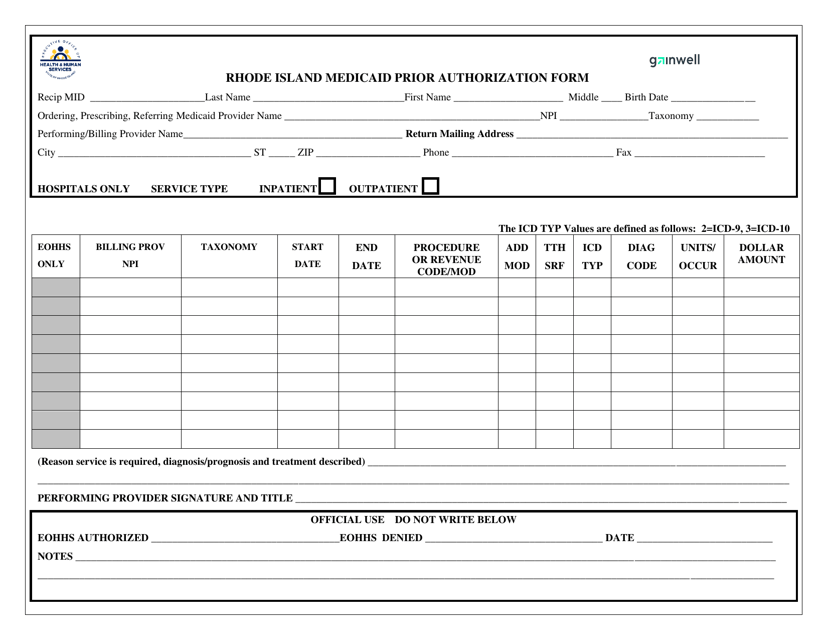
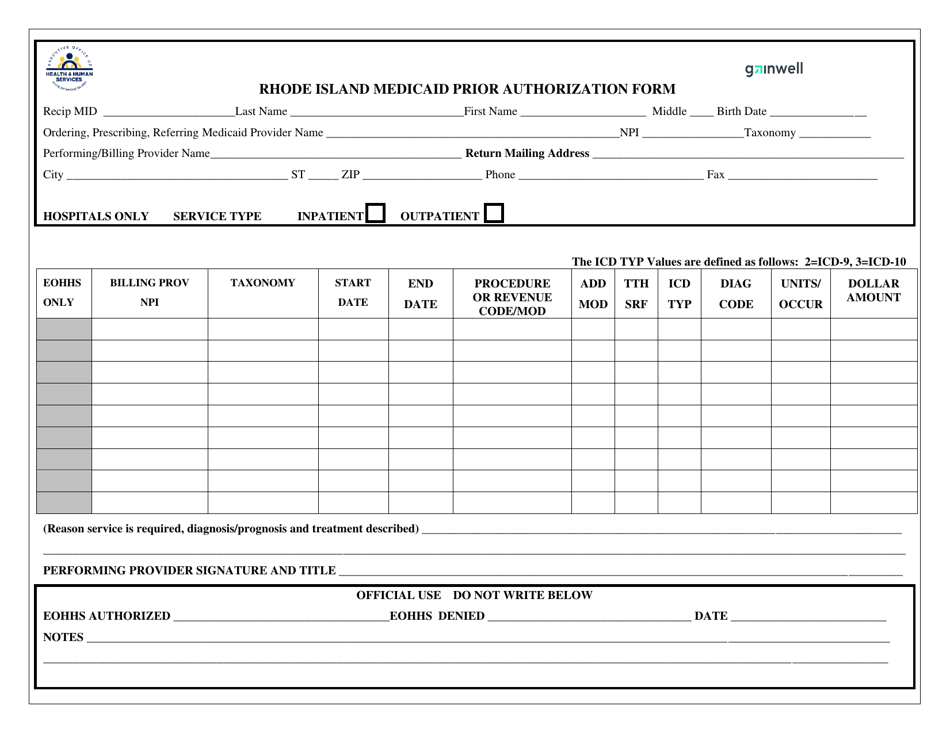
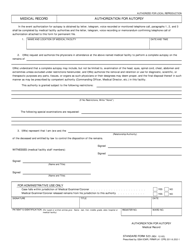
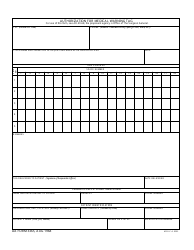
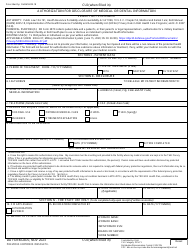
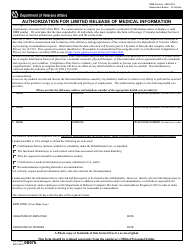
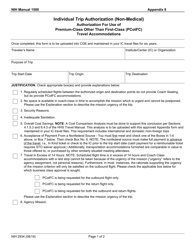
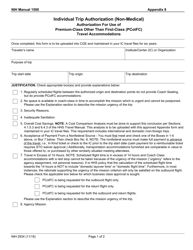
Rhode Island Medicaid Prior Authorization Form - Rhode Island
Rhode Island Medicaid Prior Authorization Form is a legal document that was released by the Rhode Island Executive Office of Health and Human Services - a government authority operating within Rhode Island.
FAQ
Q: What is the Rhode Island Medicaid Prior Authorization Form?
A: The Rhode Island Medicaid Prior Authorization Form is a document that must be completed by healthcare providers to request approval for certain medical services or medications for Medicaid recipients.
Q: Who needs to complete the Rhode Island Medicaid Prior Authorization Form?
A: Healthcare providers that treat Medicaid recipients must complete the Rhode Island Medicaid Prior Authorization Form.
Q: What is the purpose of the Rhode Island Medicaid Prior Authorization Form?
A: The purpose of the Rhode Island Medicaid Prior Authorization Form is to obtain approval for specific medical services or medications for Medicaid recipients.
Q: What information is required on the Rhode Island Medicaid Prior Authorization Form?
A: The Rhode Island Medicaid Prior Authorization Form requires information such as the patient's Medicaid ID, the requested service or medication, and supporting clinical documentation.
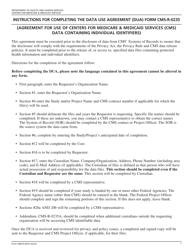
Q: What happens after the Rhode Island Medicaid Prior Authorization Form is submitted?
A: After the Rhode Island Medicaid Prior Authorization Form is submitted, the request is reviewed by the Medicaid program to determine if the requested service or medication meets the program's criteria for coverage.
Q: How long does it take to process a Rhode Island Medicaid Prior Authorization request?
A: The processing time for a Rhode Island Medicaid Prior Authorization request can vary, but it generally takes up to 10 business days.
Form Details:
- The latest edition currently provided by the Rhode Island Executive Office of Health and Human Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Rhode Island Executive Office of Health and Human Services.