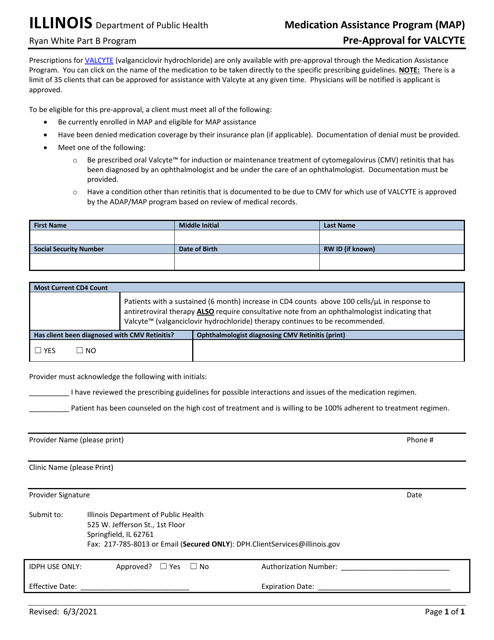
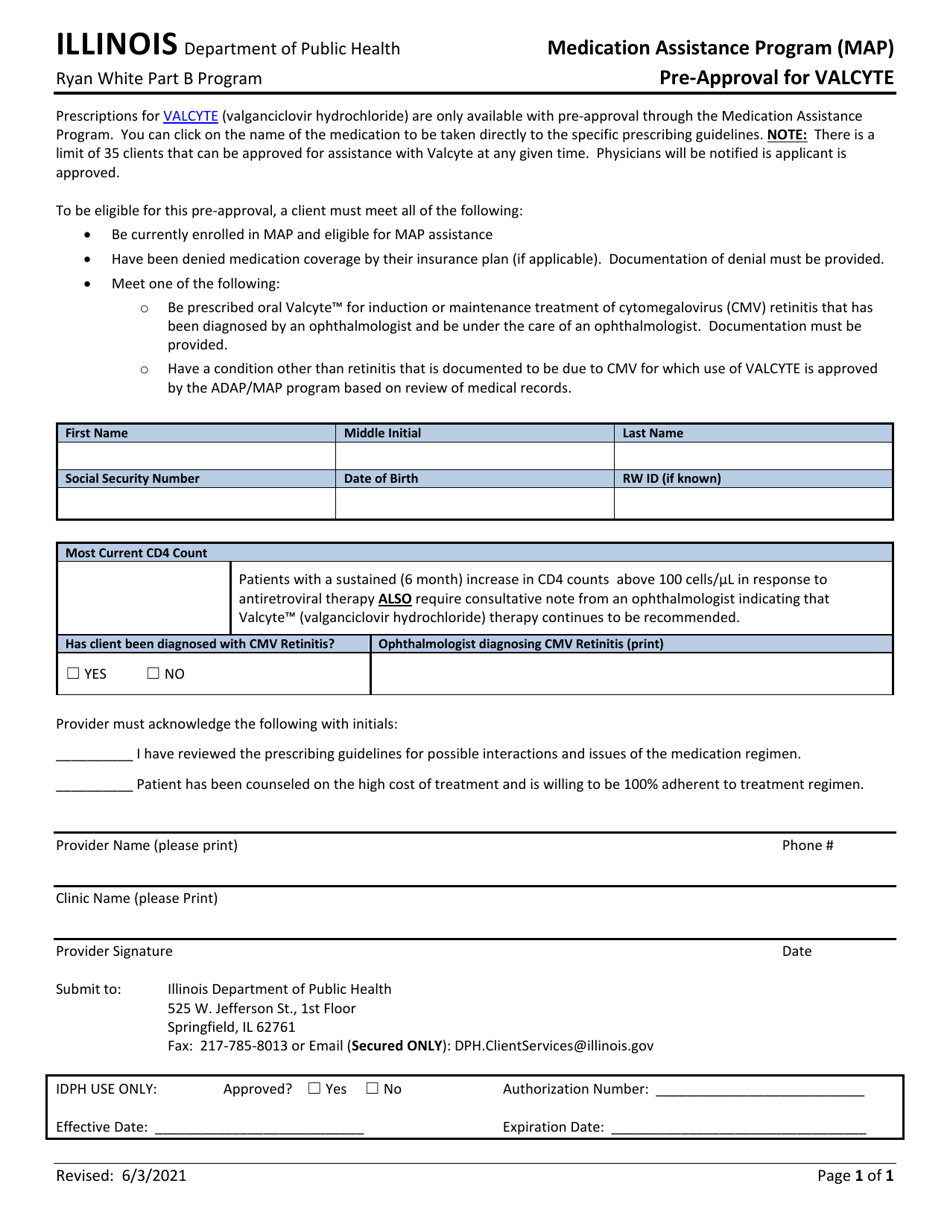
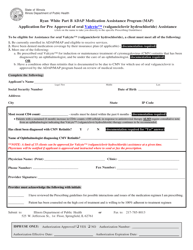
Prior Authorization for Valganciclovir Hydrochloride (Valcyte) - Illinois
Prior Authorization for Valganciclovir Hydrochloride (Valcyte) is a legal document that was released by the Illinois Department of Public Health - a government authority operating within Illinois.
FAQ
Q: What is Valganciclovir Hydrochloride (Valcyte)?
A: Valganciclovir Hydrochloride (Valcyte) is a prescription medication used to treat certain viral infections.
Q: What is prior authorization?
A: Prior authorization is a process where your healthcare provider needs to get approval from your insurance company before you can start taking Valganciclovir Hydrochloride (Valcyte).
Q: Why is prior authorization required for Valganciclovir Hydrochloride (Valcyte)?
A: Prior authorization is required to ensure that Valganciclovir Hydrochloride (Valcyte) is being used appropriately and is medically necessary.
Q: How can I get prior authorization for Valganciclovir Hydrochloride (Valcyte)?
A: You need to contact your insurance company or healthcare provider to initiate the prior authorization process.
Q: What information is needed for prior authorization?
A: Typically, you will need to provide information about your medical condition, previous treatments, and why Valganciclovir Hydrochloride (Valcyte) is necessary for your treatment.
Q: What if my prior authorization request is denied?
A: If your prior authorization request is denied, you can appeal the decision or discuss alternative treatment options with your healthcare provider.
Q: How long does the prior authorization process take?
A: The time taken for the prior authorization process can vary, but it usually takes a few days to a couple of weeks.
Q: Does prior authorization guarantee coverage?
A: No, prior authorization does not guarantee coverage. It only indicates that the treatment is being evaluated for approval.
Q: Can I start taking Valganciclovir Hydrochloride (Valcyte) without prior authorization?
A: It is best to wait for the prior authorization approval before starting the medication to ensure coverage and avoid any unexpected costs.
Q: Is prior authorization required for all medications?
A: No, prior authorization is not required for all medications. It is typically required for certain high-cost or specialized medications.
Form Details:
- Released on June 3, 2021;
- The latest edition currently provided by the Illinois Department of Public Health;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Illinois Department of Public Health.