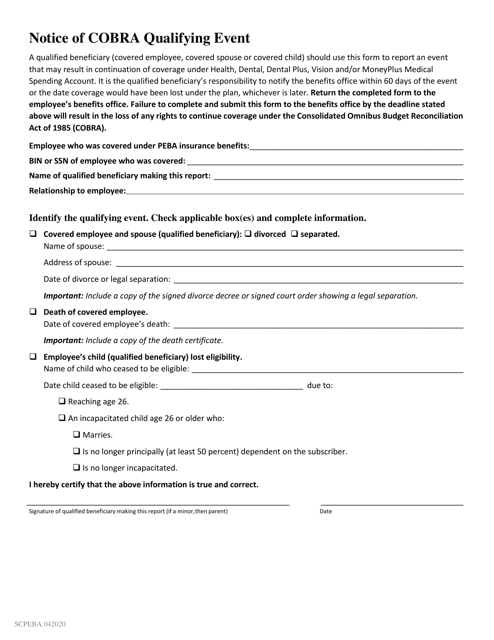
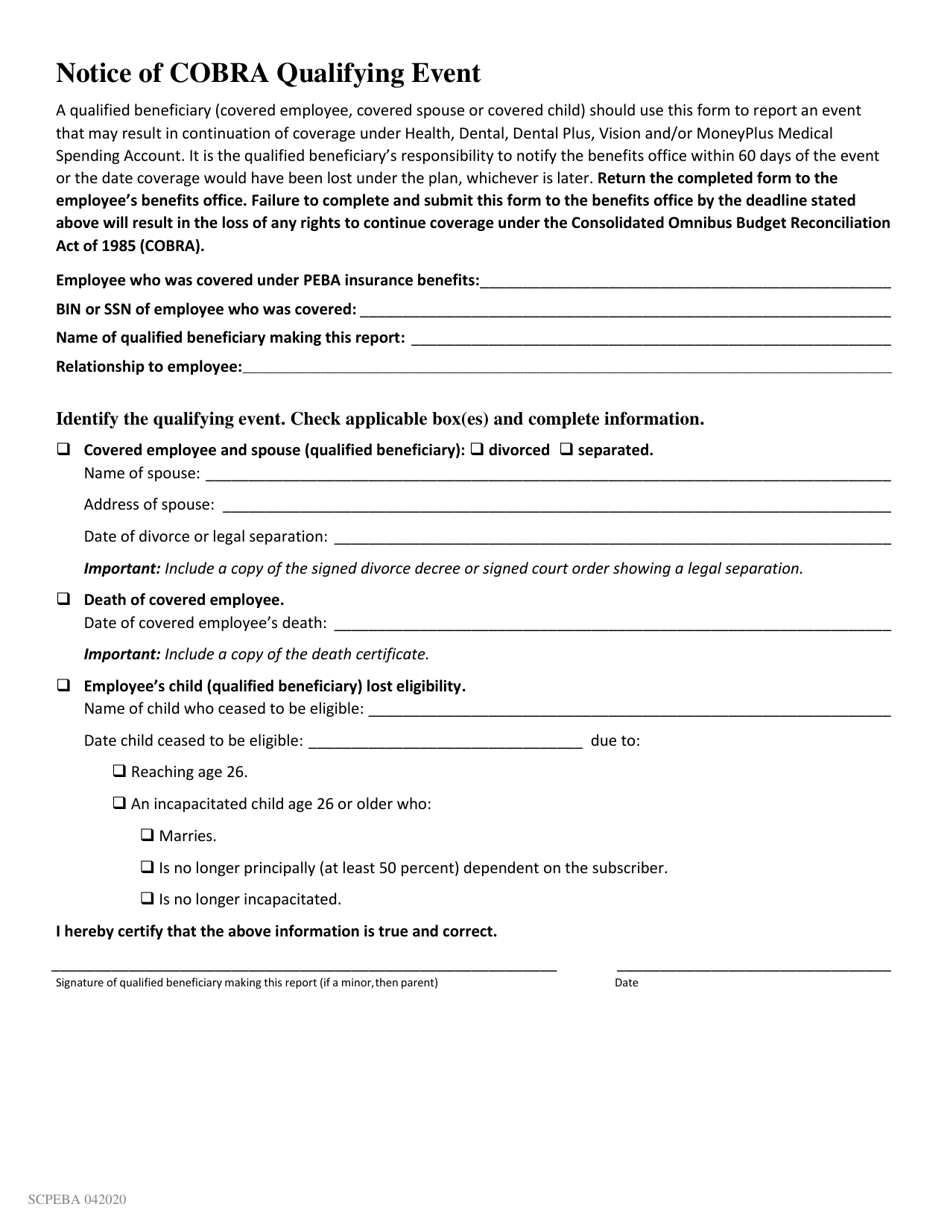
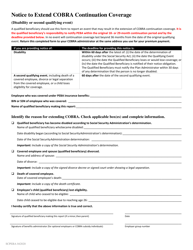
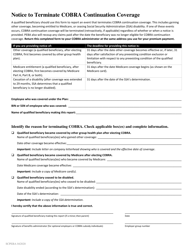
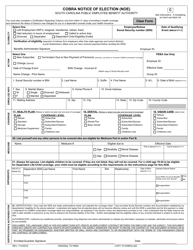
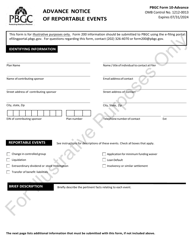
Notice of Cobra Qualifying Event - South Carolina
Notice of Cobra Qualifying Event is a legal document that was released by the South Carolina Public Employee Benefit Authority - a government authority operating within South Carolina.
FAQ
Q: What is a COBRA qualifying event?
A: A COBRA qualifying event is an event that allows an individual to become eligible for COBRA continuation coverage.
Q: What is COBRA continuation coverage?
A: COBRA continuation coverage is a health insurance coverage that allows certain individuals to continue their health insurance benefits when they would otherwise lose coverage.
Q: What are some examples of COBRA qualifying events?
A: Some examples include termination of employment, reduction in work hours, divorce or legal separation, and loss of eligibility for dependent status.
Q: How long does COBRA continuation coverage last?
A: COBRA continuation coverage typically lasts for 18 months, although some events may qualify for extended coverage of up to 36 months.
Q: Who is eligible for COBRA continuation coverage?
A: Eligibility for COBRA continuation coverage generally applies to employees and their families who were covered under a group health plan and have experienced a qualifying event.
Q: What should I do if I experience a COBRA qualifying event?
A: If you experience a COBRA qualifying event, you should contact your former employer or the plan administrator to inquire about your options for COBRA continuation coverage.
Form Details:
- Released on April 1, 2020;
- The latest edition currently provided by the South Carolina Public Employee Benefit Authority;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the South Carolina Public Employee Benefit Authority.