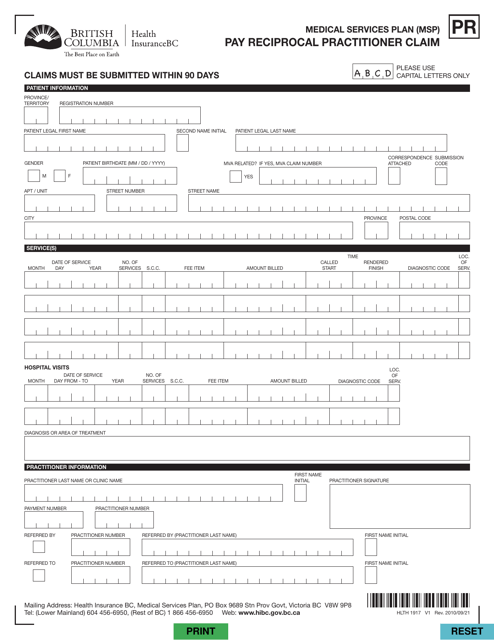
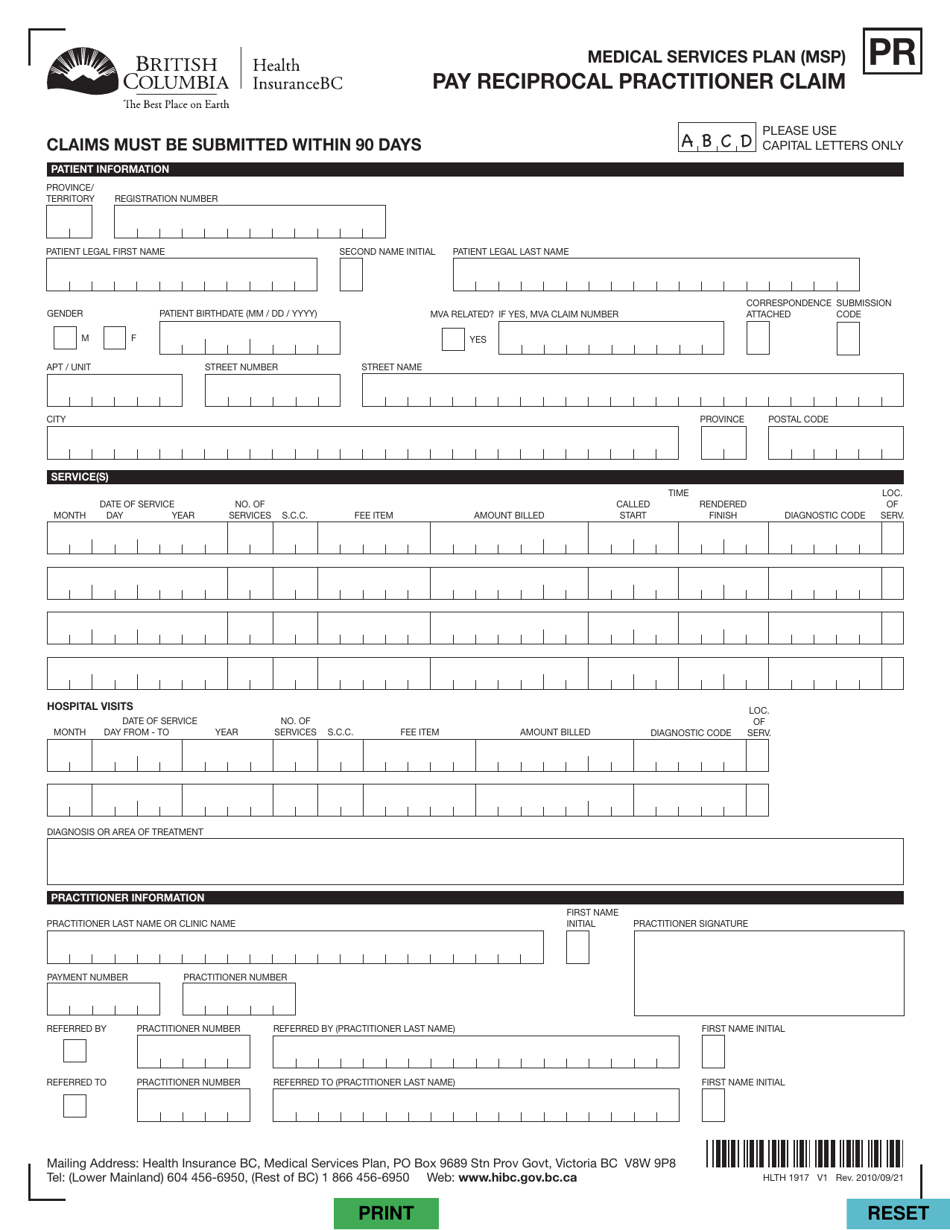
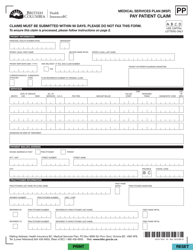
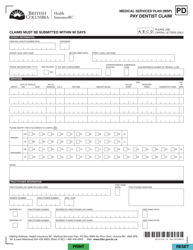
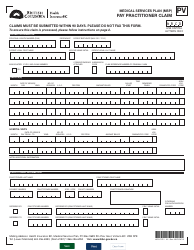
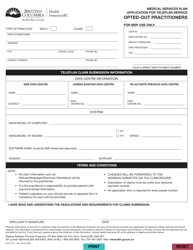
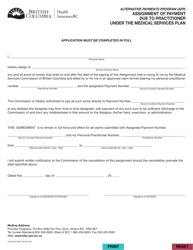
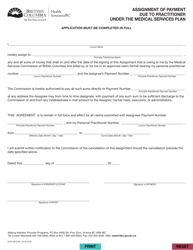
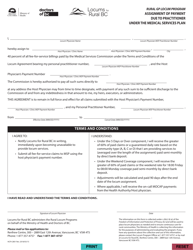
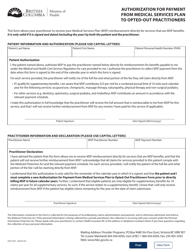
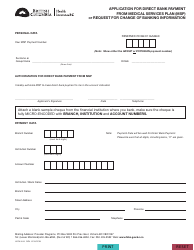
Form HLTH1917 Medical Services Plan (Msp) Pay Reciprocal Practitioner Claim - British Columbia, Canada
The Form HLTH1917 Medical Services Plan (MSP) Pay Reciprocal Practitioner Claim is used in British Columbia, Canada to submit claims for reciprocal practitioners who have provided medical services to residents covered under the MSP.
The Form HLTH1917 Medical Services Plan (MSP) Pay Reciprocal Practitioner Claim in British Columbia, Canada is typically filed by reciprocal practitioners who provide medical services to MSP beneficiaries.
FAQ
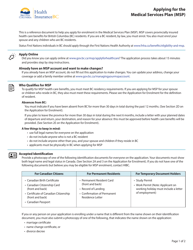
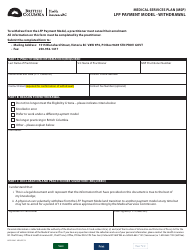
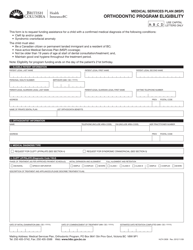
Q: What is the Medical Services Plan (MSP) in British Columbia, Canada?
A: The Medical Services Plan (MSP) is the provincial health insurance program in British Columbia, Canada.
Q: What is the purpose of MSP?
A: The purpose of MSP is to provide access to medically necessary health care services for eligible residents of British Columbia.
