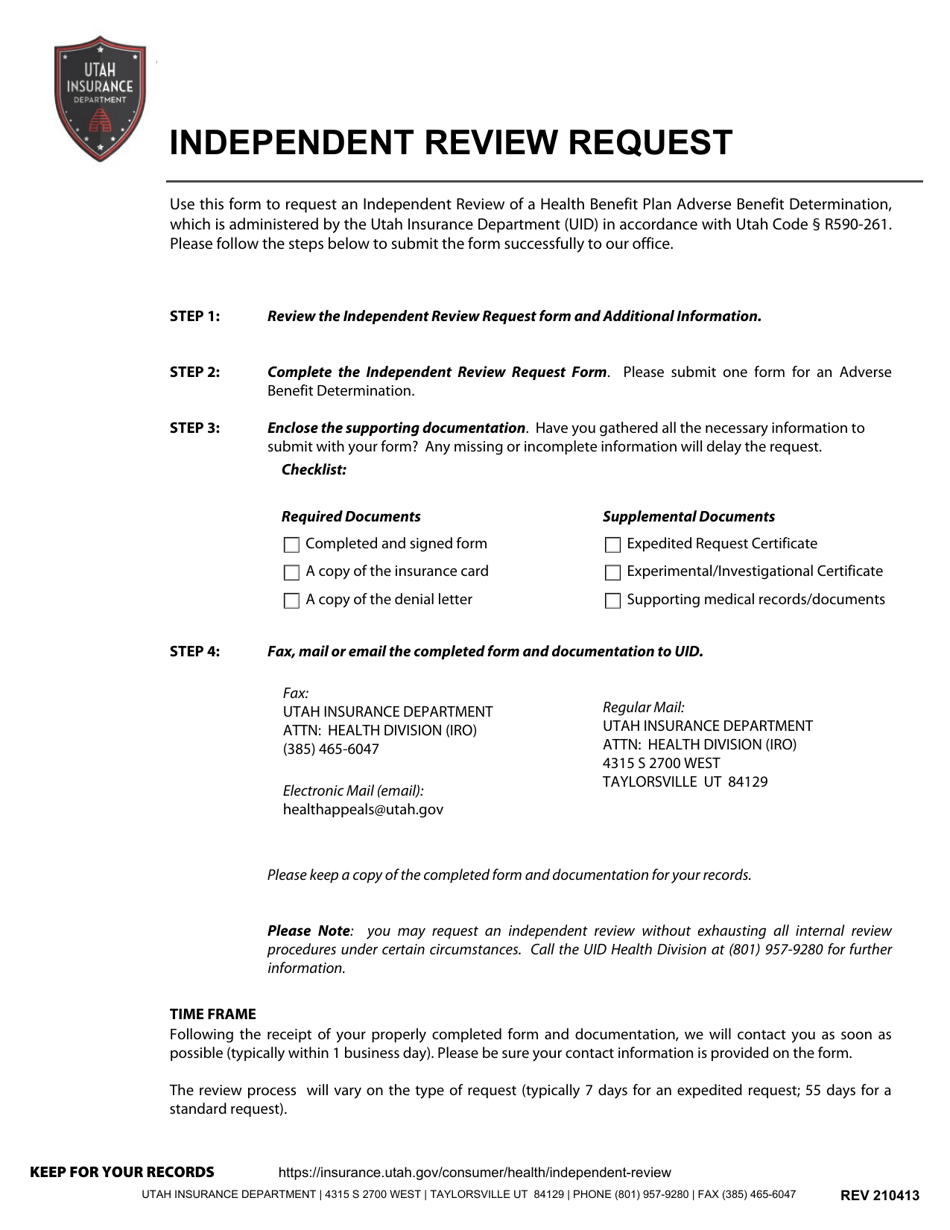
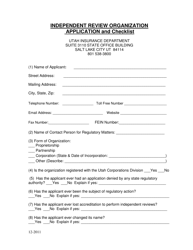
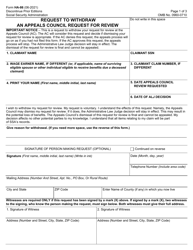
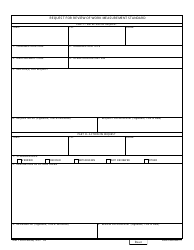
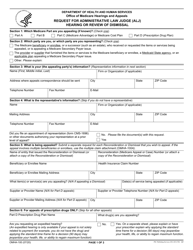
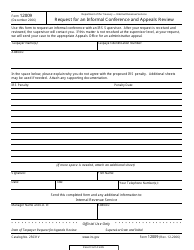
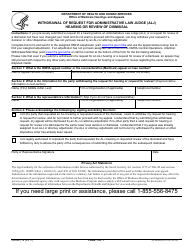
Independent Review Request - Utah
Independent Review Request is a legal document that was released by the Utah Insurance Department - a government authority operating within Utah.
