This version of the form is not currently in use and is provided for reference only. Download this version of
Form ODM01711
for the current year.
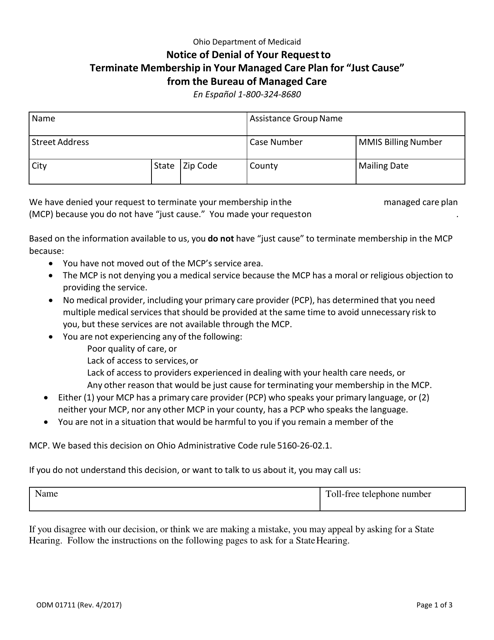
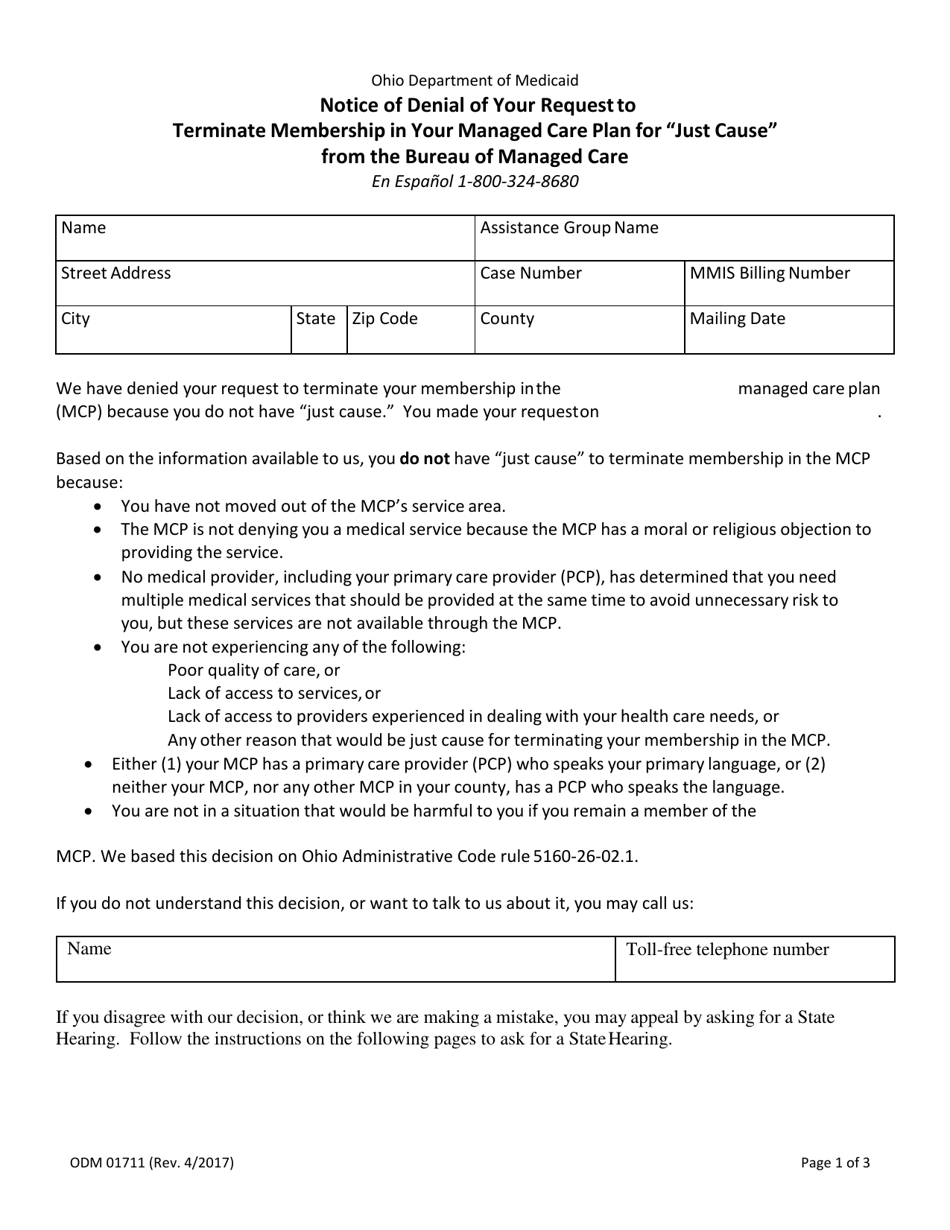
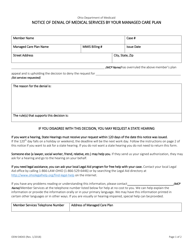
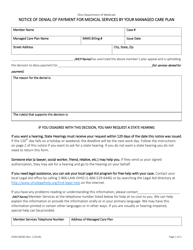
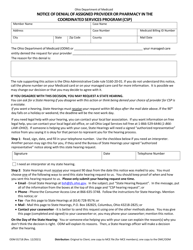
Form ODM01711 Notice of Denial of Your Request to Terminate Membership in Your Managed Care Plan for "just Cause" From the Bureau of Managed Care - Ohio
What Is Form ODM01711?
