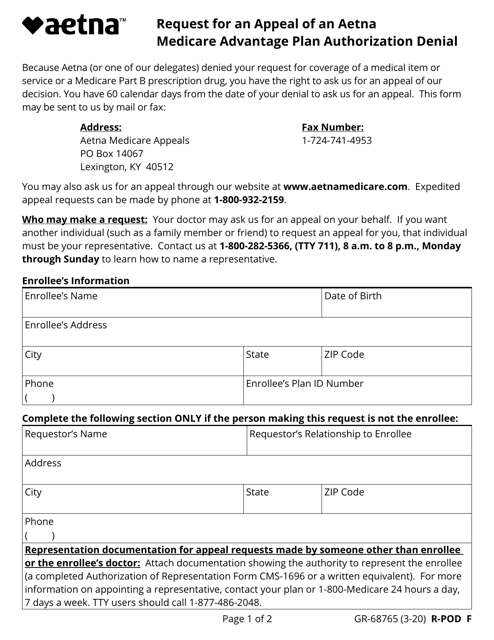
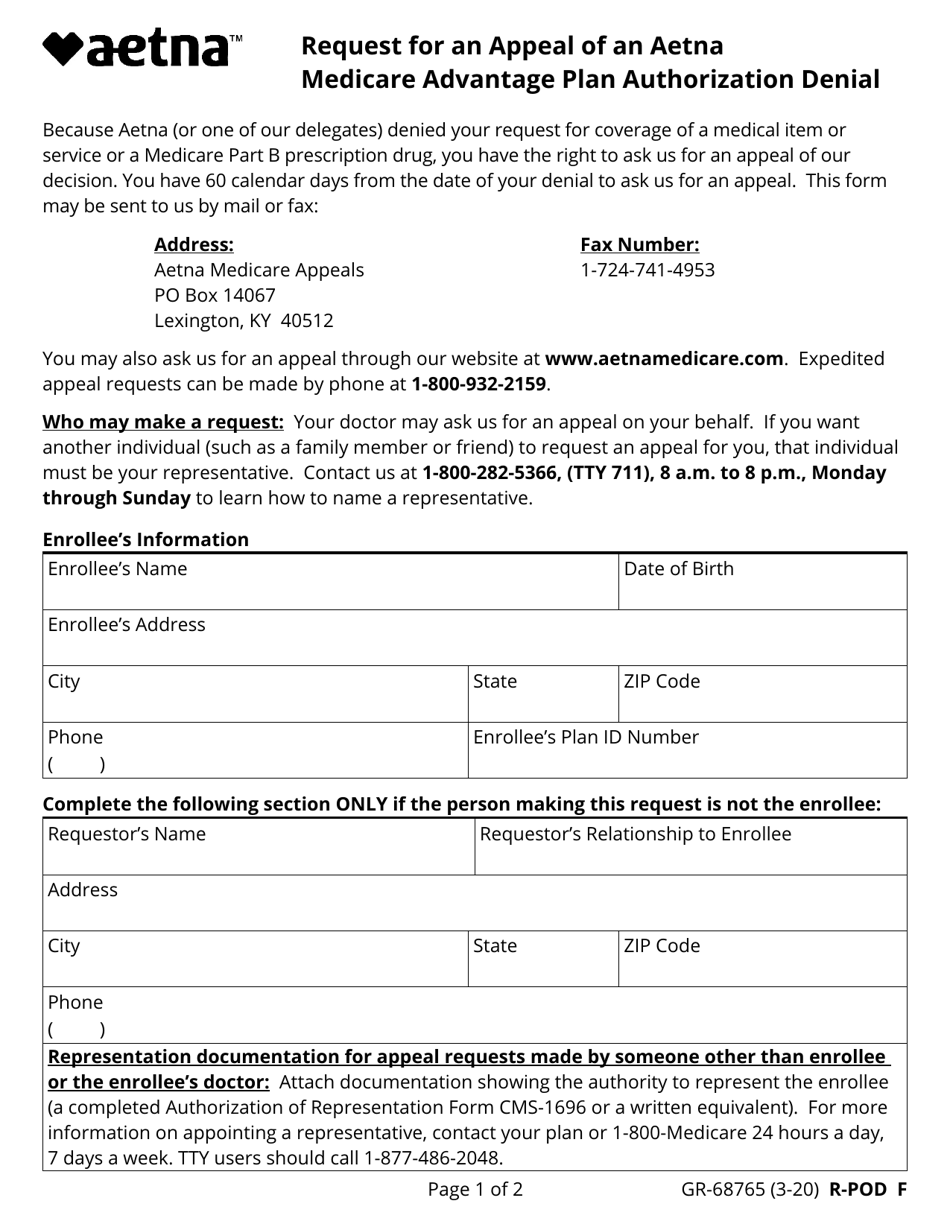
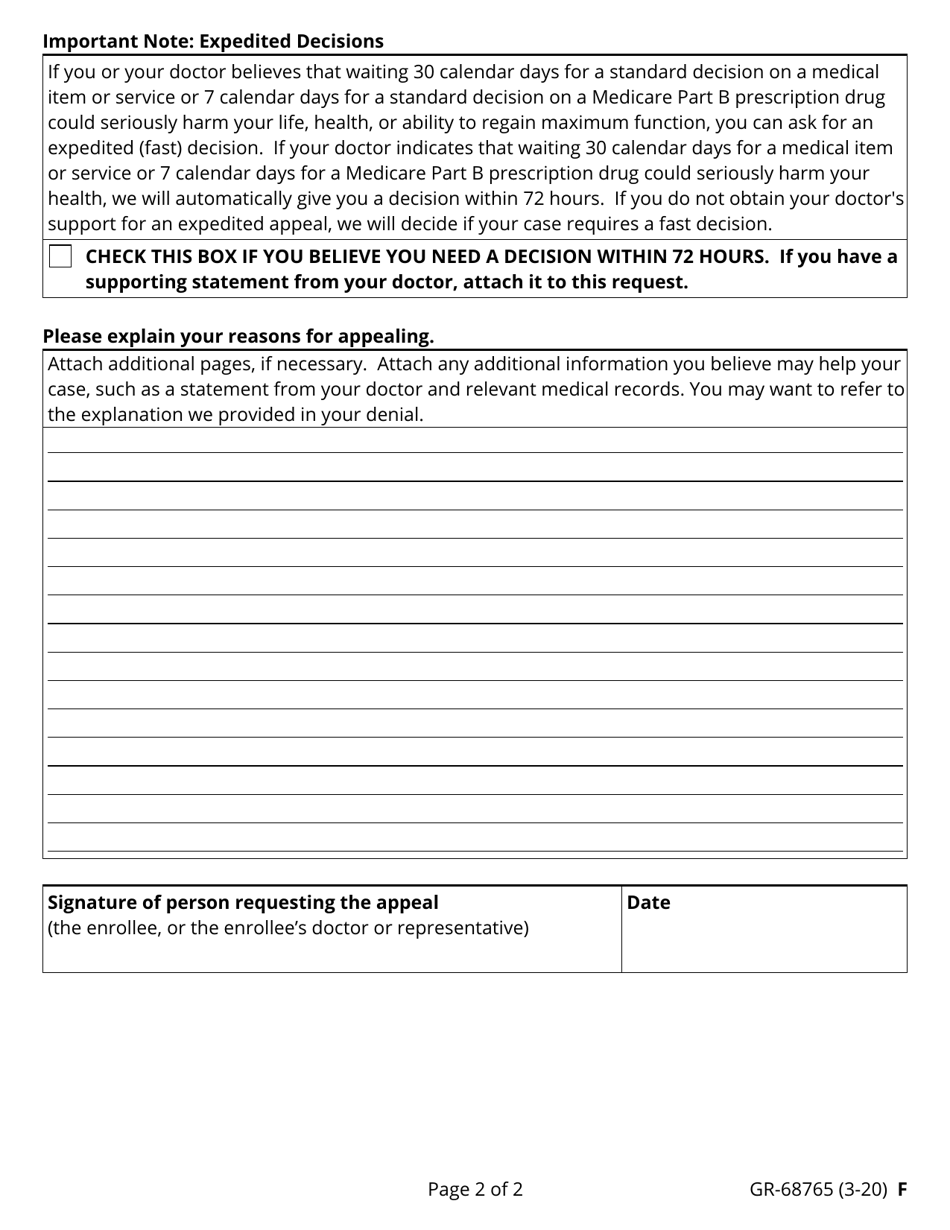
Form GR-68765 Request for an Appeal of an Aetna Medicare Advantage Plan Authorization Denial - Aetna
Form GR-68765 is used to request an appeal of a denial of authorization for an Aetna Medicare Advantage Plan. It allows individuals to request a review of the denial decision and provide additional information or arguments to support their case.
Yes, Aetna files the Form GR-68765 for an appeal of an Aetna Medicare Advantage Plan authorization denial.
FAQ
Q: What is Form GR-68765?
A: Form GR-68765 is a request form for an appeal of an Aetna Medicare Advantage Plan authorization denial.
Q: What is an Aetna Medicare Advantage Plan?
A: An Aetna Medicare Advantage Plan is a type of health insurance plan offered by Aetna for individuals eligible for Medicare.
Q: What does an authorization denial mean?
A: An authorization denial means that Aetna has refused to approve a medical service or treatment requested by the beneficiary.
Q: How can I use Form GR-68765?
A: You can use Form GR-68765 to request an appeal of an Aetna Medicare Advantage Plan authorization denial.
Q: How do I submit Form GR-68765?
A: You can submit Form GR-68765 by mail or fax, as indicated on the form.
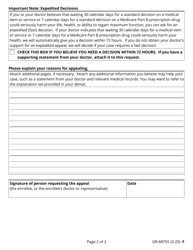
Q: What should I include with Form GR-68765?
A: You should include any relevant documentation or information supporting your appeal, such as medical records or a letter from your healthcare provider.
Q: What happens after I submit Form GR-68765?
A: After you submit Form GR-68765, Aetna will review your appeal and make a decision. You will be notified of the decision in writing.
Q: Can I appeal an Aetna Medicare Advantage Plan authorization denial?
A: Yes, you can appeal an Aetna Medicare Advantage Plan authorization denial by using Form GR-68765.
Q: Is there a deadline for submitting Form GR-68765?
A: Yes, there is a deadline for submitting Form GR-68765. The specific deadline will be provided in the denial letter you received from Aetna.
Q: Can I get help with completing Form GR-68765?
A: Yes, you can contact Aetna customer service for assistance with completing Form GR-68765.