FAQ
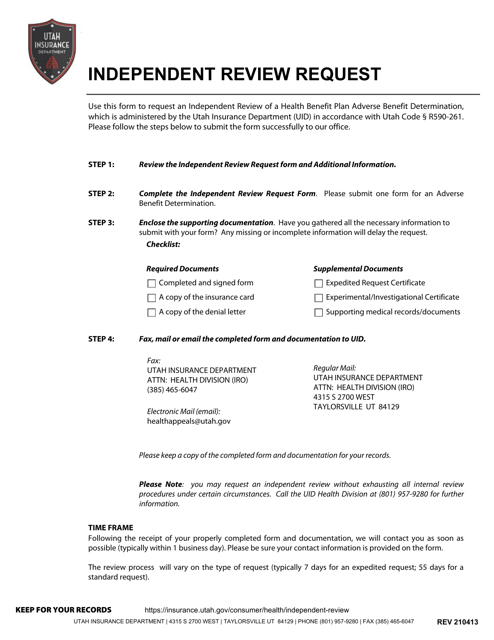
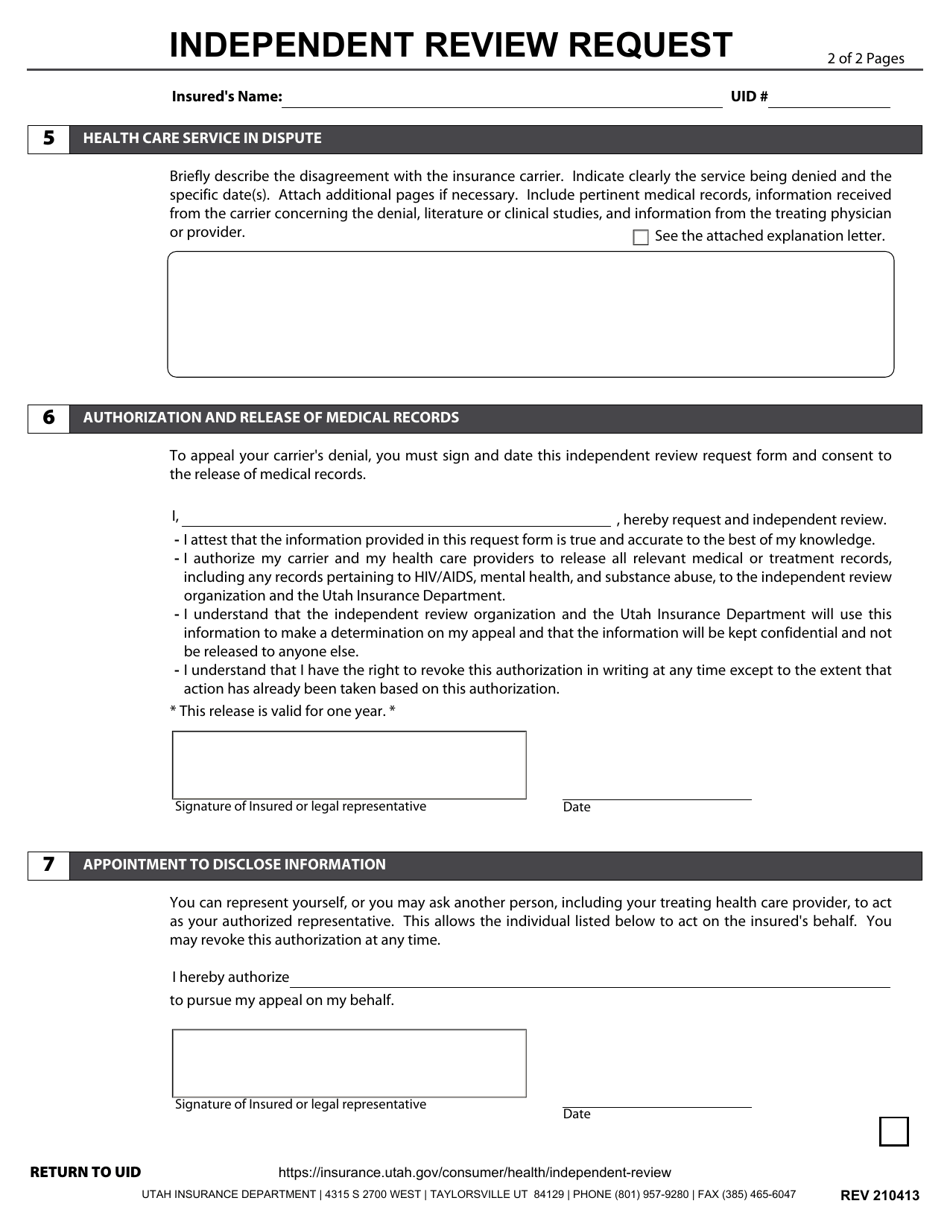
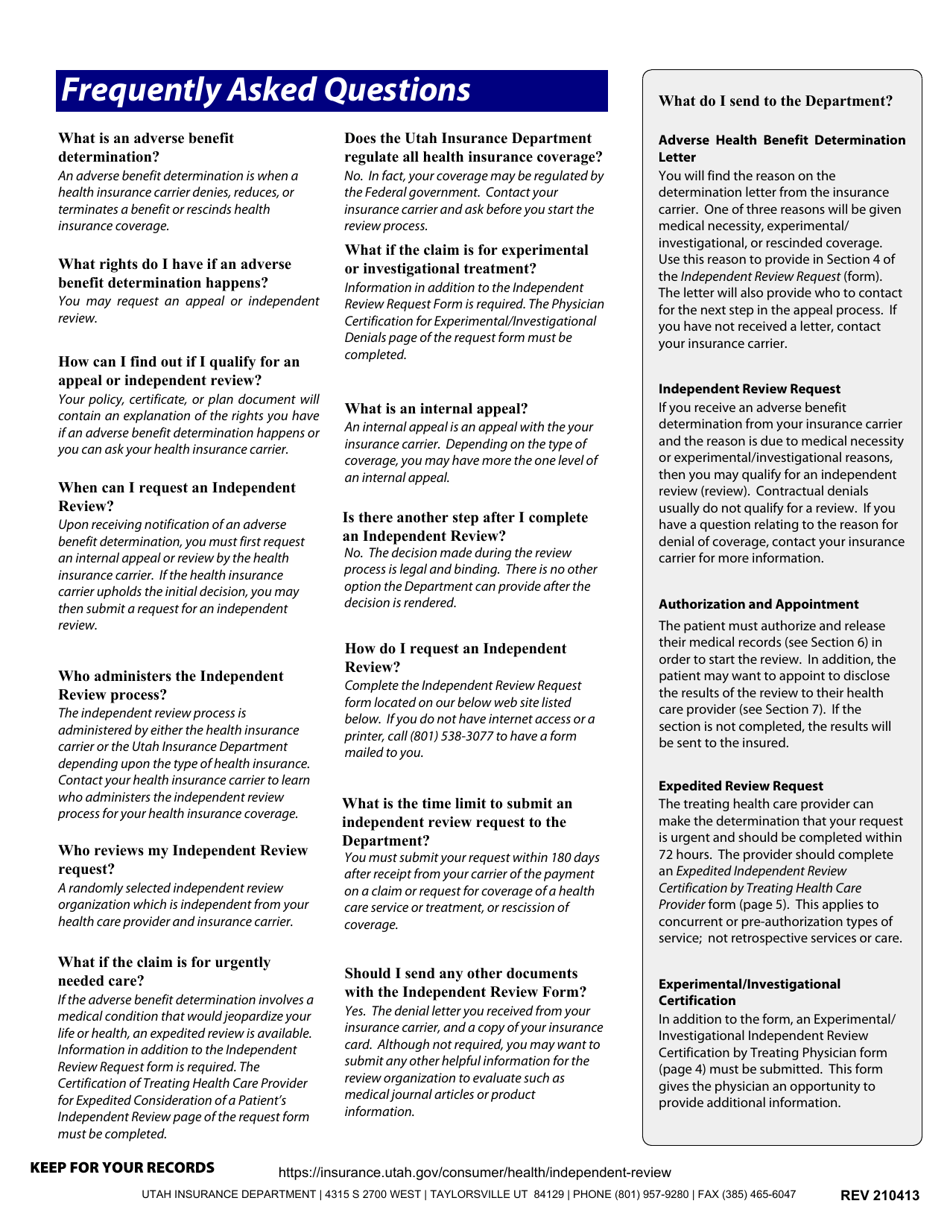
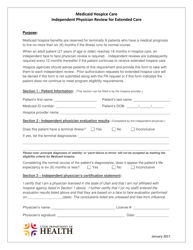
Q: What is an Independent Review Request?
A: An Independent Review Request is a process for appealing health insurance denials and decisions.
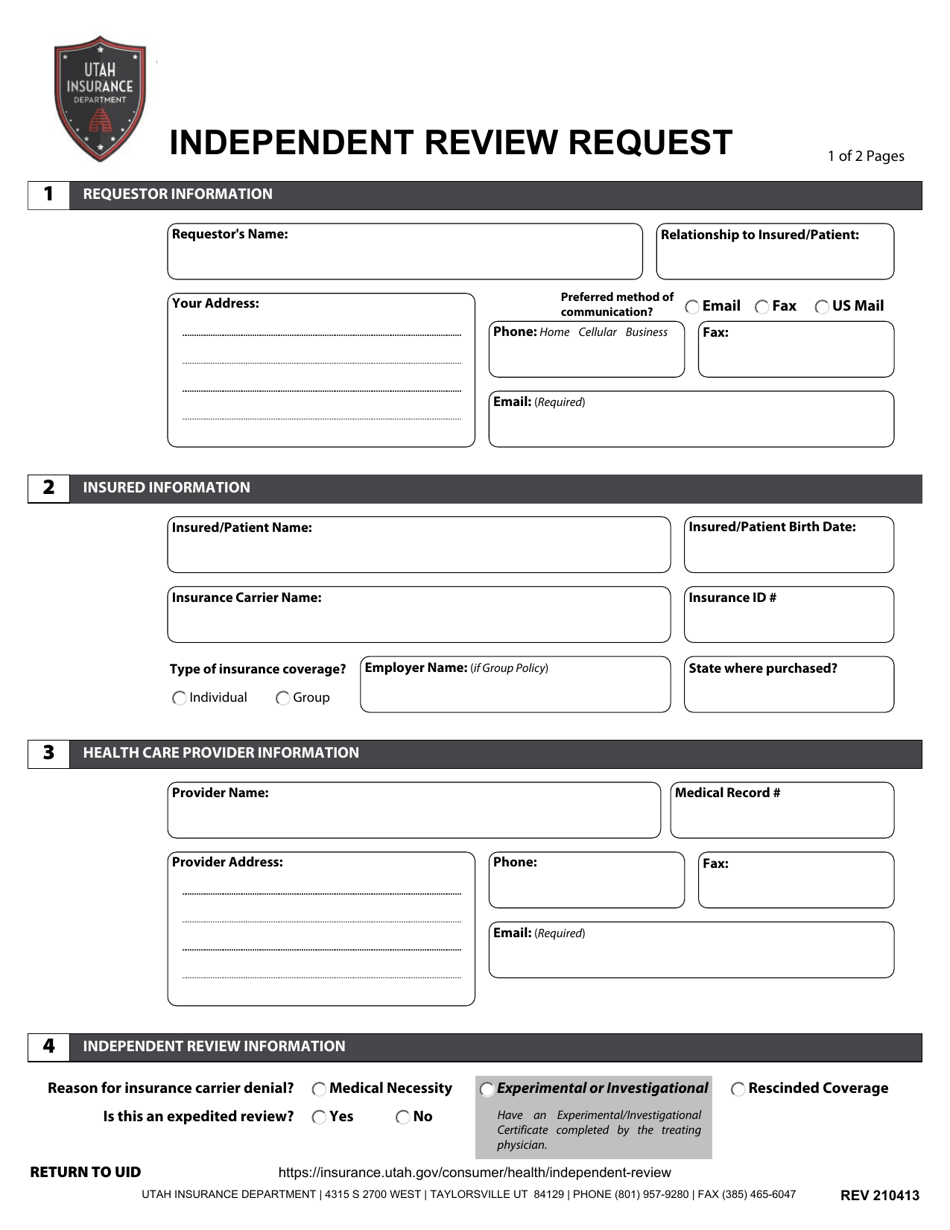
Q: Who can submit an Independent Review Request in Utah?
