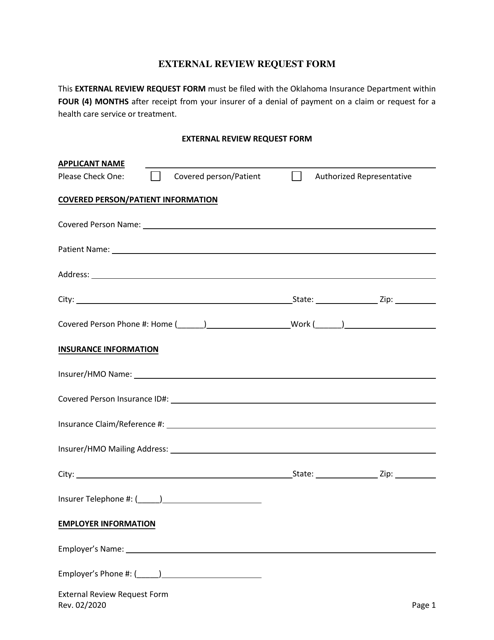
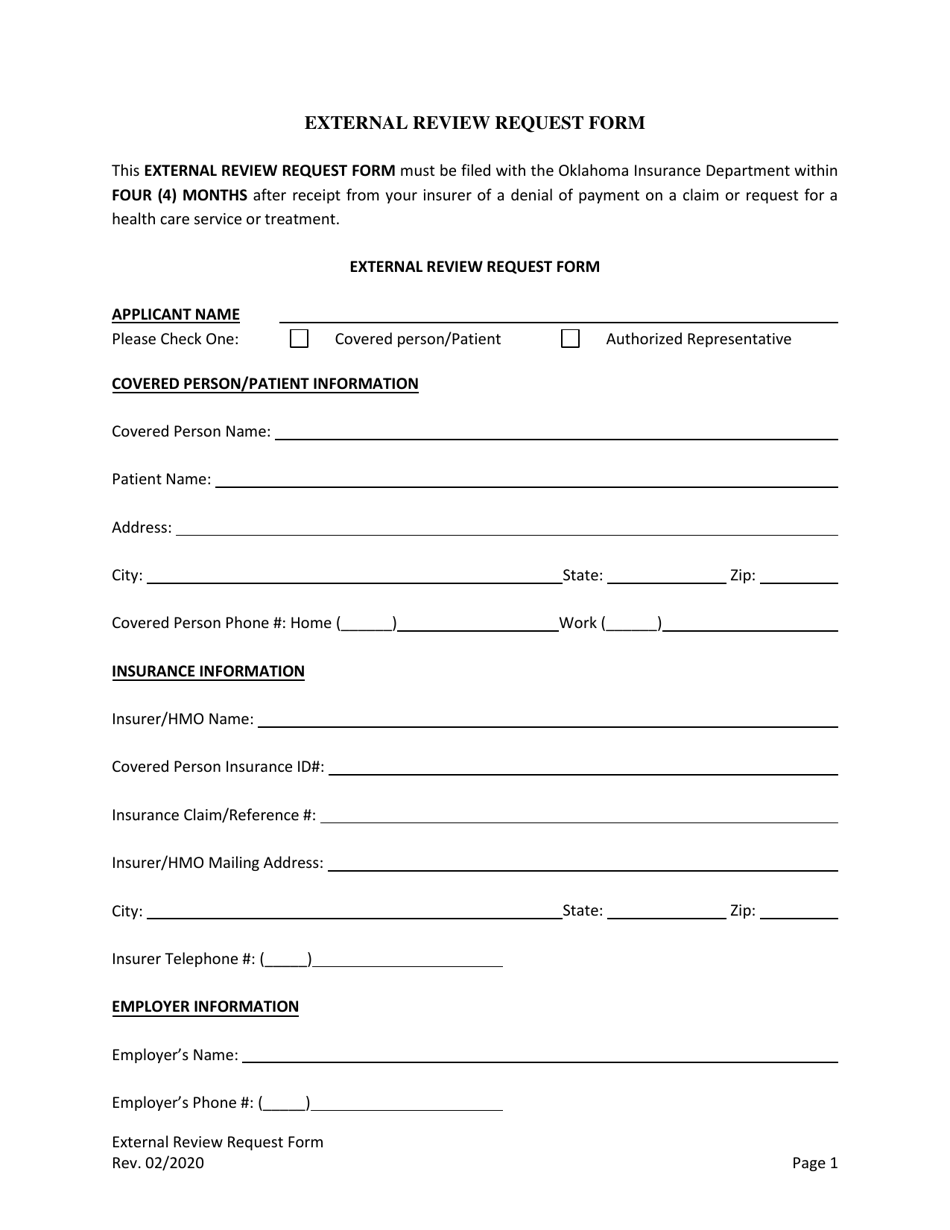
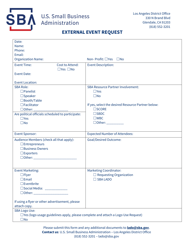
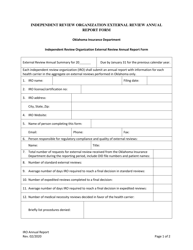
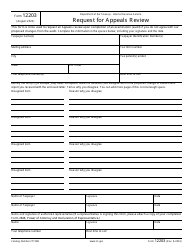
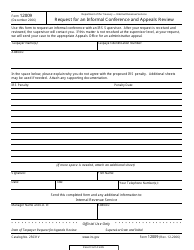
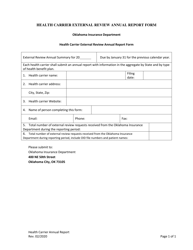
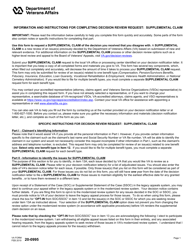
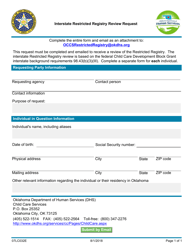
External Review Request Form - Oklahoma
External Review Request Form is a legal document that was released by the Oklahoma Insurance Department - a government authority operating within Oklahoma.
