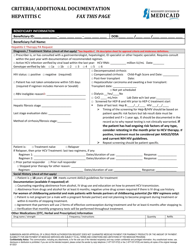
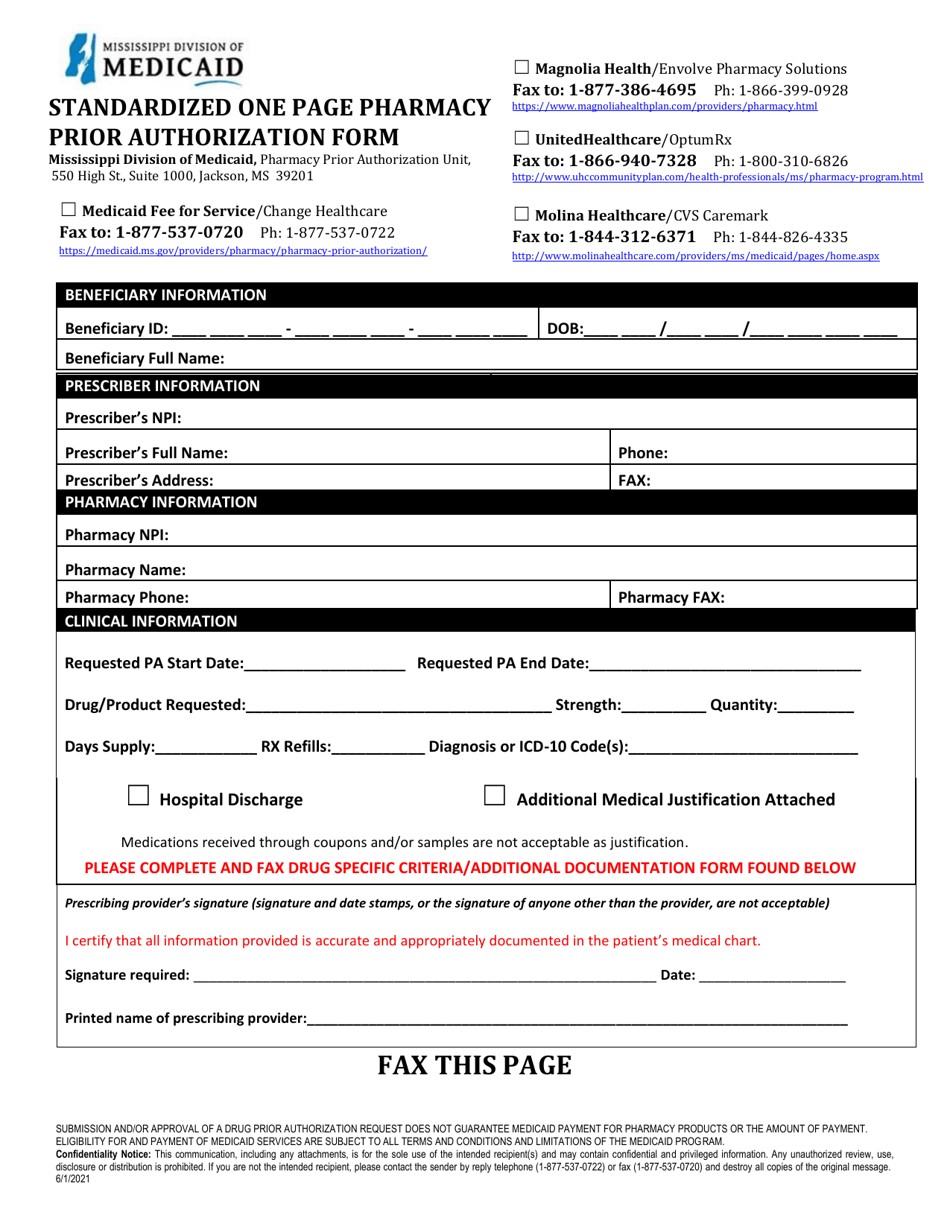
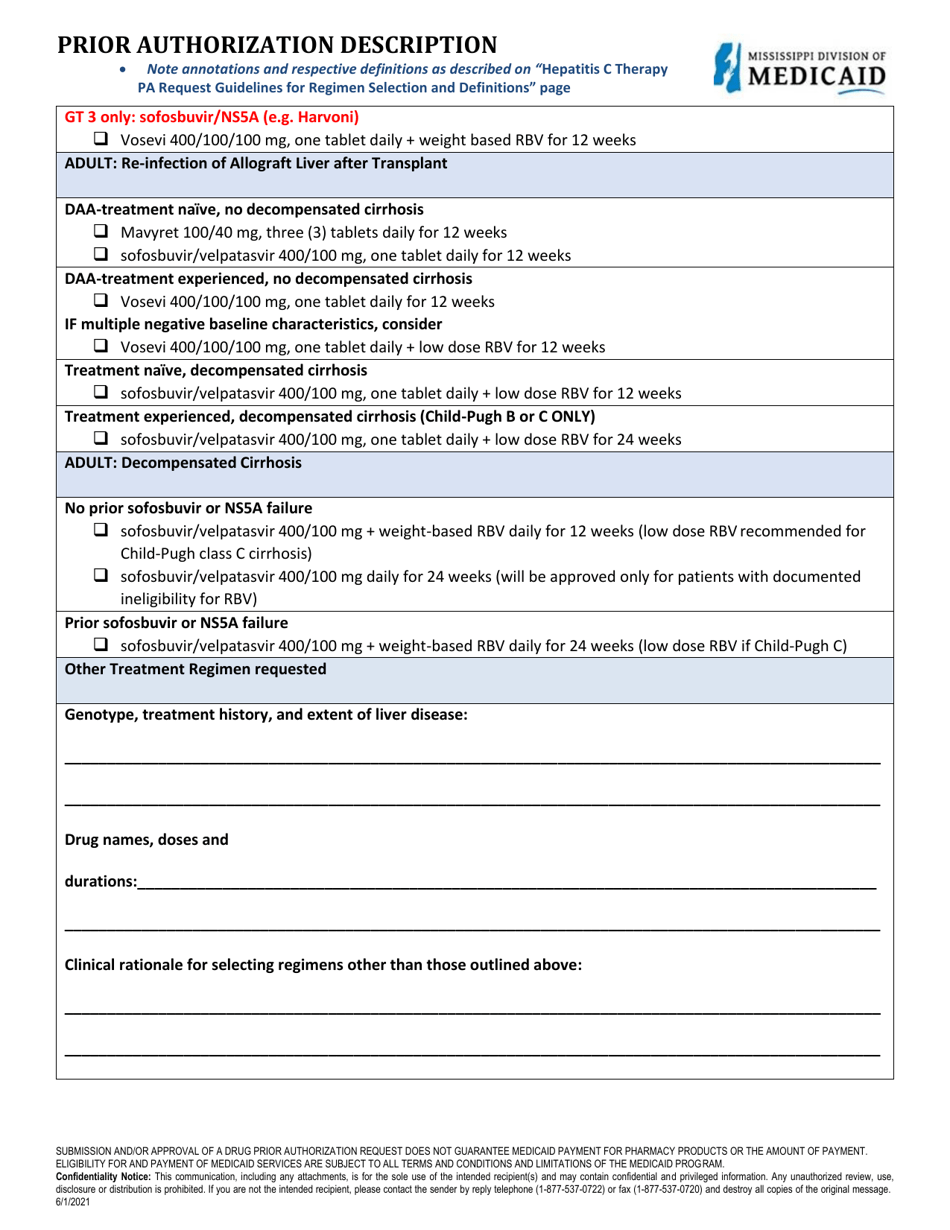
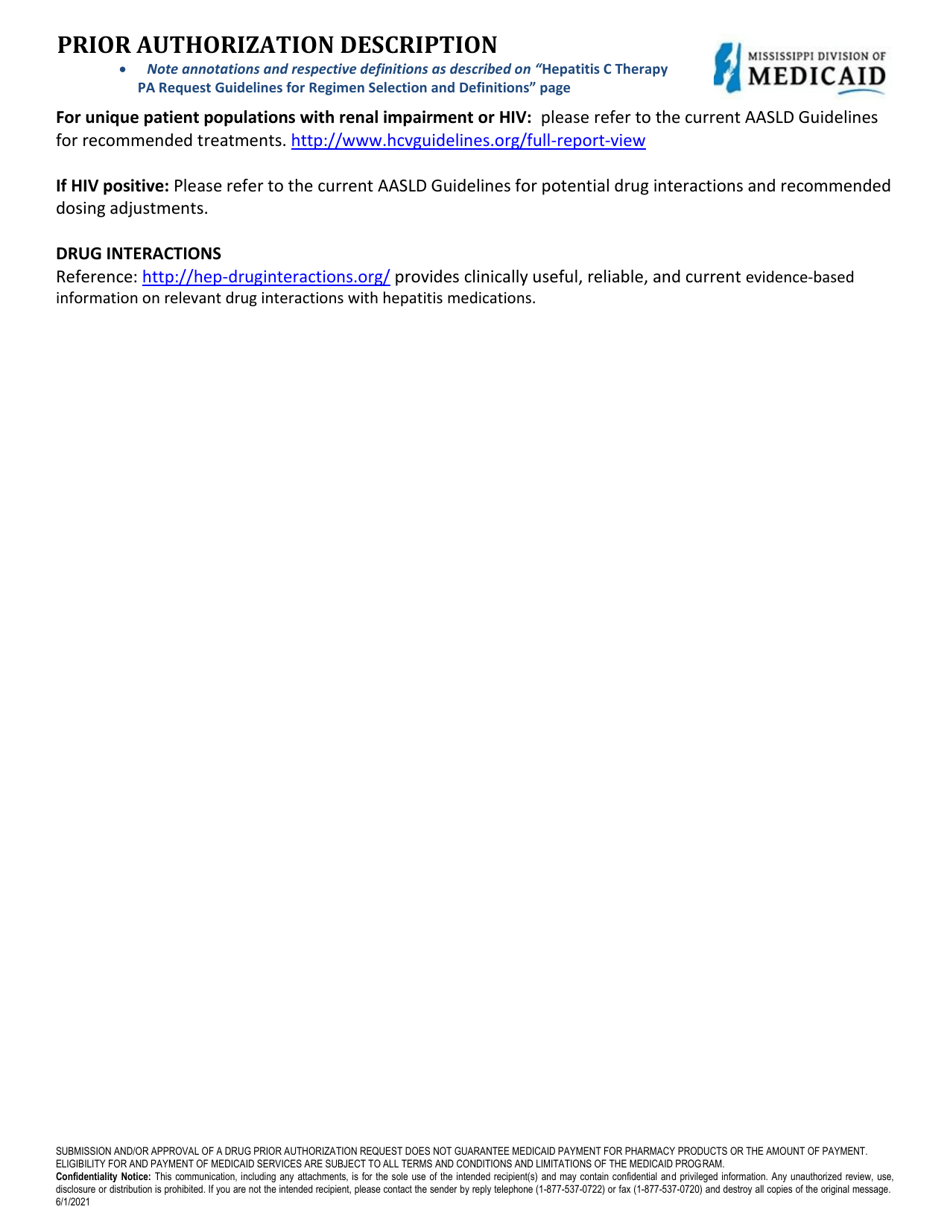
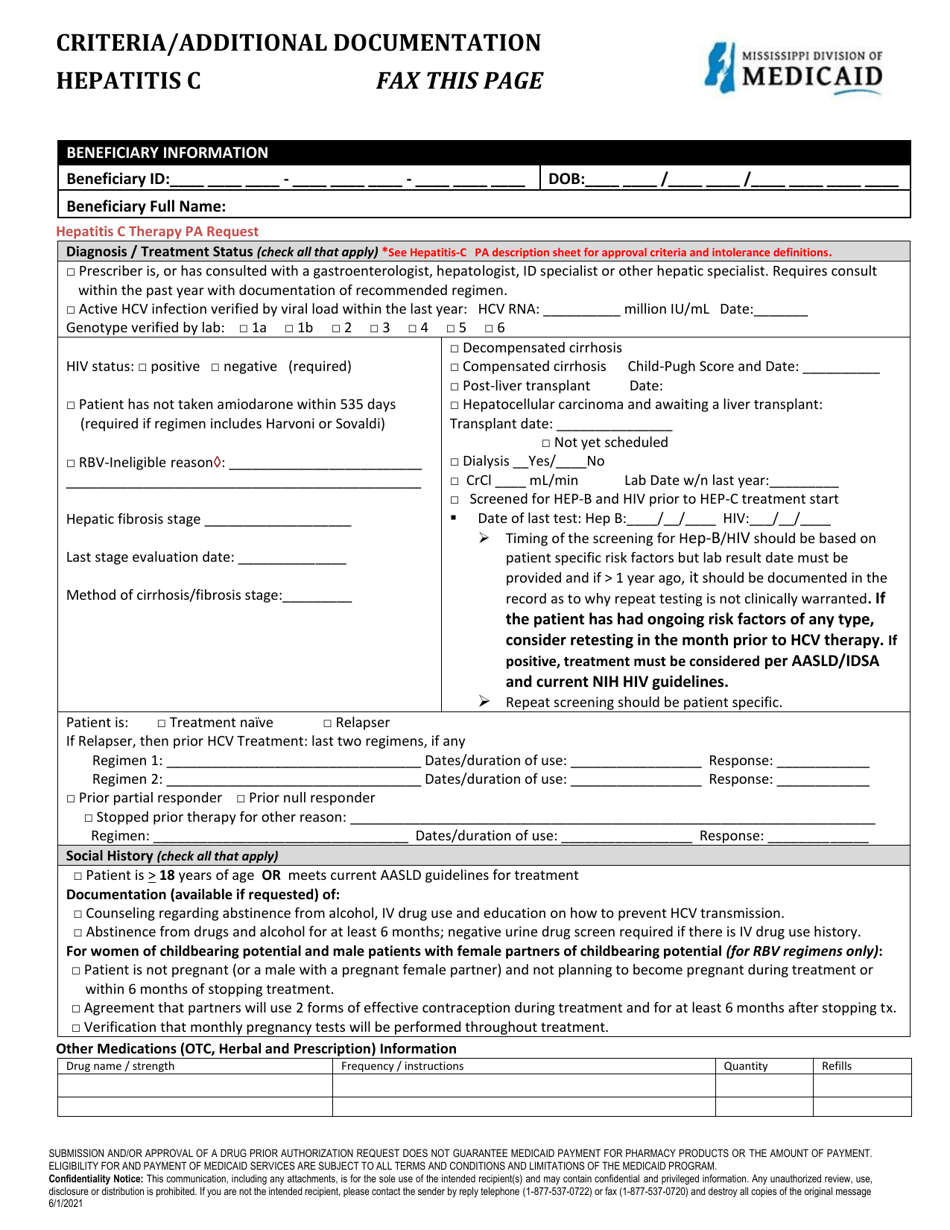
