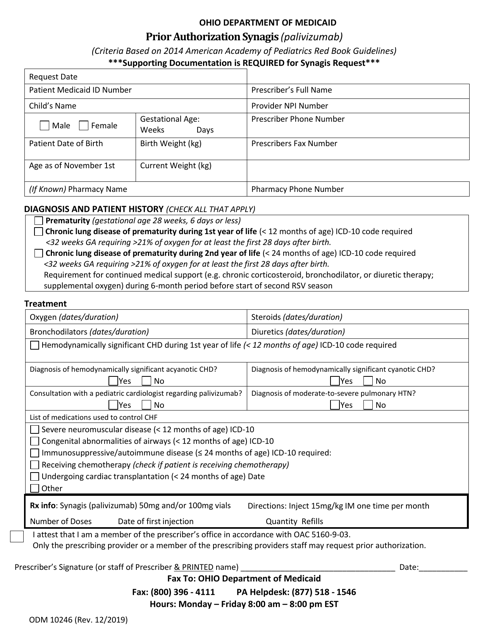
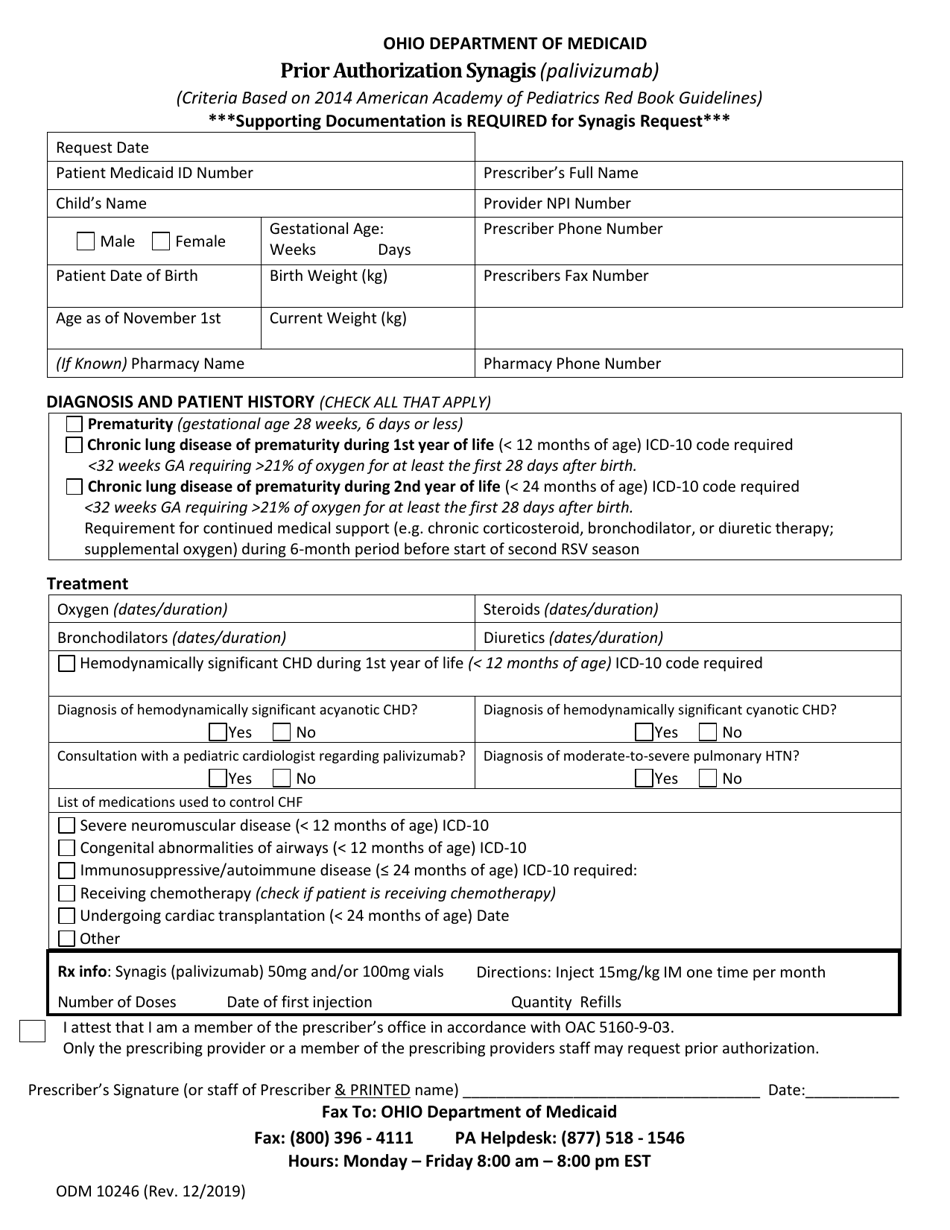
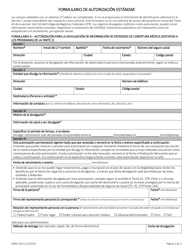
Form ODM10246 Prior Authorization Synagis - Ohio
What Is Form ODM10246?
This is a legal form that was released by the Ohio Department of Medicaid - a government authority operating within Ohio. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is a Prior Authorization?
A: A Prior Authorization is a requirement by health insurance companies to obtain approval before a specific medication or treatment will be covered.
Q: What is Synagis?
A: Synagis is a medication that helps prevent serious lung infections caused by respiratory syncytial virus (RSV) in high-risk infants.
Q: Who needs prior authorization for Synagis in Ohio?
A: In Ohio, prior authorization is typically required for Synagis for high-risk infants who are at increased risk of severe RSV infection.
Q: How can I obtain a Prior Authorization for Synagis in Ohio?
A: To obtain a Prior Authorization for Synagis in Ohio, you will need to contact your health insurance company and follow their specific process for requesting authorization.
Q: What information is typically required for a Prior Authorization?
A: The specific information required for a Prior Authorization may vary, but it generally includes the infant's medical history, documentation of high-risk status, and a prescription from a healthcare provider.
Q: What happens if a Prior Authorization for Synagis is denied?
A: If a Prior Authorization for Synagis is denied, you may have the option to appeal the decision or explore other options for obtaining the medication, such as patient assistance programs or other financial assistance programs.
Q: Are there any alternatives to Synagis?
A: There may be alternatives to Synagis for preventing severe RSV infection in high-risk infants. It is best to consult with a healthcare provider to discuss the options that may be available.
Form Details:
- Released on December 1, 2019;
- The latest edition provided by the Ohio Department of Medicaid;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form ODM10246 by clicking the link below or browse more documents and templates provided by the Ohio Department of Medicaid.