FAQ
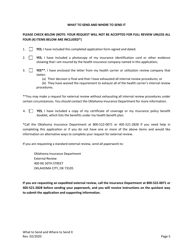
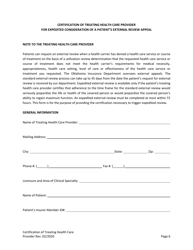
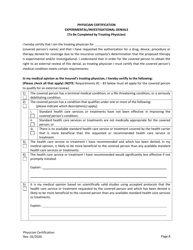
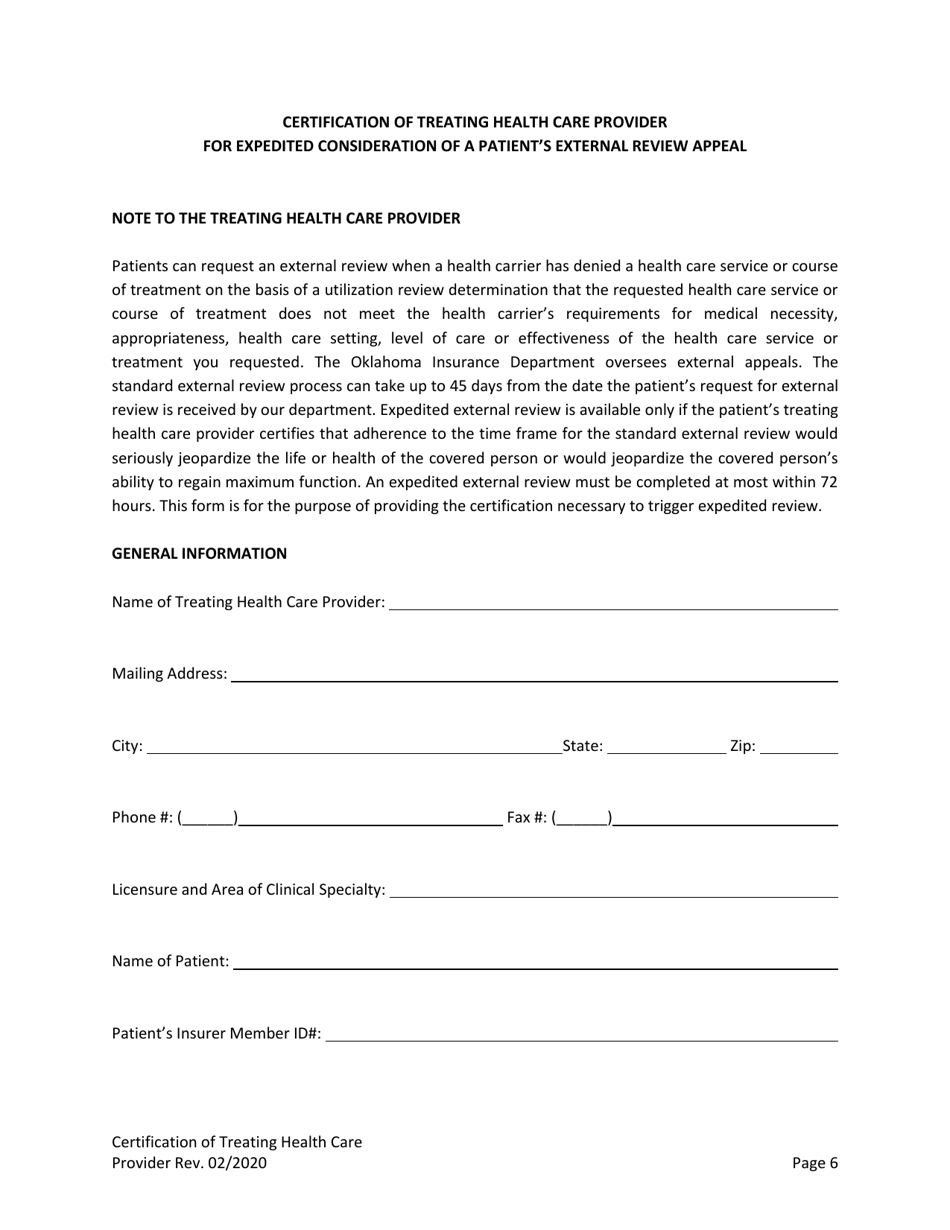
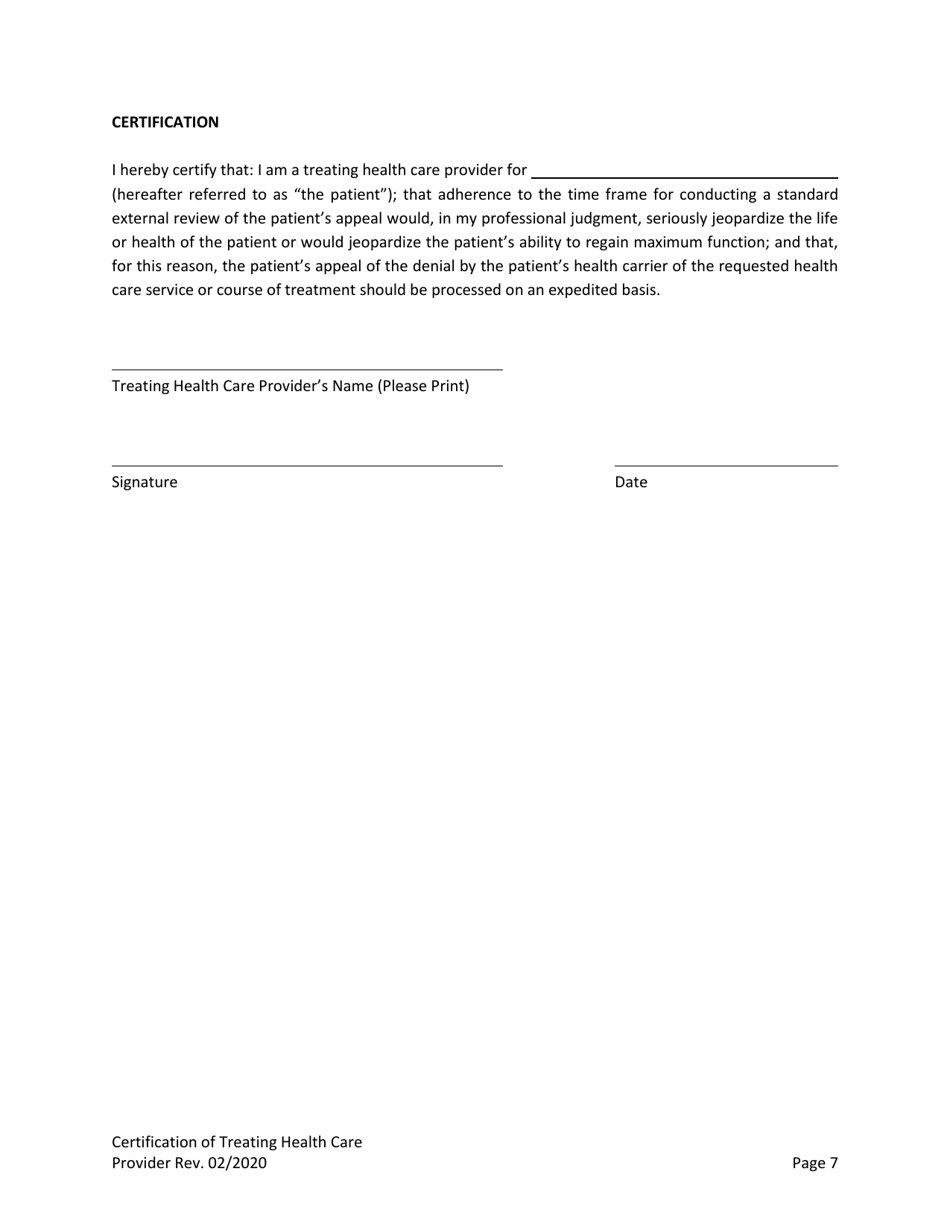
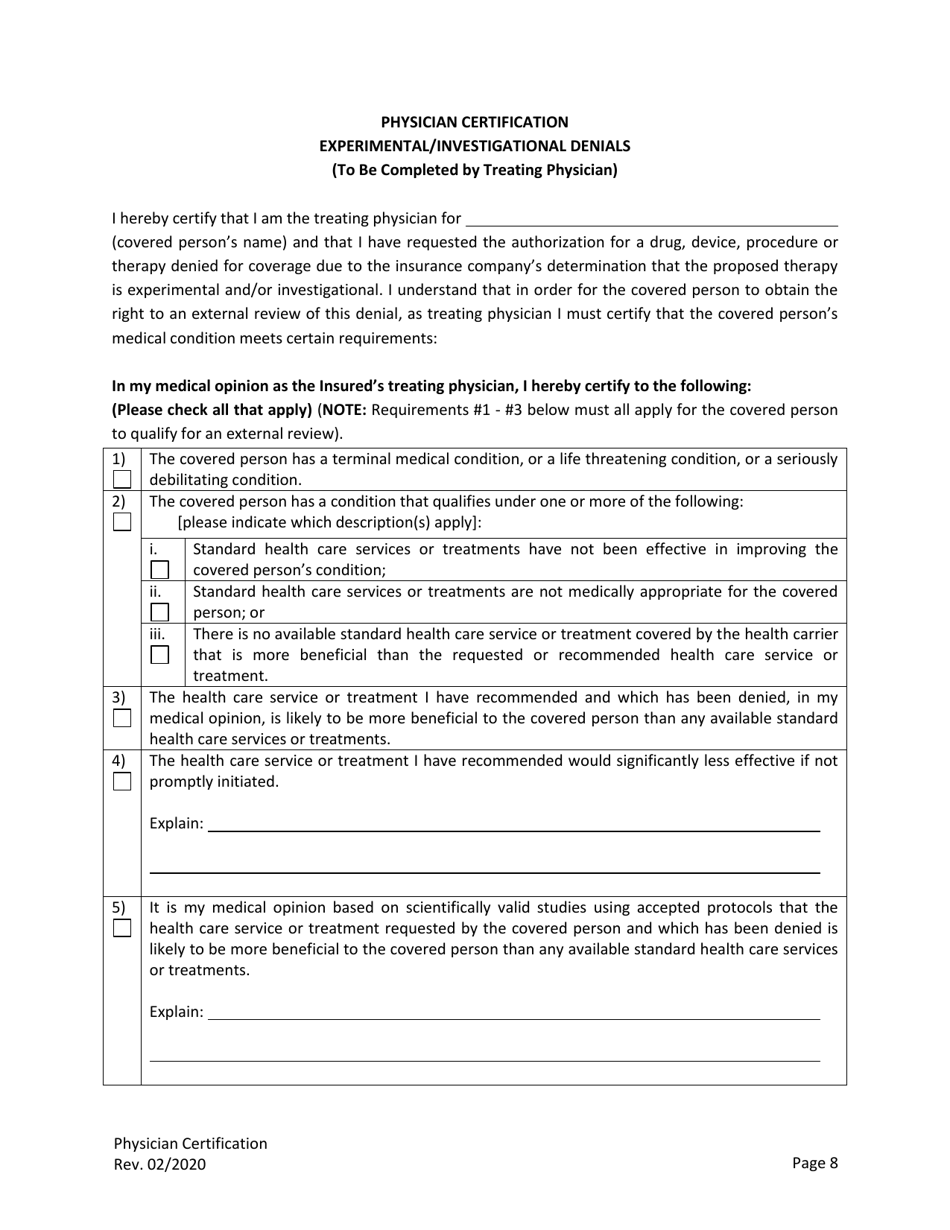
Q: What is the purpose of the External Review Request Form?
