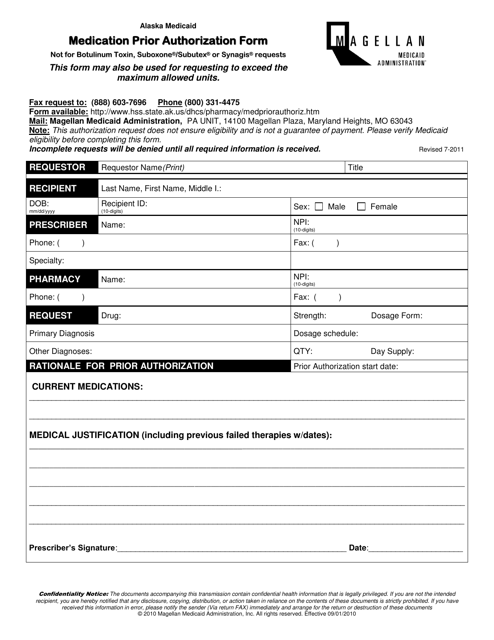
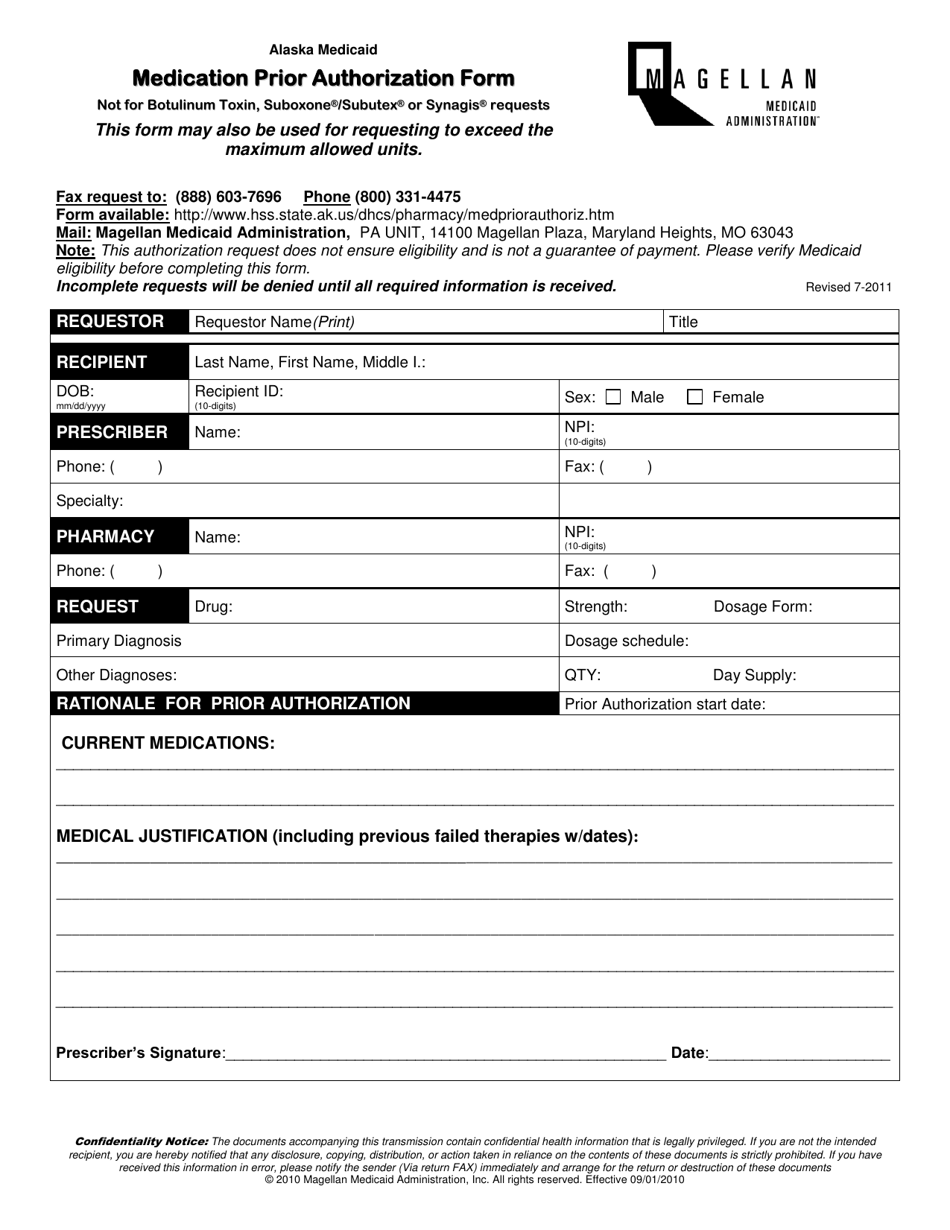
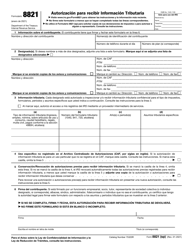
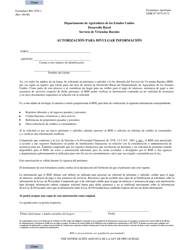
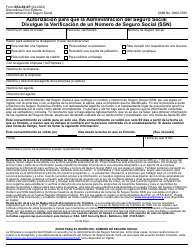
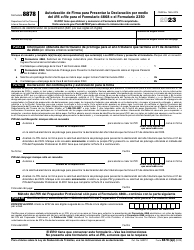
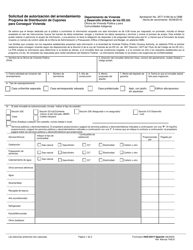
Medication Prior Authorization Form - Alaska
Medication Prior Authorization Form is a legal document that was released by the Alaska Department of Health and Social Services - a government authority operating within Alaska.
FAQ
Q: What is a Prior Authorization Form?
A: A Prior Authorization Form is a document used by healthcare providers to request approval from insurance companies for specific medications.
Q: Why is a Prior Authorization Form needed?
A: Insurance companies require a Prior Authorization Form to ensure that medications prescribed are necessary and appropriate.
Q: Who needs to complete the Prior Authorization Form?
A: The healthcare provider who is prescribing the medication needs to complete the Prior Authorization Form.
Q: What information is required on the Prior Authorization Form?
A: The Prior Authorization Form typically requires information such as patient demographics, medical diagnosis, medication details, and supporting documentation.
Q: How long does it take to process a Prior Authorization?
A: The processing time for a Prior Authorization can vary, but it usually takes several business days.
Q: Is there a fee for submitting a Prior Authorization Form?
A: There is usually no fee for submitting a Prior Authorization Form, but it's important to check with your insurance company.
Q: What happens if a Prior Authorization is denied?
A: If a Prior Authorization is denied, the healthcare provider may need to explore alternative medication options or appeal the decision.
Q: Is a Prior Authorization required for every medication?
A: Not every medication requires a Prior Authorization. It depends on the specific medication and your insurance company's guidelines.
Form Details:
- Released on July 1, 2011;
- The latest edition currently provided by the Alaska Department of Health and Social Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Alaska Department of Health and Social Services.