This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
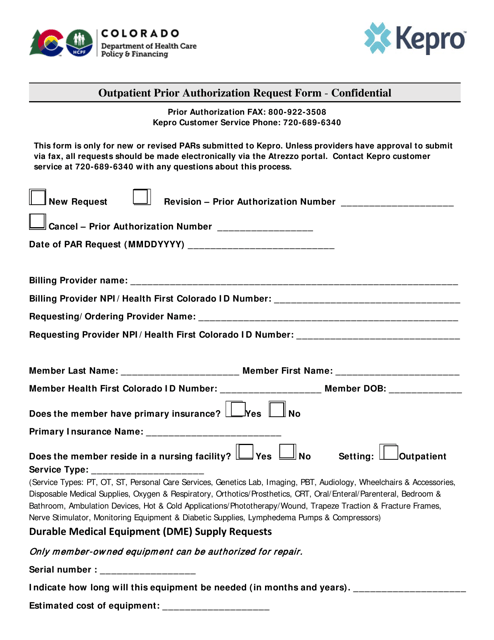
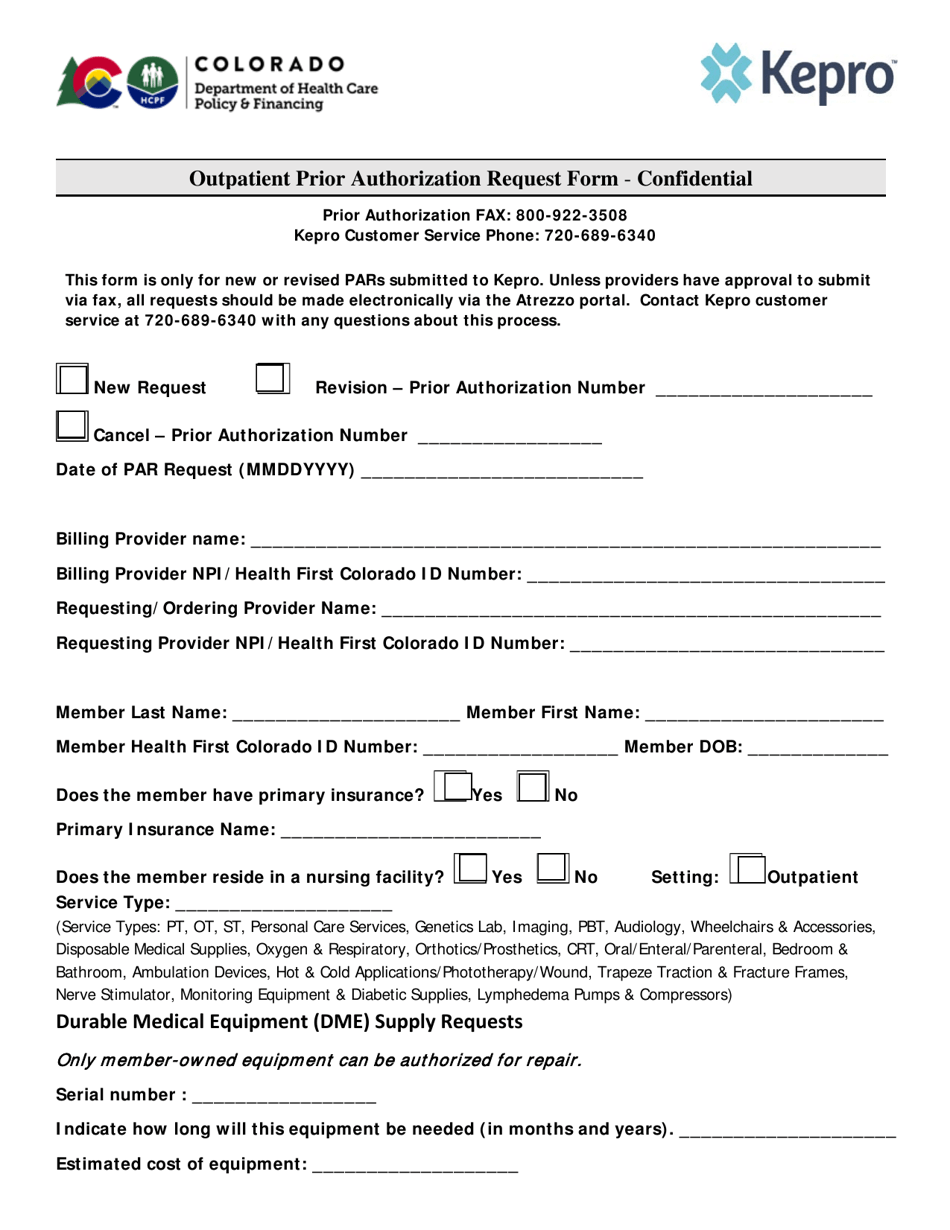
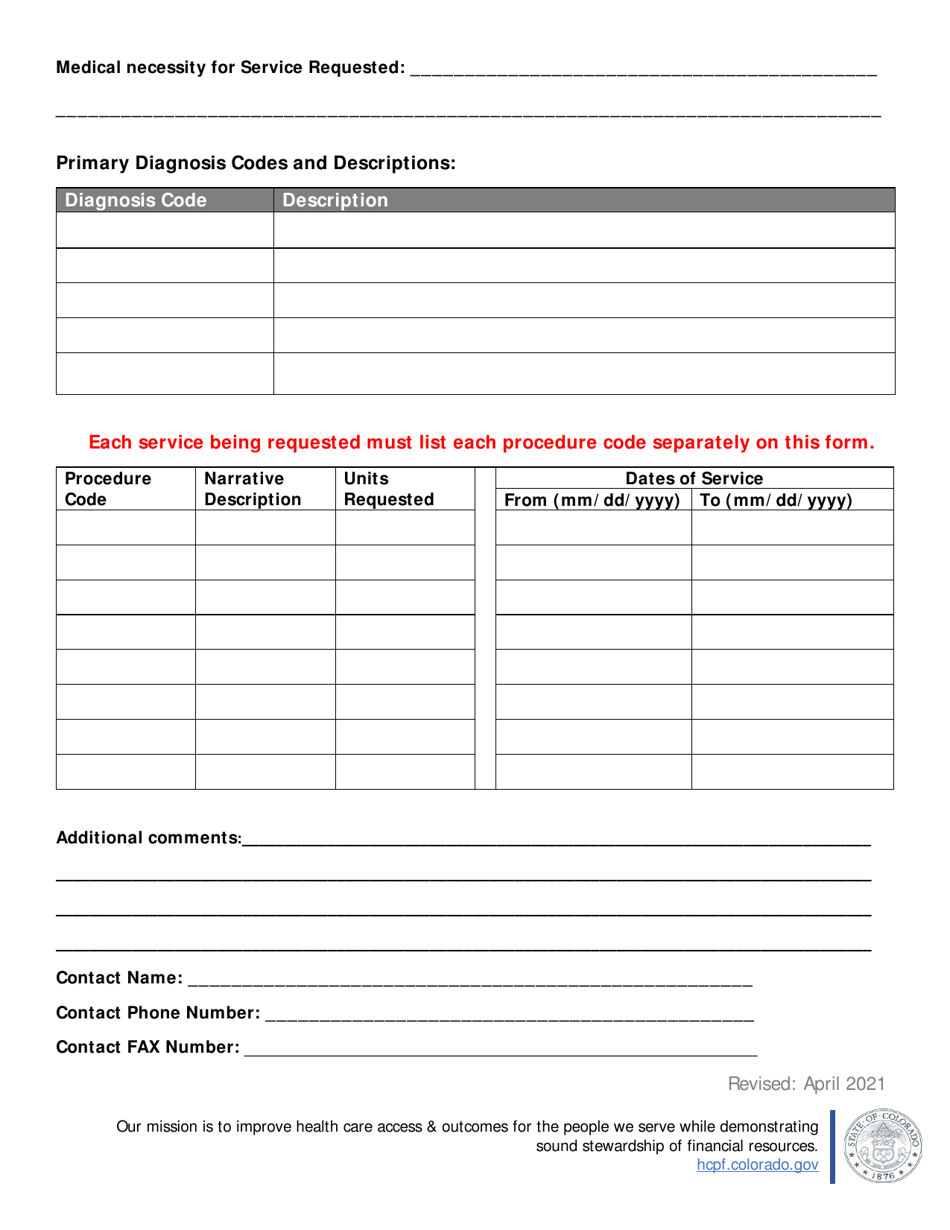
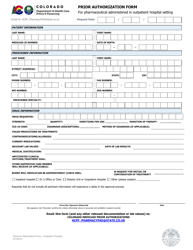
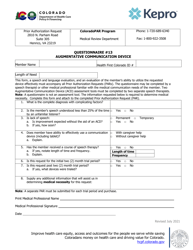
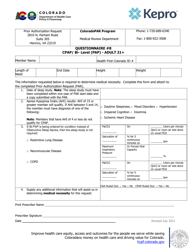
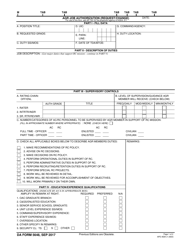
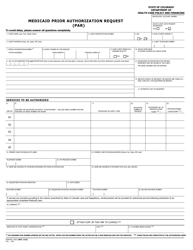
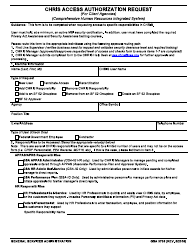
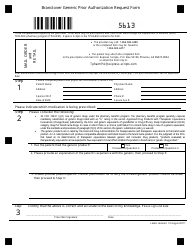
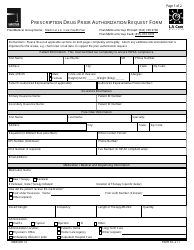
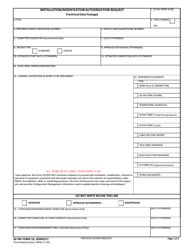
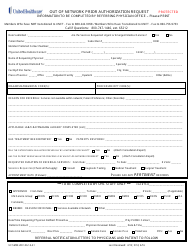
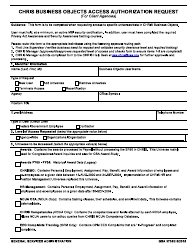
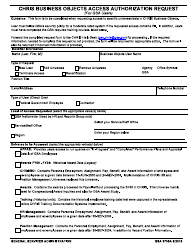
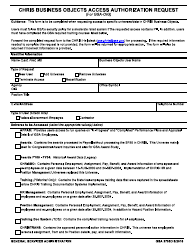
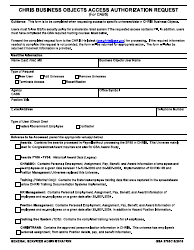
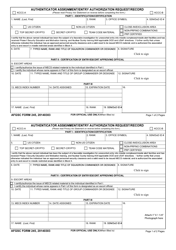
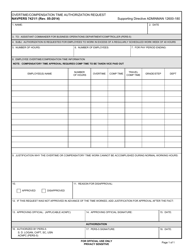
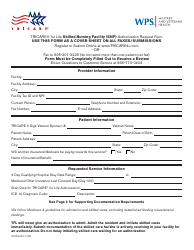
Outpatient Prior Authorization Request Form - Colorado
Outpatient Prior Authorization Request Form is a legal document that was released by the Colorado Department of Health Care Policy and Financing - a government authority operating within Colorado.
FAQ
Q: What is an outpatient prior authorization?