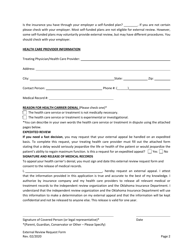
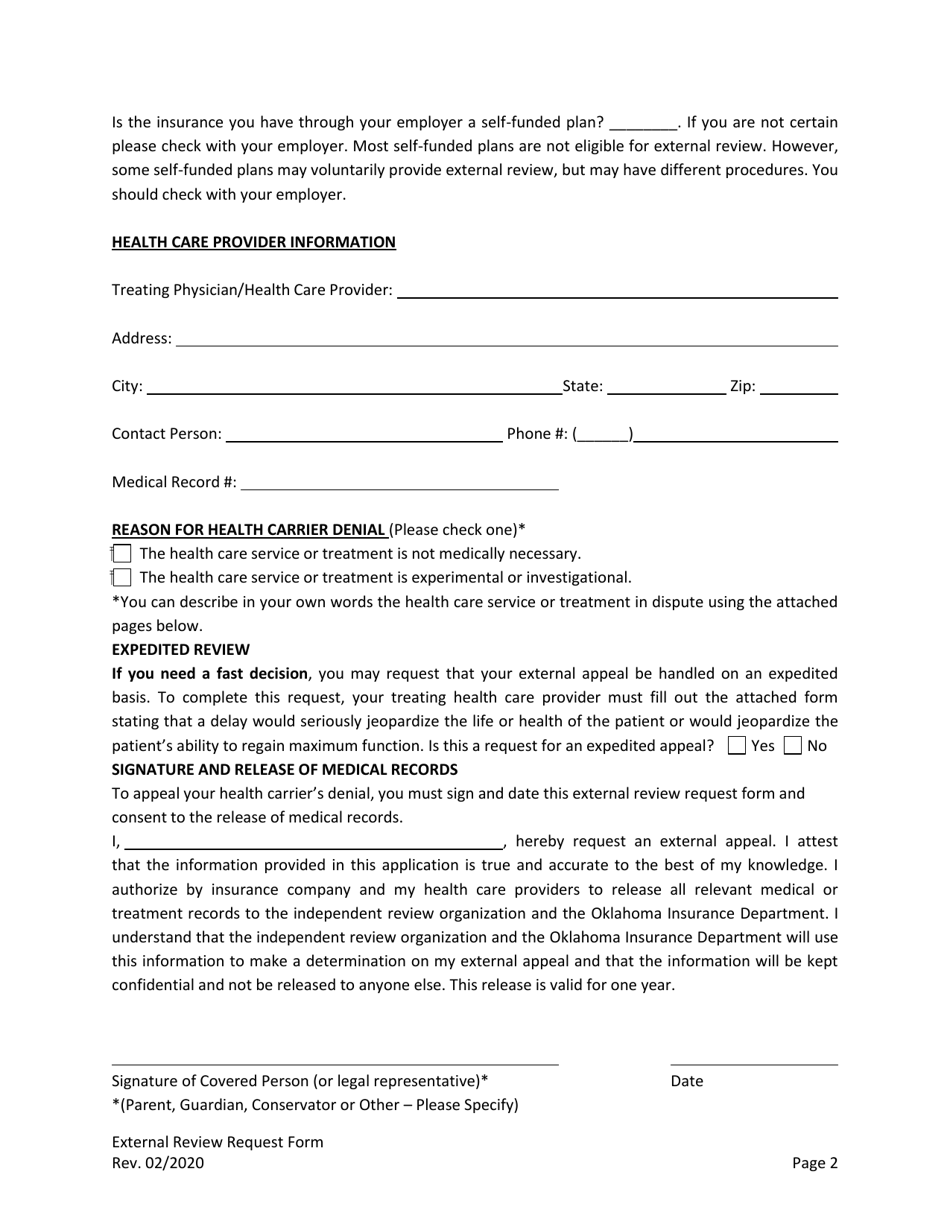
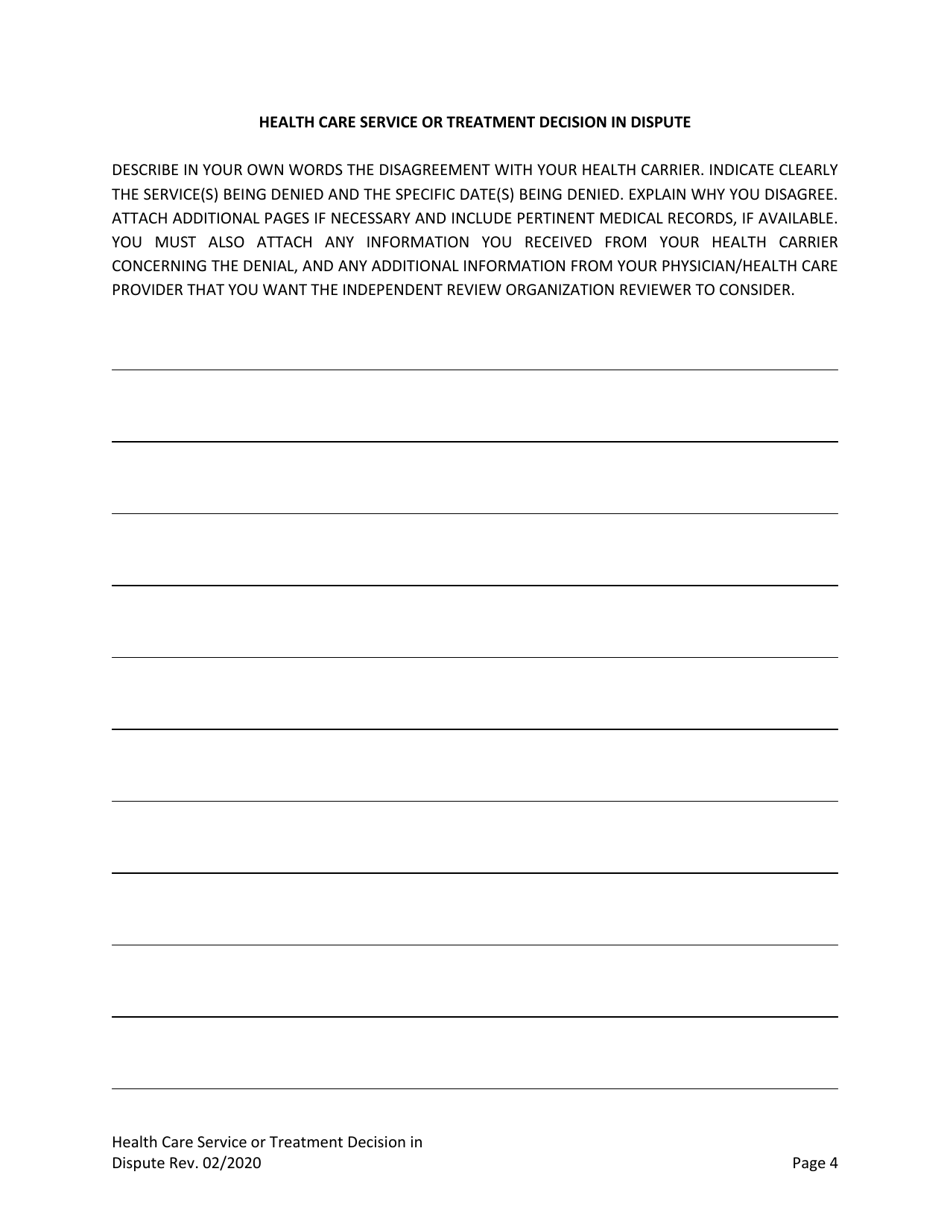
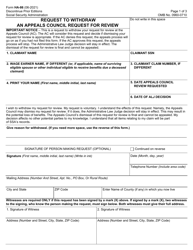
A: The form is used to request a review of a denied health insurance claim by an external independent reviewer.