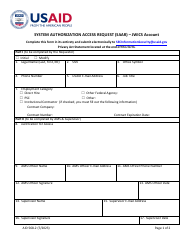
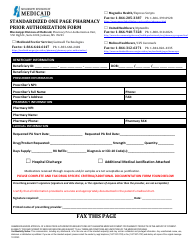
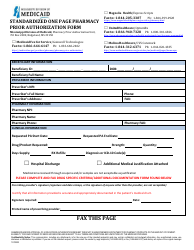
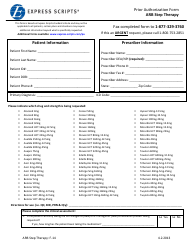
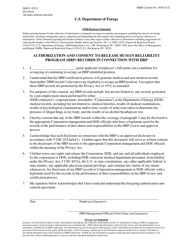
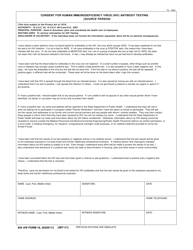
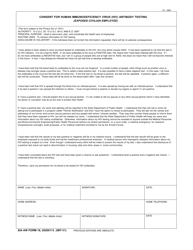
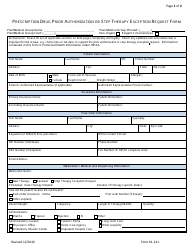
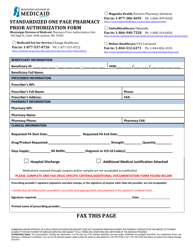
Prior Authorization Form - Hepatitis C Therapy - Mississippi
Prior Authorization Form - Hepatitis C Therapy is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is a prior authorization form?
