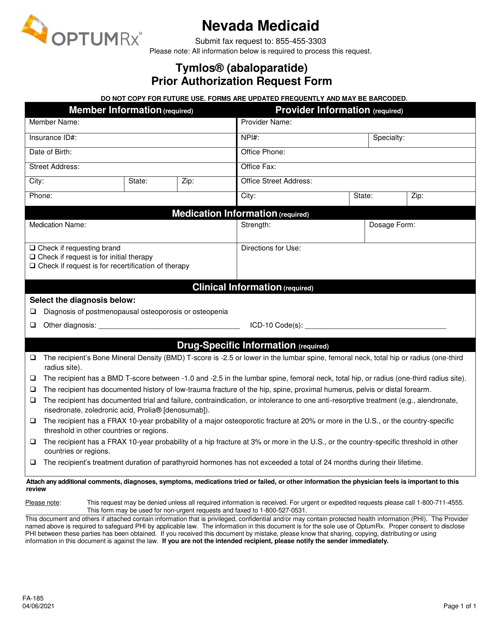
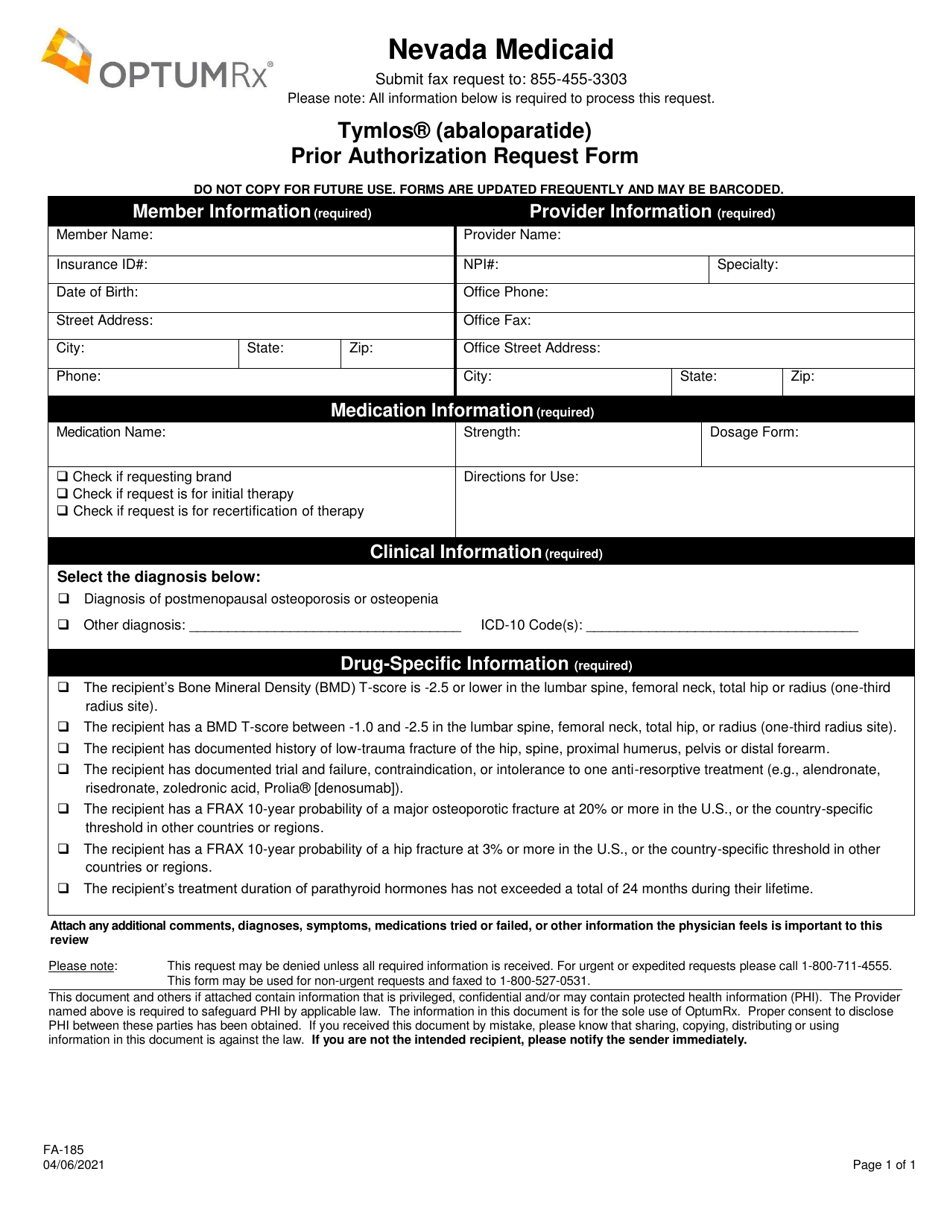
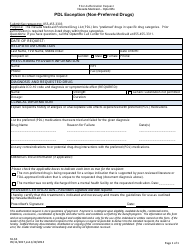
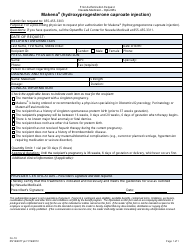
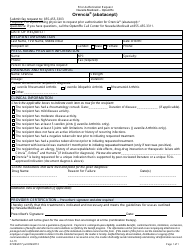
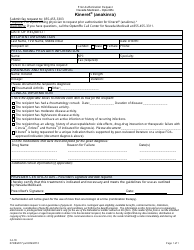
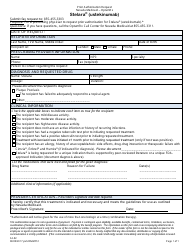
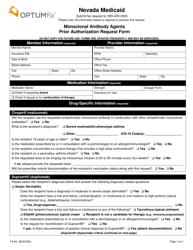
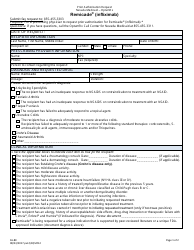
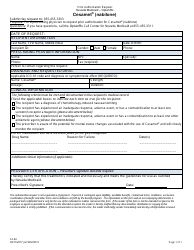
Form FA-185 Tymlos (Abaloparatide) Prior Authorization Request Form - Nevada
What Is Form FA-185?
This is a legal form that was released by the Nevada Department of Health and Human Services - a government authority operating within Nevada. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is the Form FA-185 Tymlos (Abaloparatide) Prior Authorization Request Form?
A: It is a form used to request prior authorization for the medication Tymlos (Abaloparatide) in Nevada.
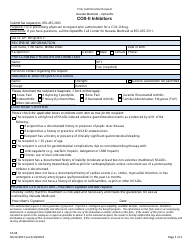
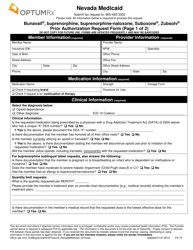
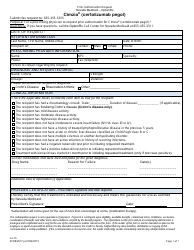
Q: What is Tymlos (Abaloparatide)?
A: Tymlos (Abaloparatide) is a medication used to treat osteoporosis in postmenopausal women at high risk of fracture.
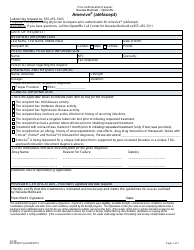
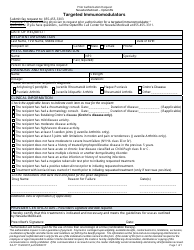
Q: What is prior authorization?
A: Prior authorization is a process where a healthcare provider must get approval from an insurance company before prescribing a specific medication or treatment.
Q: Why is prior authorization required?
A: Insurance companies require prior authorization to ensure that medications or treatments are medically necessary and appropriate.