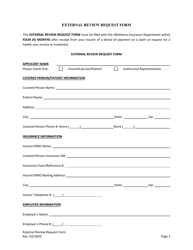
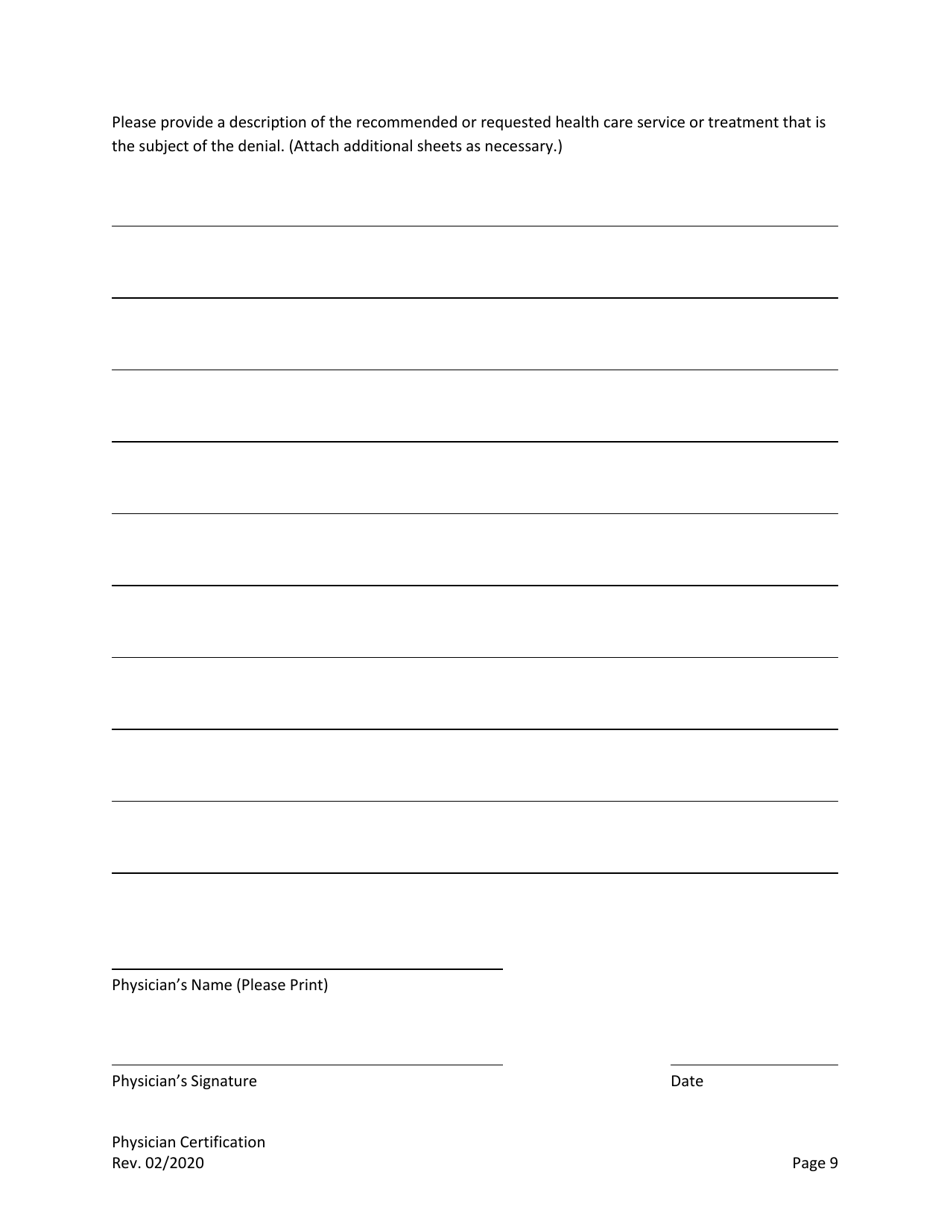
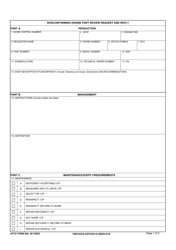
Q: What information do I need to provide on the form?