A: A prior authorization form is a document that your doctor or healthcare provider fills out to request coverage for a specific medication or treatment.
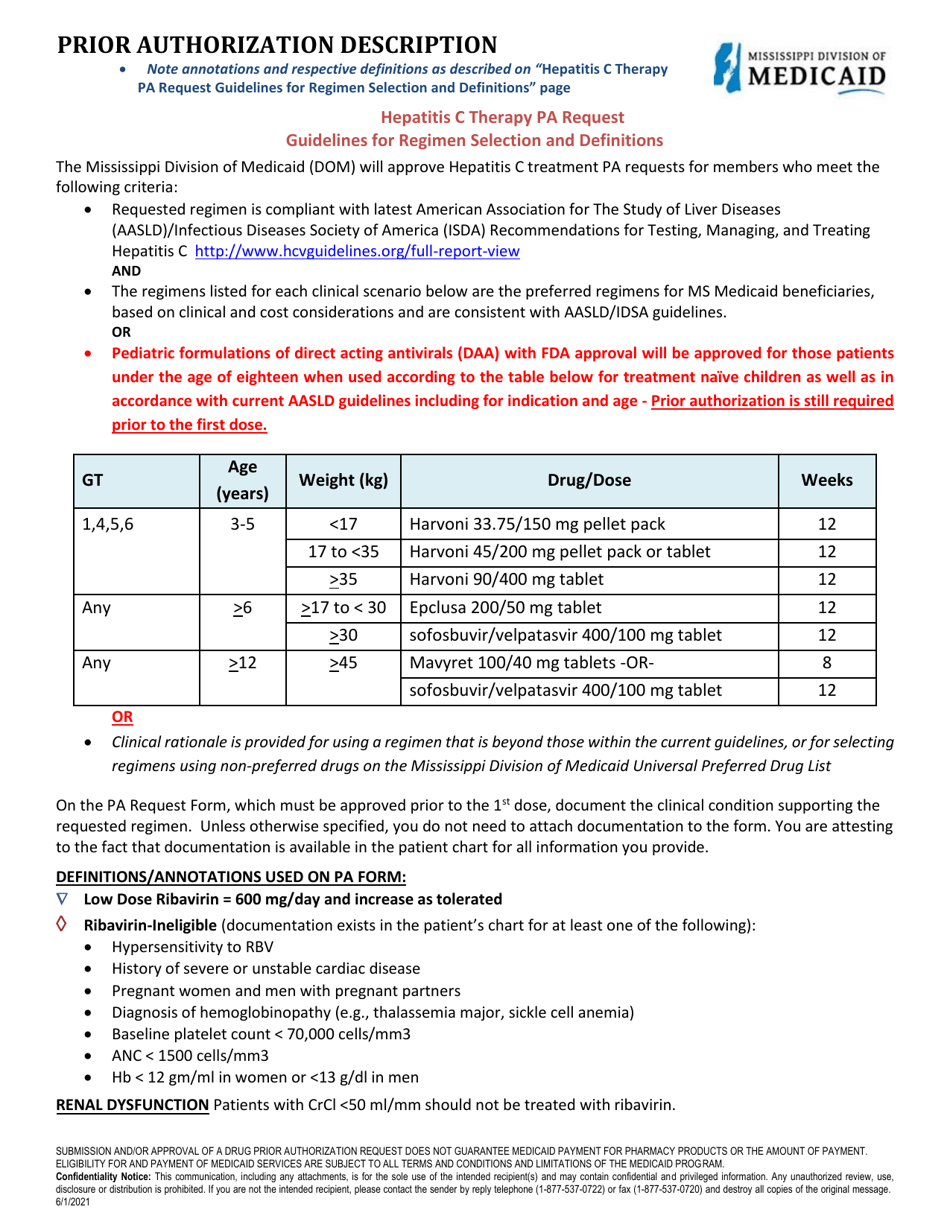
Q: What is Hepatitis C?