A: Any insured individual or their authorized representative can submit an Independent Review Request in Utah.
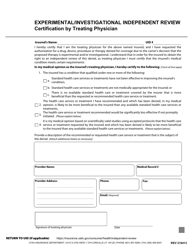
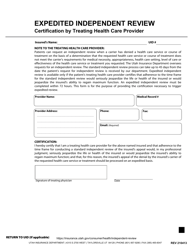
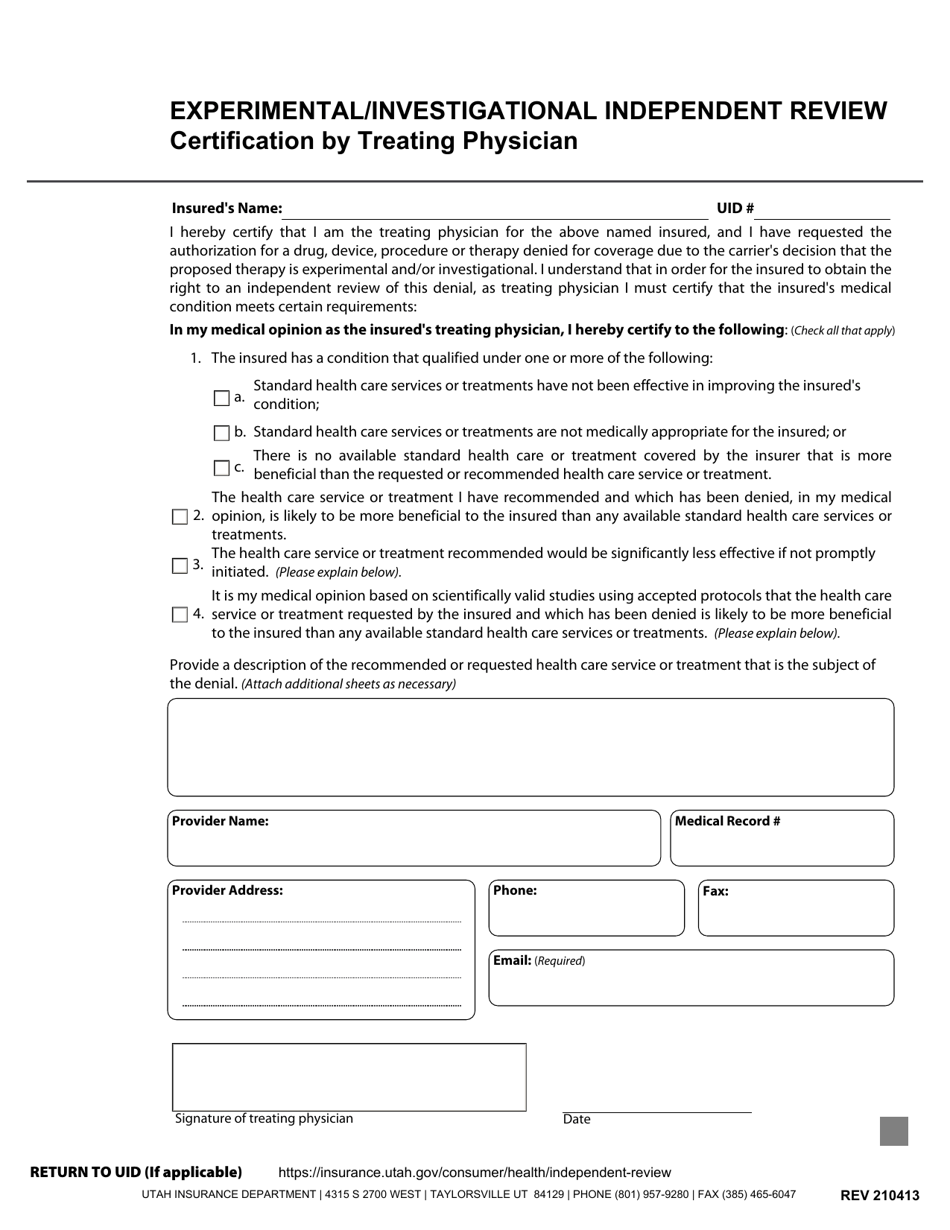
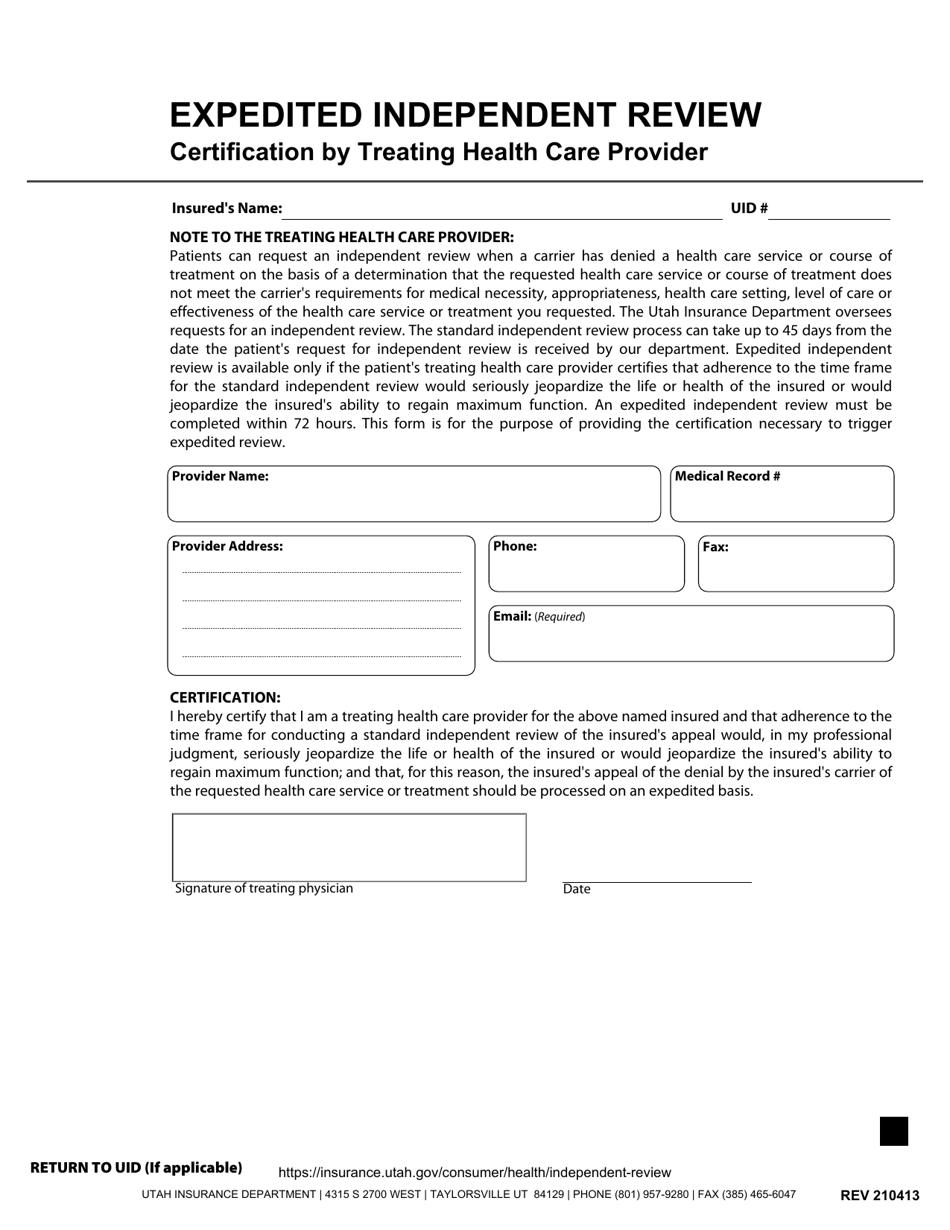
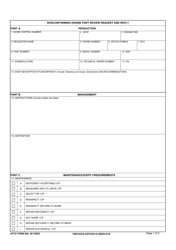
Q: What types of denials can be appealed through an Independent Review Request?