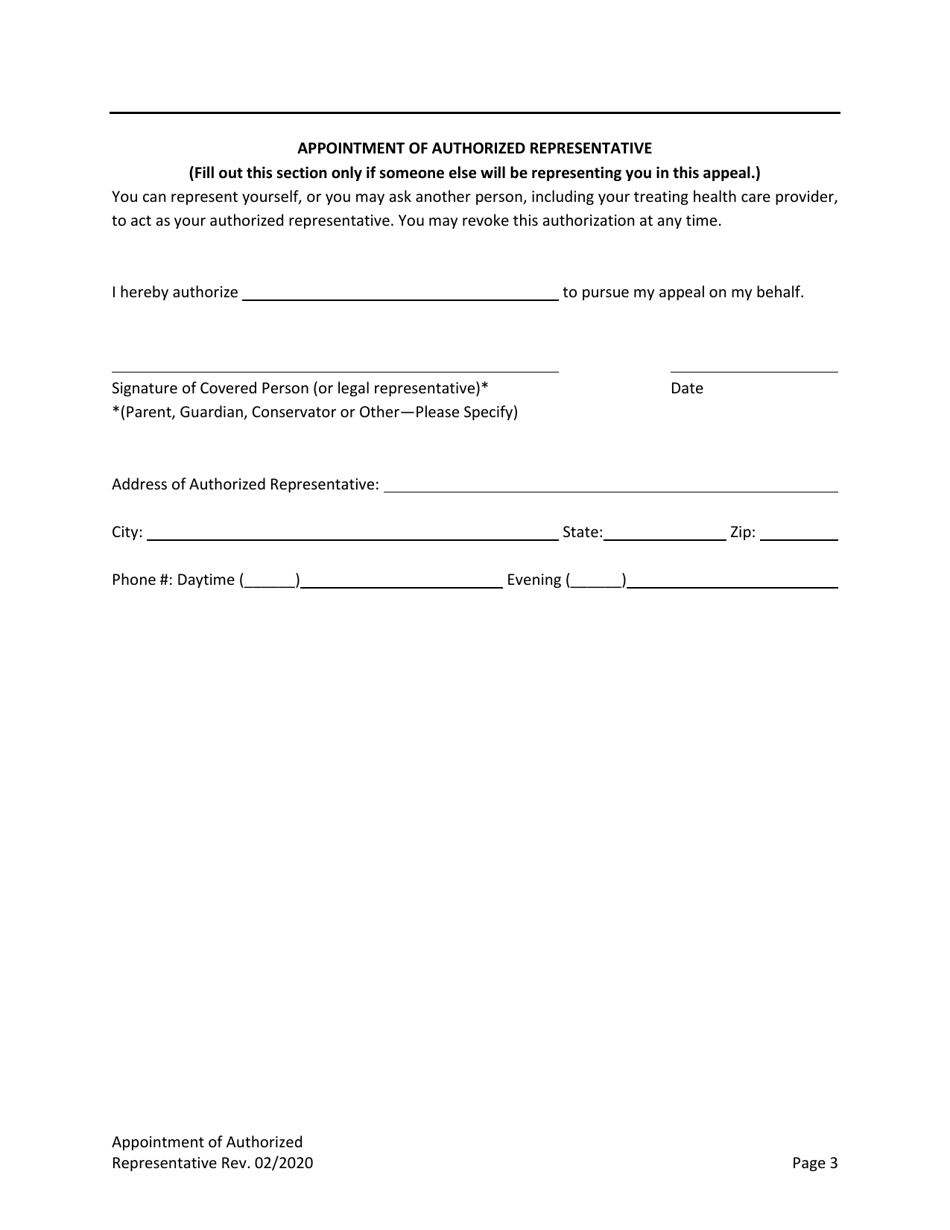
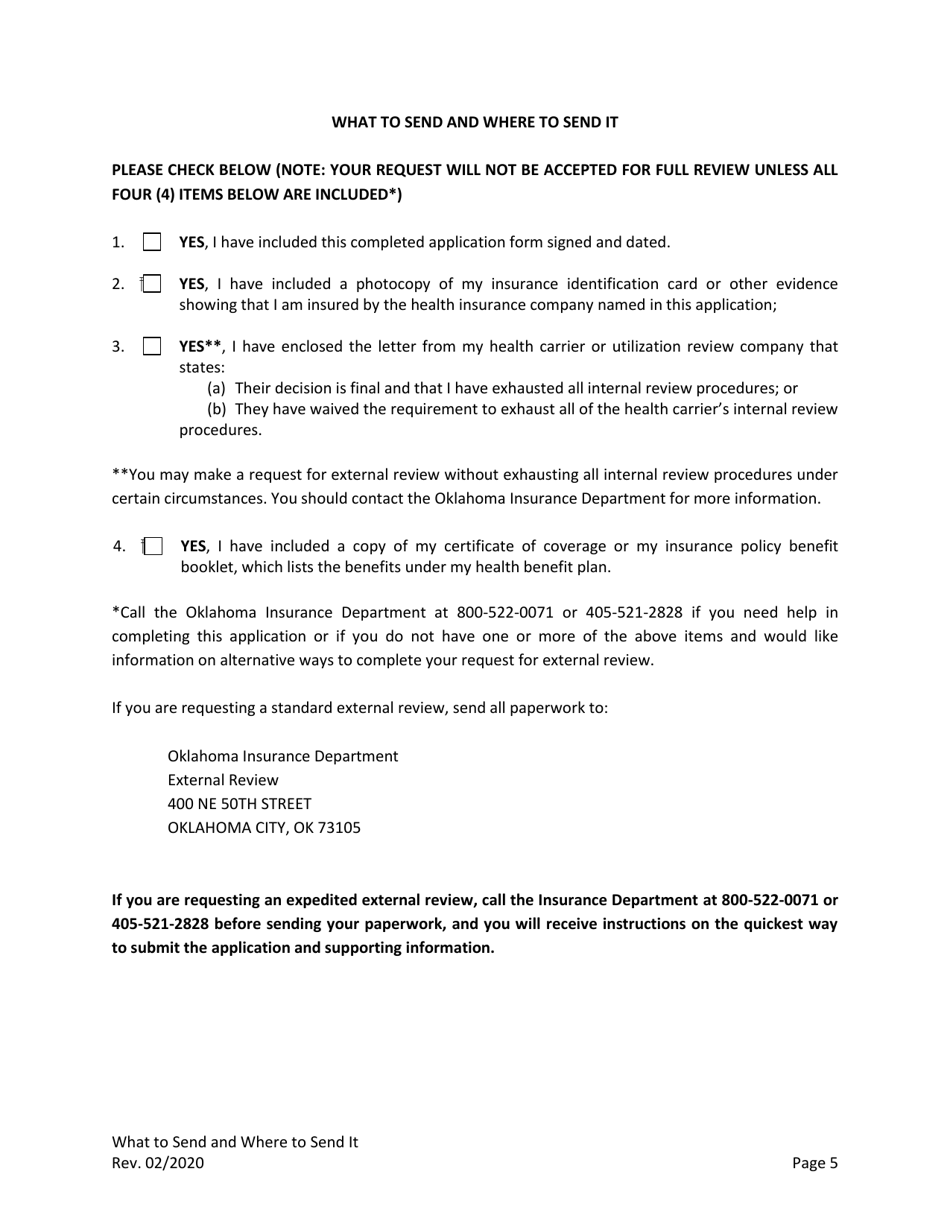
A: You will need to provide your personal information, insurance policy details, and a summary of the denial or dispute.
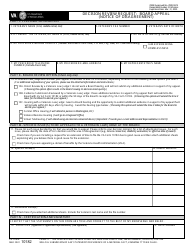
Q: Is there a deadline to submit the External Review Request Form?
A: Yes, you must submit the form within 60 days of receiving the final adverse benefit determination notice.
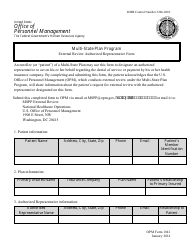
Q: Who is eligible to file an external review request?
A: Any person covered by a health insurance policy in Oklahoma who has received a denial of coverage or payment can file a request.
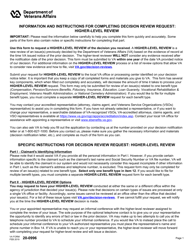
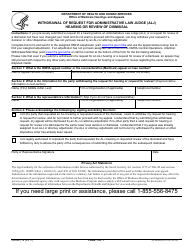
Q: What happens after I submit the External Review Request Form?
A: The external independent reviewer will evaluate your case and make a recommendation to the insurance company on whether to uphold or reverse the denial.
Q: How long does the external review process take?
A: The process typically takes 45 days from the receipt of your request for an expedited review or 60 days for a standard review.
Q: Is the decision of the external independent reviewer final?
A: Yes, the decision made by the external reviewer is binding on the insurance company, and they must abide by it.
Q: Are there any fees associated with filing an external review request?
A: No, there are no fees to file the request or for the external review process.
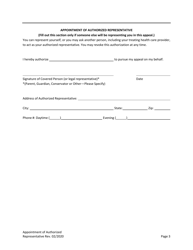
Q: Can I seek legal representation during the external review process?
A: Yes, you have the right to seek legal assistance or enlist the help of a consumer assistance program during the review process.
Form Details:
- Released on February 1, 2020;
- The latest edition currently provided by the Oklahoma Insurance Department;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Oklahoma Insurance Department.