This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
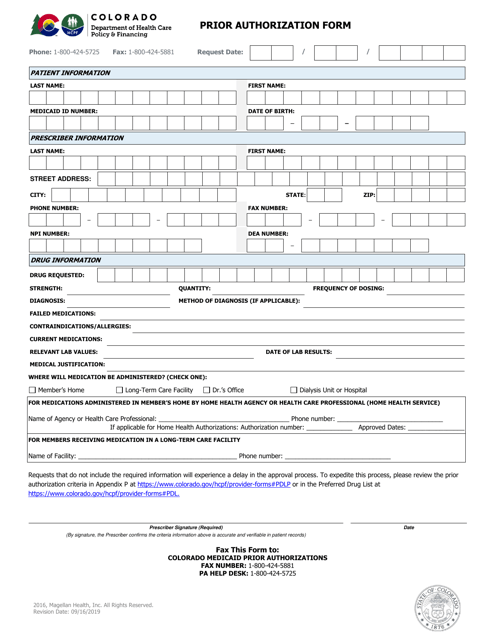
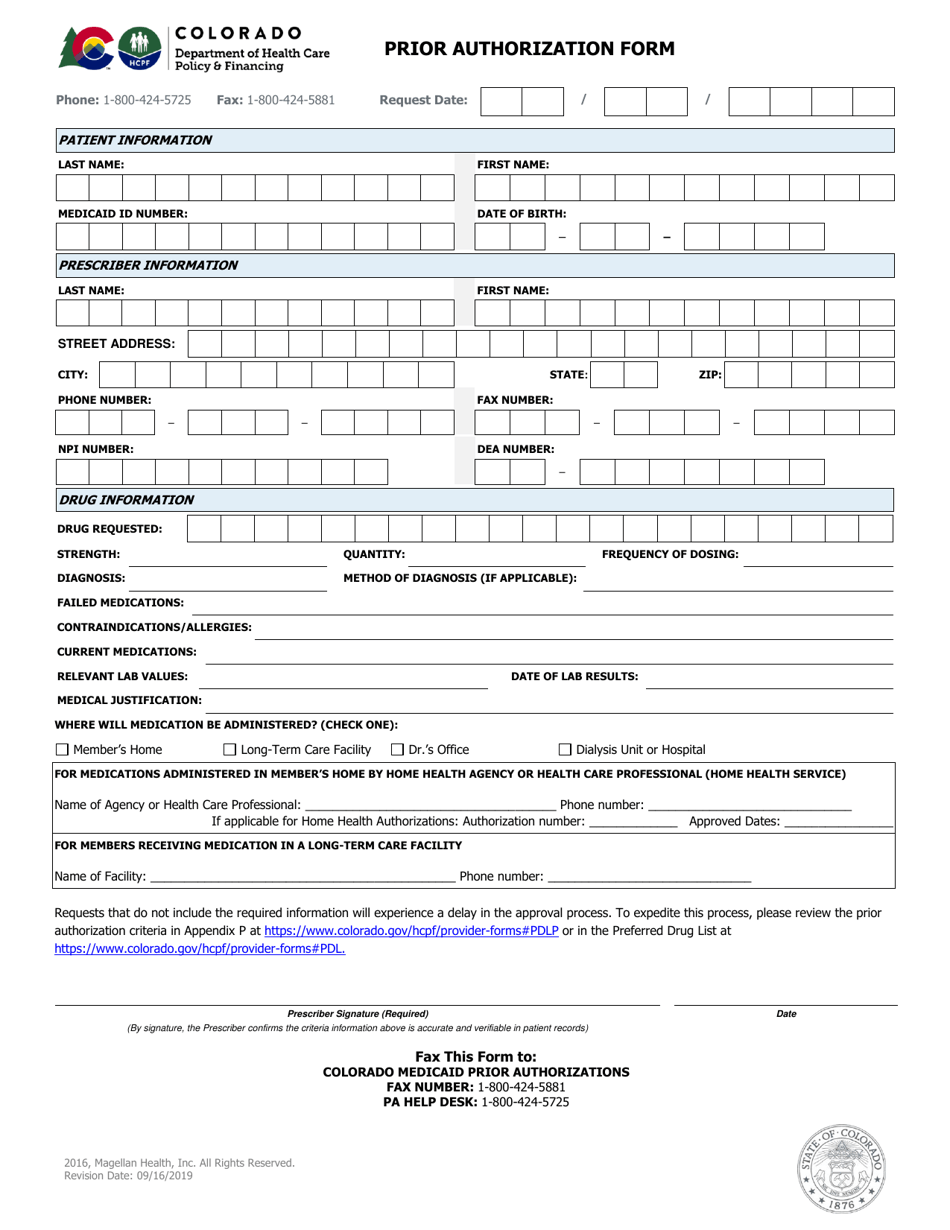
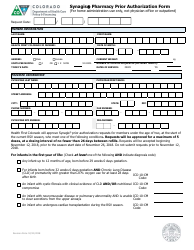
Pharmacy Prior Authorization Form - Colorado
Pharmacy Prior Authorization Form is a legal document that was released by the Colorado Department of Health Care Policy and Financing - a government authority operating within Colorado.
FAQ
Q: What is a Pharmacy Prior Authorization Form?
A: A Pharmacy Prior Authorization Form is a document that must be completed by a healthcare provider to request coverage for a specific medication.
Q: Why is a Pharmacy Prior Authorization Form necessary?
A: A Pharmacy Prior Authorization Form is necessary to ensure that the prescribed medication meets the criteria set by the insurance company for coverage.
Q: How can I obtain a Pharmacy Prior Authorization Form in Colorado?
A: You can obtain a Pharmacy Prior Authorization Form in Colorado by contacting your insurance company or healthcare provider.
Q: What information is required on the Pharmacy Prior Authorization Form?
A: The Pharmacy Prior Authorization Form typically requires information such as the patient's name, insurance information, prescribing healthcare provider's information, and details about the medication being requested.
Q: What happens after the Pharmacy Prior Authorization Form is submitted?
A: After the Pharmacy Prior Authorization Form is submitted, the insurance company will review the form and make a decision regarding coverage. They may request additional information or contact the healthcare provider for clarification.
Q: How long does it take to receive a decision on a Pharmacy Prior Authorization Form?
A: The time it takes to receive a decision on a Pharmacy Prior Authorization Form can vary. It may take anywhere from a few days to a few weeks.
Q: What if the Pharmacy Prior Authorization Form is denied?
A: If the Pharmacy Prior Authorization Form is denied, the healthcare provider can appeal the decision or explore other medication options with the patient.
Q: Are there any fees associated with submitting a Pharmacy Prior Authorization Form?
A: There are typically no fees associated with submitting a Pharmacy Prior Authorization Form.
Q: Can a Pharmacy Prior Authorization Form be faxed?
A: Yes, Pharmacy Prior Authorization Forms can often be faxed to the appropriate department at the insurance company.
Form Details:
- Released on September 16, 2019;
- The latest edition currently provided by the Colorado Department of Health Care Policy and Financing;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Colorado Department of Health Care Policy and Financing.