This is a legal form that was released by the Ohio Department of Medicaid - a government authority operating within Ohio. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is ODM01711?
A: ODM01711 is a notice of denial of your request to terminate membership in your managed care plan for 'just cause' from the Bureau of Managed Care - Ohio.
Q: What does 'just cause' mean?
A: 'Just cause' refers to a valid reason or justification for terminating your membership in a managed care plan.
Q: Why would I receive a notice of denial?
A: You would receive a notice of denial if the Bureau of Managed Care - Ohio has determined that your request to terminate membership in your managed care plan does not have 'just cause'.
Q: What should I do if my request was denied?
A: If your request to terminate membership in your managed care plan was denied, you should review the reasons provided in the notice and consider seeking further clarification or assistance from the Bureau of Managed Care - Ohio.
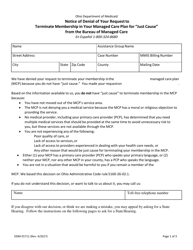
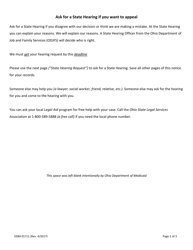
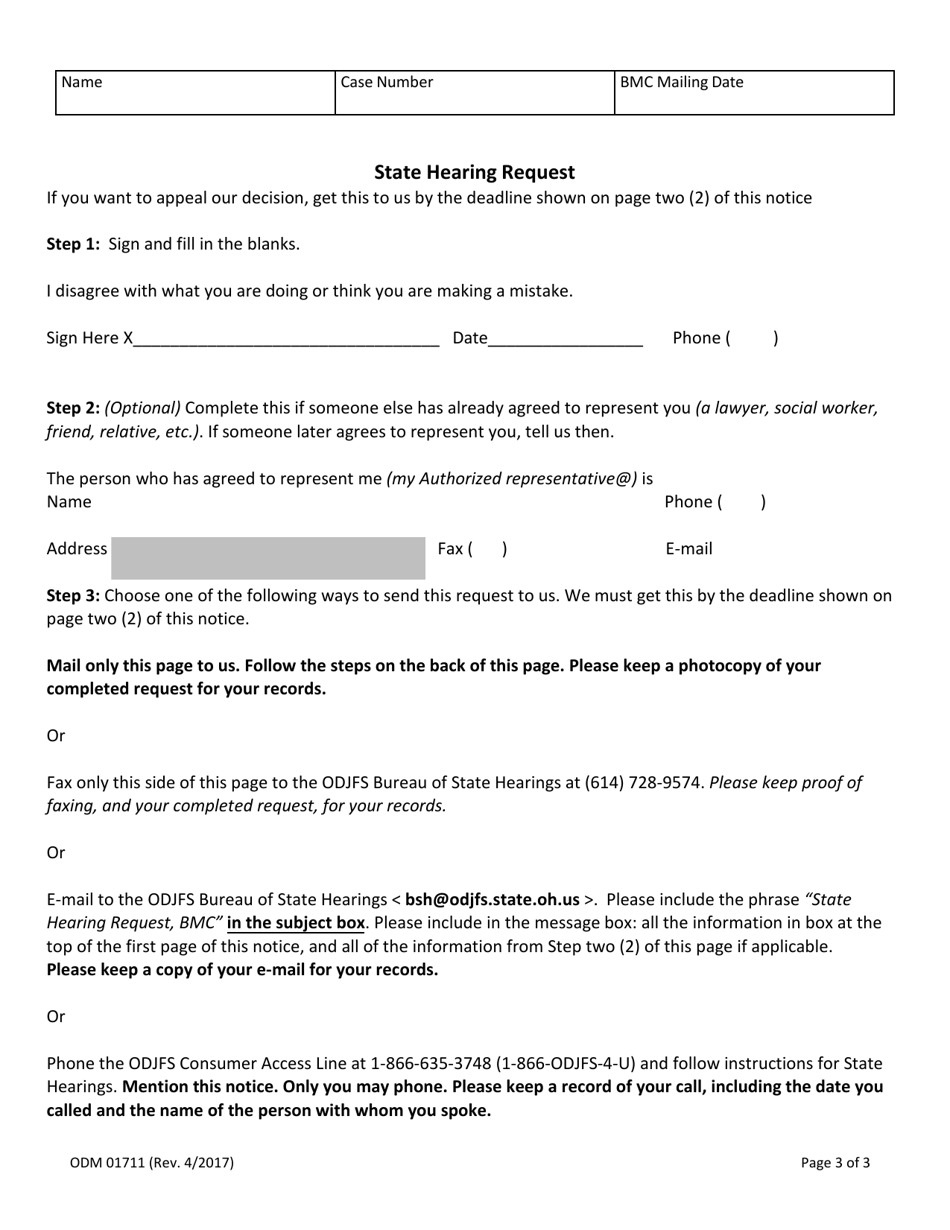
Q: Can I appeal the denial?
A: Yes, you have the right to appeal the denial of your request to terminate membership in your managed care plan. The notice should provide information on how tofile an appeal.
Q: What is the Bureau of Managed Care - Ohio?
A: The Bureau of Managed Care - Ohio is an organization responsible for overseeing managed care plans and addressing complaints or issues related to these plans in the state of Ohio.
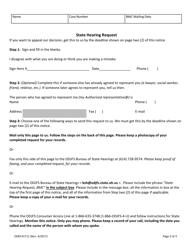
Form Details:
- Released on April 1, 2017;
- The latest edition provided by the Ohio Department of Medicaid;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form ODM01711 by clicking the link below or browse more documents and templates provided by the Ohio Department of Medicaid.