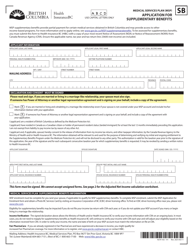
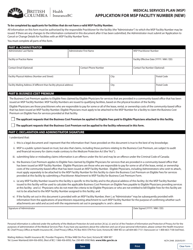
Q: What is a reciprocal practitioner claim?
A: A reciprocal practitioner claim is a claim for medical services provided by a healthcare practitioner from another province or territory in Canada.
Q: How do I pay a reciprocal practitioner claim under MSP?
A: To pay a reciprocal practitioner claim under MSP, you need to complete and submit the HLTH 1917 form.
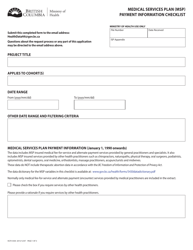
Q: Do I need to provide any supporting documents with the HLTH 1917 form?
A: Yes, you need to attach all relevant invoices and receipts supporting the medical services provided by the reciprocal practitioner.
Q: What is the deadline for submitting a reciprocal practitioner claim under MSP?
A: The reciprocal practitioner claim should be submitted within 90 days from the date of service.
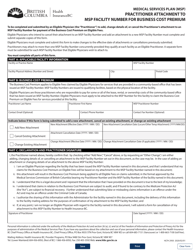
Q: How long does it take to process a reciprocal practitioner claim under MSP?
A: The processing time for a reciprocal practitioner claim under MSP can vary, but it usually takes several weeks.
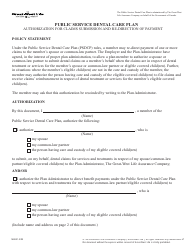
Q: Can I receive reimbursement for the full cost of the medical services?
A: No, under MSP, there may be certain limitations and eligibility requirements that determine the amount of reimbursement.
Q: Who is eligible for MSP coverage?
A: Residents of British Columbia who meet the eligibility criteria are eligible for MSP coverage.