by the Colorado Department of Health Care Policy and Financing;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Colorado Department of Health Care Policy and Financing.