Q: Who needs to complete the Form FA-185 Tymlos (Abaloparatide) Prior Authorization Request Form?
A: Healthcare providers who want to prescribe Tymlos (Abaloparatide) in Nevada need to complete this form.
Q: What information is required on the Form FA-185 Tymlos (Abaloparatide) Prior Authorization Request Form?
A: The form requires information about the patient, healthcare provider, diagnosis, and the medical necessity for prescribing Tymlos (Abaloparatide).
Q: How long does it take to get a response for a prior authorization request?
A: The time to get a response for a prior authorization request can vary, but it is usually within a few business days.
Q: What happens if the prior authorization request is denied?
A: If the prior authorization request is denied, the healthcare provider and patient can work together to explore other treatment options or appeal the decision.
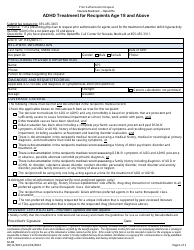
Q: Is prior authorization always required for Tymlos (Abaloparatide)?
A: Not necessarily. Prior authorization requirements may vary depending on the insurance plan and individual circumstances. It's best to check with the insurance company or healthcare provider.
Q: Are there any alternatives to Tymlos (Abaloparatide)?
A: Yes, there are other medications available for the treatment of osteoporosis in postmenopausal women. Your healthcare provider can discuss the options with you.
Form Details:
- Released on April 6, 2021;
- The latest edition provided by the Nevada Department of Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of Form FA-185 by clicking the link below or browse more documents and templates provided by the Nevada Department of Health and Human Services.