A: An outpatient prior authorization is a request for approval before receiving certain healthcare services or treatments.
Q: Why do I need to fill out a prior authorization form?
A: You need to fill out a prior authorization form to obtain approval from your insurance company before receiving outpatient services, as certain services may require prior authorization for coverage.
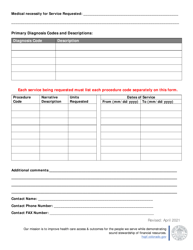
Q: What information is required on the outpatient prior authorization form?
A: The form will typically require details such as your personal information, insurance information, the requested services, and supporting documentation from your healthcare provider.
Q: How do I submit the outpatient prior authorization request form?
A: You can submit the form directly to your insurance company either through mail, fax, or electronically, as specified by your insurer.
Q: How long does it take to receive a decision on the prior authorization request?
A: The timeframe for a decision varies depending on the insurance company, but it is typically within a few business days to a couple of weeks.
Q: What happens if my prior authorization request is denied?
A: If your request is denied, you may have the option to appeal the decision or explore other alternatives with your healthcare provider.
Q: Can I still receive the outpatient services if my prior authorization request is denied?
A: If your prior authorization request is denied, it may result in your insurance not covering the cost of the requested services, unless you are able to successfully appeal the decision.
Q: Are all outpatient services subject to prior authorization?
A: Not all outpatient services require prior authorization, but certain services, treatments, or procedures may have specific requirements for obtaining prior approval.
Q: What should I do if I have questions or need assistance with the outpatient prior authorization process?
A: If you have questions or need assistance, you should contact your insurance company's customer service department for guidance and support.
Form Details:
- Released on April 1, 2021;
- The latest edition currently provided by the Colorado Department of Health Care Policy and Financing;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Colorado Department of Health Care Policy and Financing.