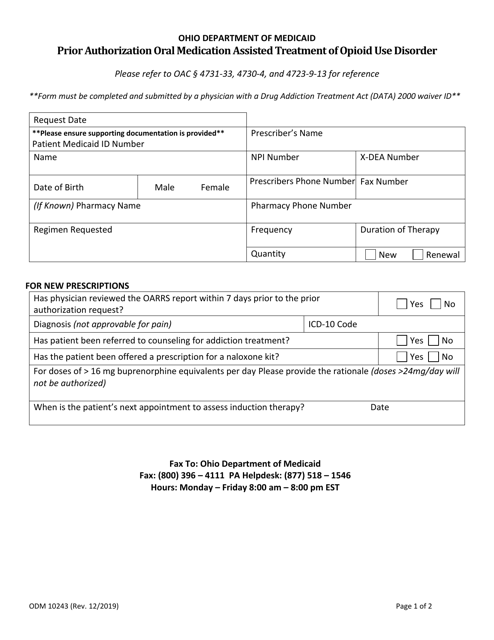
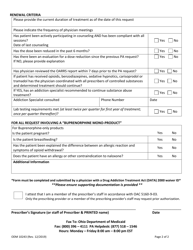
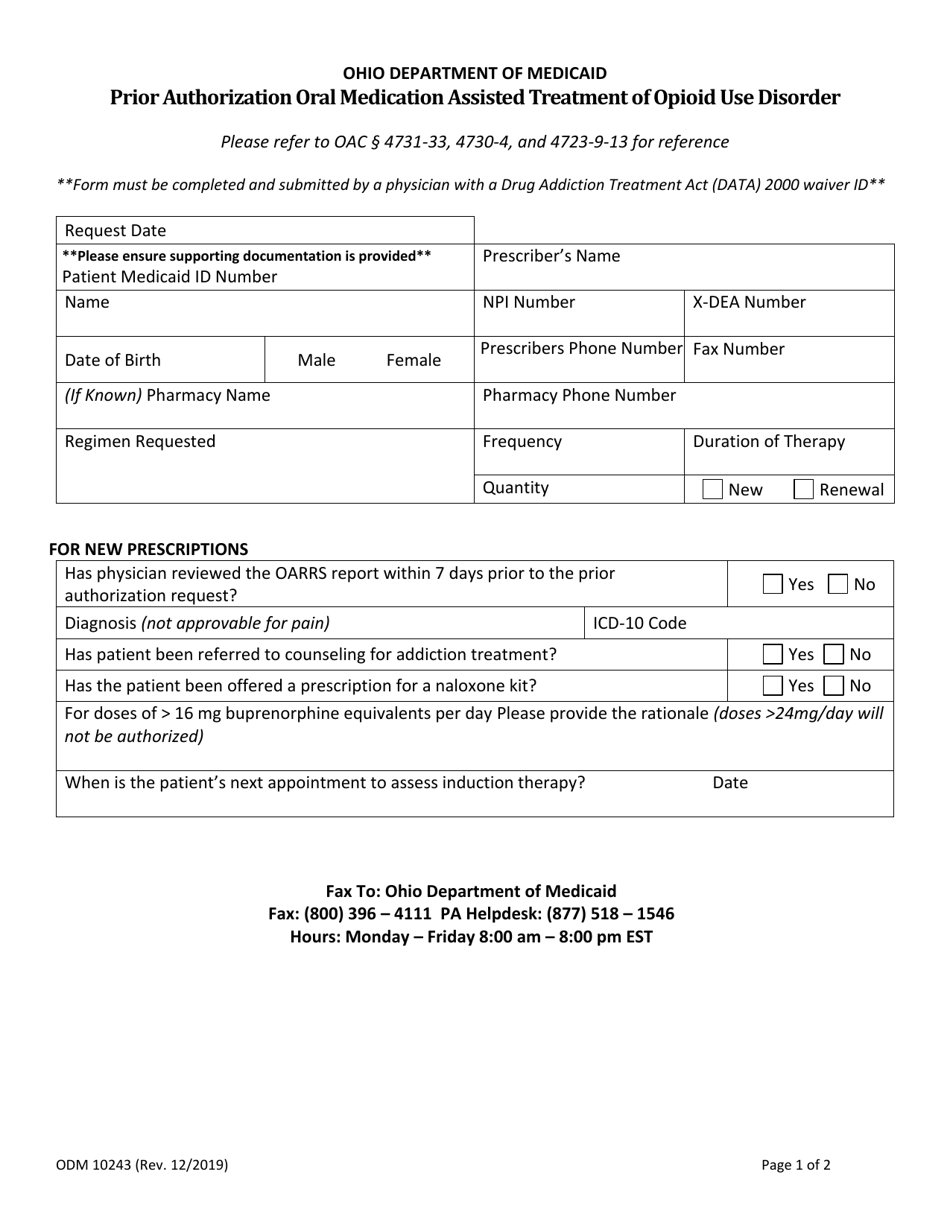
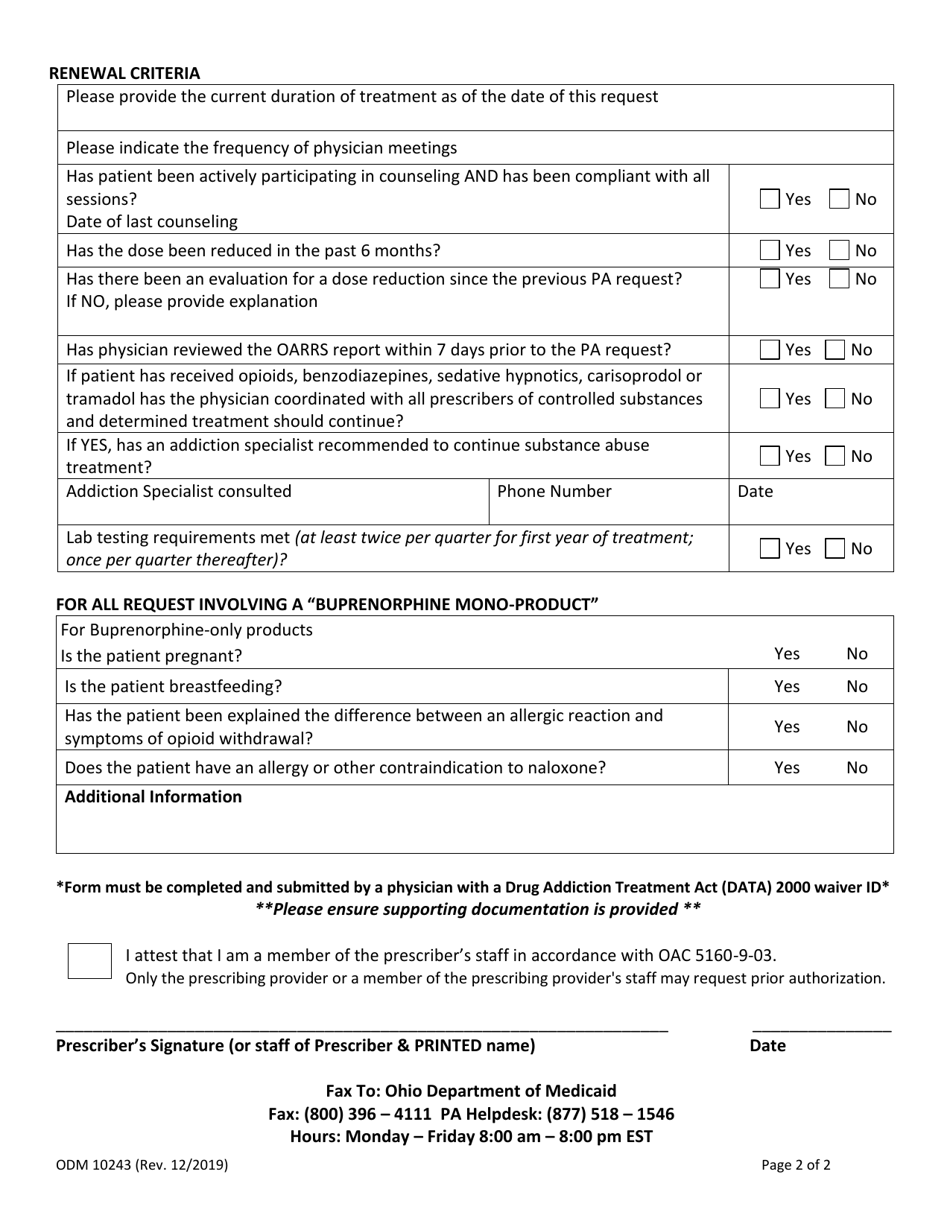
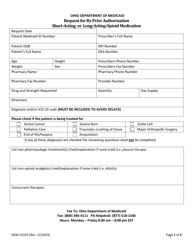
Form ODM10243 Prior Authorization Oral Medication Assisted Treatment of Opioid Use Disorder - Ohio
What Is Form ODM10243?
This is a legal form that was released by the Ohio Department of Medicaid - a government authority operating within Ohio. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is the ODM10243 form?
A: ODM10243 is the Prior Authorization form for oral medication assisted treatment of opioid use disorder in Ohio.
Q: What is the purpose of the form?
A: The form is used to request prior authorization for medication assisted treatment of opioid use disorder with oral medications.
Q: Who can use the form?
A: The form is intended for healthcare providers in Ohio who are seeking to initiate or continue oral medication assisted treatment for opioid use disorder.
Q: What types of medications are covered by the form?
A: The form is specifically for oral medications used in medication assisted treatment of opioid use disorder, such as buprenorphine or naltrexone.
Q: What information is required on the form?
A: The form requires various information including patient demographics, diagnosis, treatment history, and details of the requested medication treatment plan.
Q: How long does the prior authorization process take?
A: The processing time for prior authorization requests can vary, but generally, a response is provided within 14 business days.
Q: Can the form be submitted electronically?
A: Yes, the ODM10243 form can be submitted electronically through the Ohio Department of Medicaid's secure web portal.
Q: Is prior authorization required for all medication assisted treatment for opioid use disorder?
A: No, prior authorization is only required for oral medication assisted treatment. Other forms of medication assisted treatment, such as injectable medications, may have their own authorization processes.
Q: What if the prior authorization request is denied?
A: If a prior authorization request is denied, the healthcare provider can appeal the decision or explore alternative treatment options for the patient.
Form Details:
- Released on December 1, 2019;
- The latest edition provided by the Ohio Department of Medicaid;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form ODM10243 by clicking the link below or browse more documents and templates provided by the Ohio Department of Medicaid.