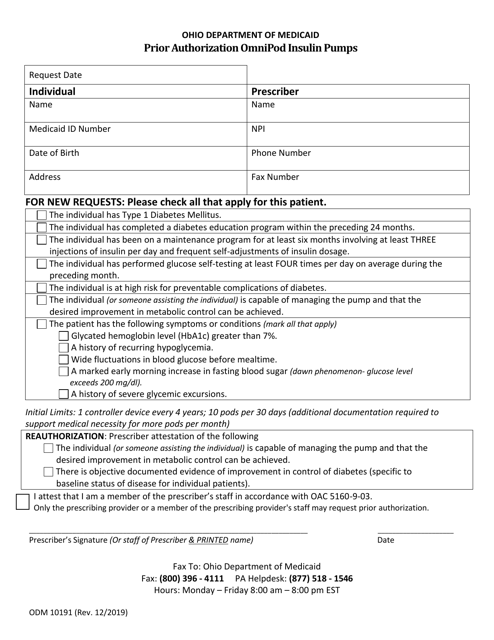
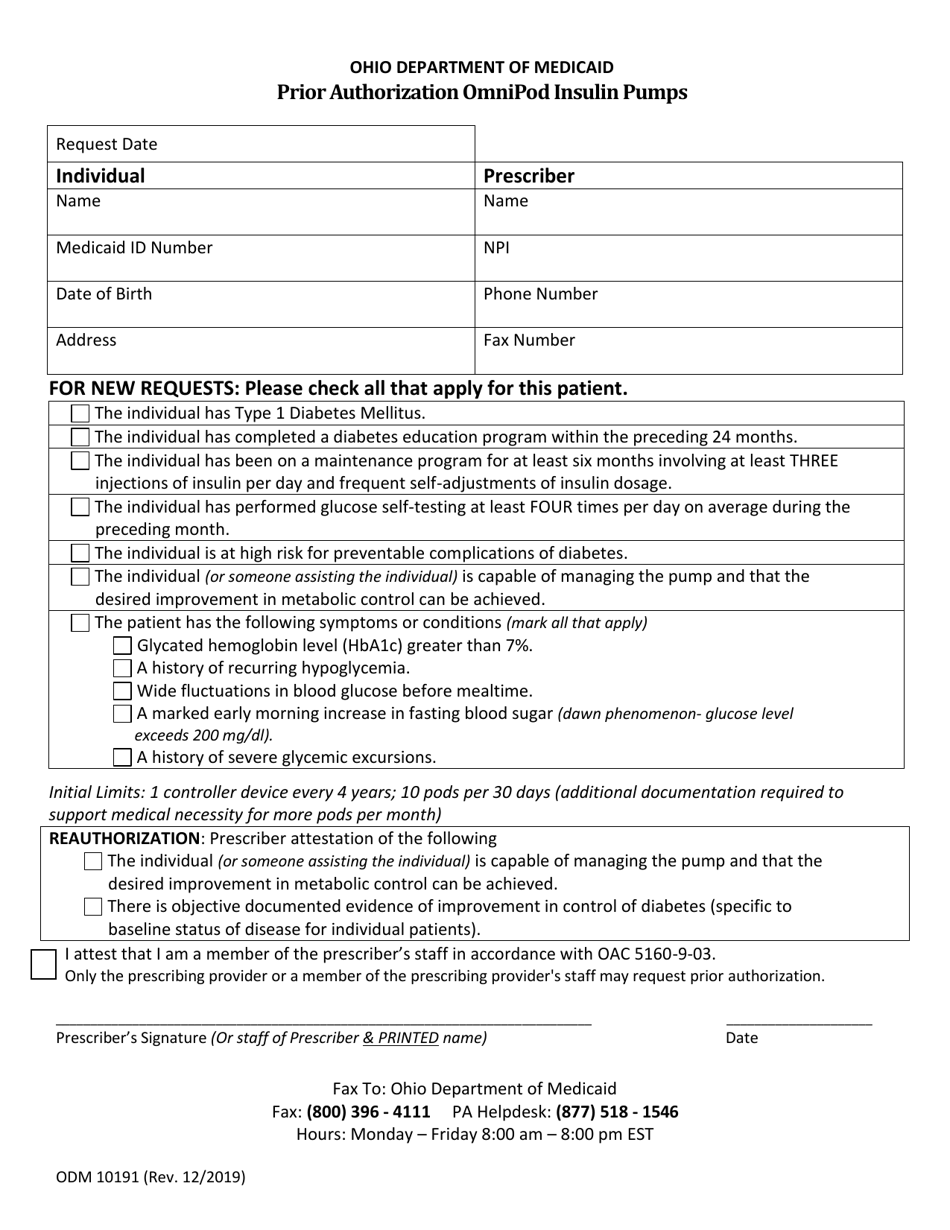
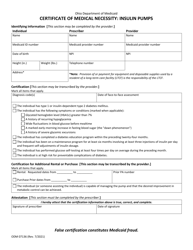
Form ODM10191 Prior Authorization Omnipod Insulin Pumps - Ohio
What Is Form ODM10191?
This is a legal form that was released by the Ohio Department of Medicaid - a government authority operating within Ohio. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form ODM10191 Prior Authorization Omnipod Insulin Pumps?
A: Form ODM10191 is a prior authorization form used in Ohio to request coverage for Omnipod insulin pumps.
Q: What is a prior authorization?
A: A prior authorization is a process where healthcare providers must obtain approval from an insurance company before certain medications, devices, or treatments will be covered.
Q: What are Omnipod insulin pumps?
A: Omnipod insulin pumps are a type of insulin delivery system that is worn on the body and provides continuous insulin infusion.
Q: Why is prior authorization necessary for Omnipod insulin pumps?
A: Prior authorization is necessary to ensure that insurance will cover the cost of the Omnipod insulin pump, as it may be a higher-cost option compared to other insulin delivery systems.
Q: How can I get Form ODM10191?
A: Form ODM10191 can be obtained from your healthcare provider or insurance company. They will be able to provide you with the necessary form and instructions on how to complete it.
Q: What information is required on Form ODM10191?
A: The form typically requires information such as patient details, healthcare provider information, medical history, and supporting documentation to justify the need for the Omnipod insulin pump.
Q: How long does the prior authorization process take?
A: The length of the prior authorization process can vary, but it typically takes a few business days to a few weeks to receive a decision from the insurance company.
Q: What happens after the prior authorization is approved?
A: If the prior authorization is approved, the insurance company will cover the cost of the Omnipod insulin pump, subject to any applicable deductibles or copayments.
Q: What should I do if my prior authorization is denied?
A: If your prior authorization is denied, you can work with your healthcare provider to appeal the decision. They may be able to provide additional information or documentation to support your case.
Q: Are there any alternatives to Omnipod insulin pumps?
A: Yes, there are other insulin delivery systems available, such as insulin pens or traditional insulin pumps. Your healthcare provider can discuss these options with you.
Q: Does Form ODM10191 apply only to Ohio residents?
A: Yes, Form ODM10191 is specific to Ohio residents and is used for requesting prior authorization for Omnipod insulin pumps in Ohio.
Form Details:
- Released on December 1, 2019;
- The latest edition provided by the Ohio Department of Medicaid;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form ODM10191 by clicking the link below or browse more documents and templates provided by the Ohio Department of Medicaid.