A: Any denial or decision by a health insurance company regarding the medical necessity, appropriateness, or quality of care can be appealed.
Q: Is there a deadline for submitting an Independent Review Request in Utah?
A: Yes, you must submit an Independent Review Request within 30 days of receiving the denial or decision from your health insurance company.
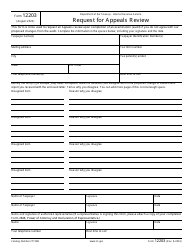
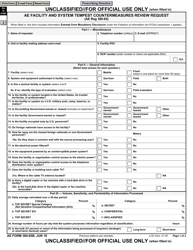
Q: Who conducts the Independent Review in Utah?
A: Independent reviews in Utah are conducted by third-party reviewers selected by the Utah Insurance Department.
Q: What happens after an Independent Review Request is submitted?
A: After submitting an Independent Review Request, you will receive a written decision from the reviewer within a specified timeframe.
Q: Is the decision of the Independent Review binding?
A: Yes, the decision of the Independent Review is binding on the health insurance company, but not on the insured individual.
Q: Can I seek legal assistance during the Independent Review process?
A: Yes, you have the right to seek legal assistance or representation during the Independent Review process in Utah.
Q: Can I file a complaint if I believe the Independent Review was not conducted properly?
A: Yes, you can file a complaint with the Utah Insurance Department if you believe the Independent Review was not conducted properly.
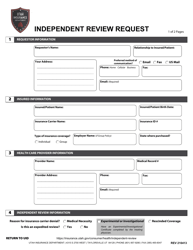
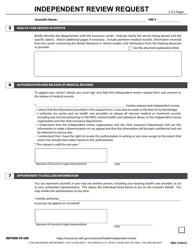
Form Details:
- Released on April 13, 2021;
- The latest edition currently provided by the Utah Insurance Department;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Utah Insurance Department.