A: Hepatitis C is a viral infection that affects the liver.
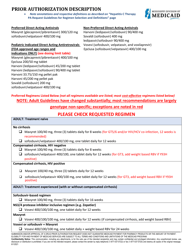
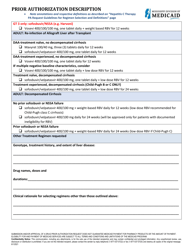
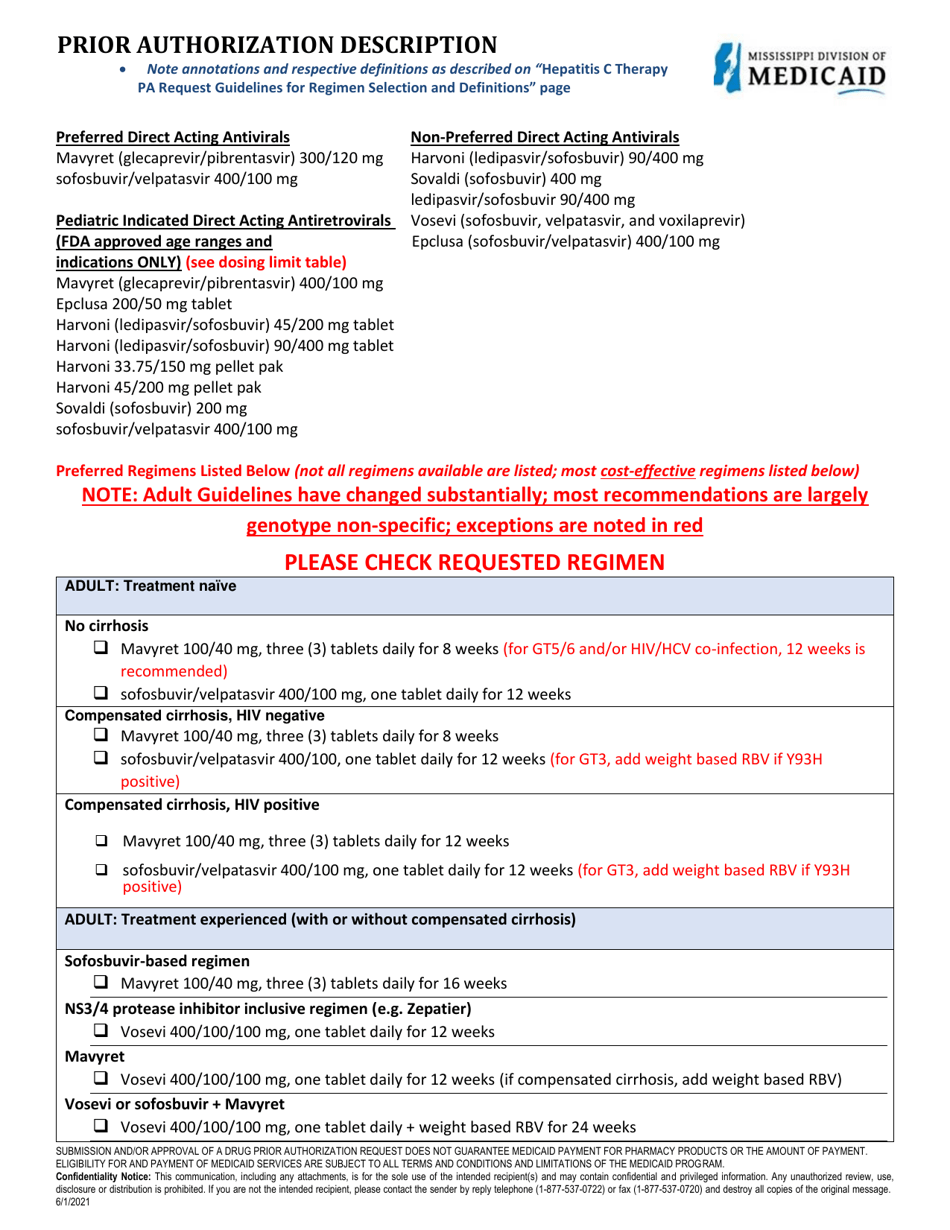
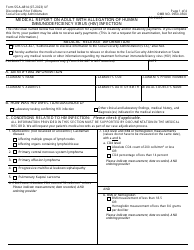
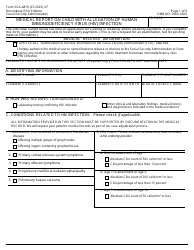
Q: What is Hepatitis C therapy?
A: Hepatitis C therapy is a treatment to manage or cure Hepatitis C infection.
Q: Why is a prior authorization form needed for Hepatitis C therapy?
A: A prior authorization form is required to ensure that your health insurance plan covers the cost of Hepatitis C therapy.
Q: Who needs to fill out the prior authorization form?
A: Your doctor or healthcare provider needs to fill out the prior authorization form.
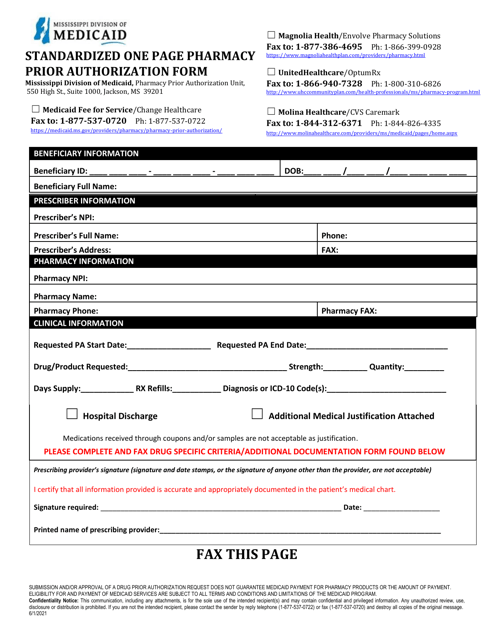
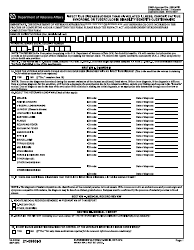
Q: What information is required on the prior authorization form?
A: The prior authorization form will require information such as your personal details, diagnosis, prescribed medication, and supporting medical documentation.
Q: How long does it take for a prior authorization to be approved?
A: The time taken to approve a prior authorization can vary, but typically it can take a few days to a couple of weeks.
Q: What happens if the prior authorization is denied?
A: If the prior authorization is denied, your doctor may work with your insurance company to provide additional information or explore other treatment options.
Q: Will I have to pay for Hepatitis C therapy if the prior authorization is denied?
A: If the prior authorization is denied, you may be responsible for the full cost of Hepatitis C therapy, unless you can explore alternative payment options.
Form Details:
- Released on June 1, 2021;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.