Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics
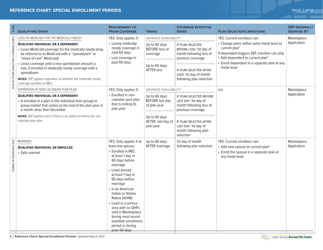
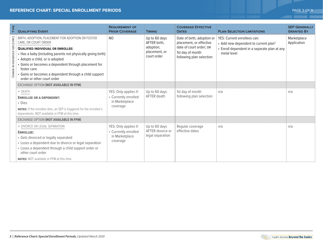
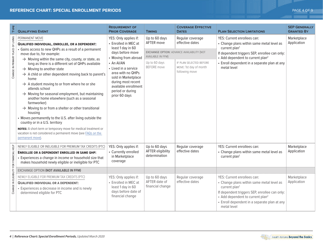
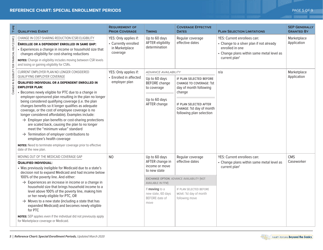
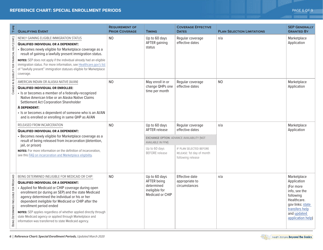
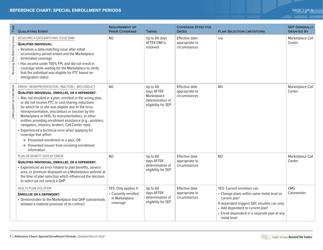
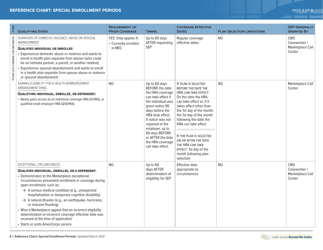
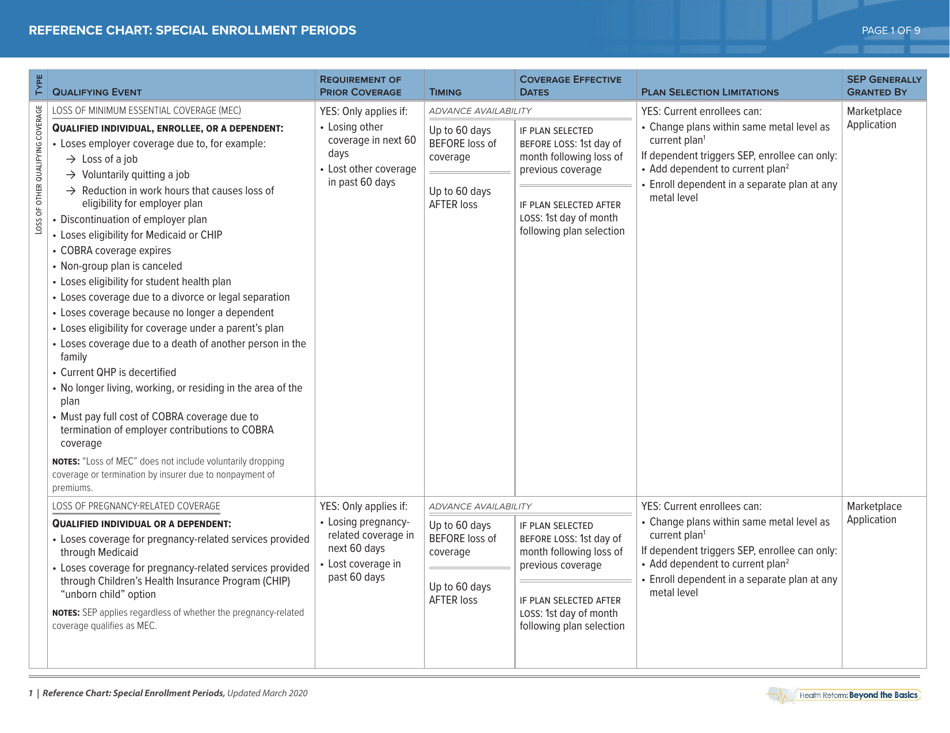
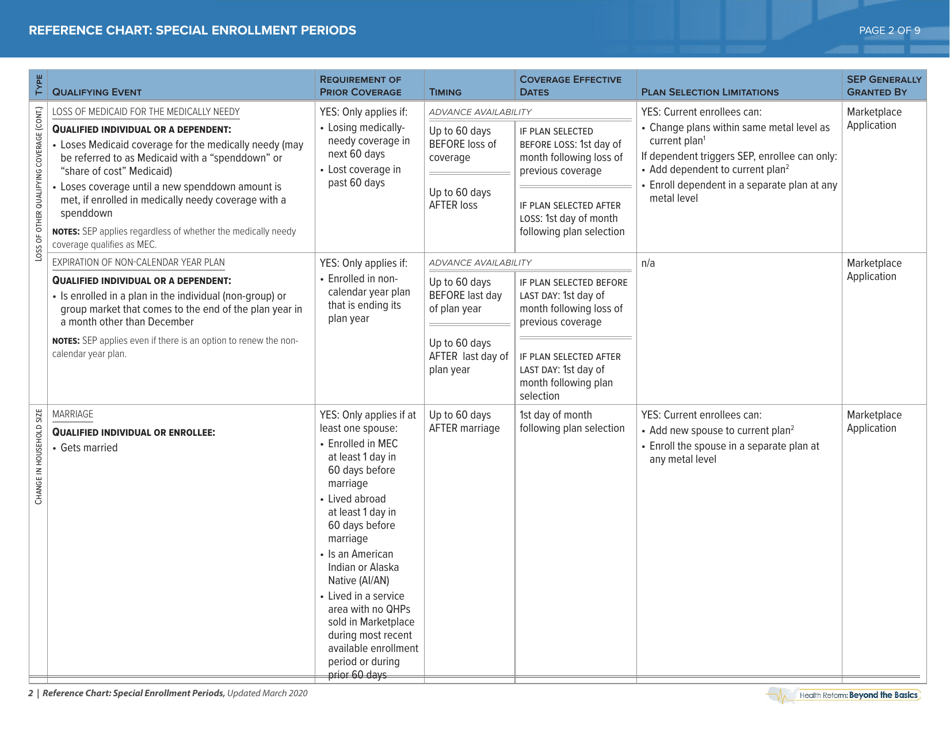
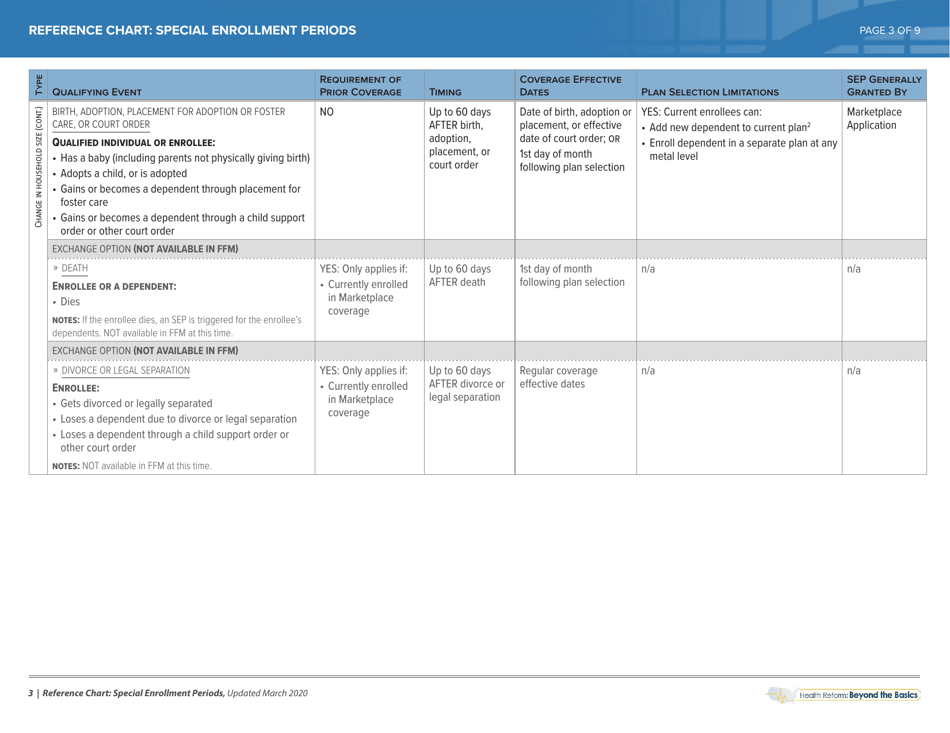
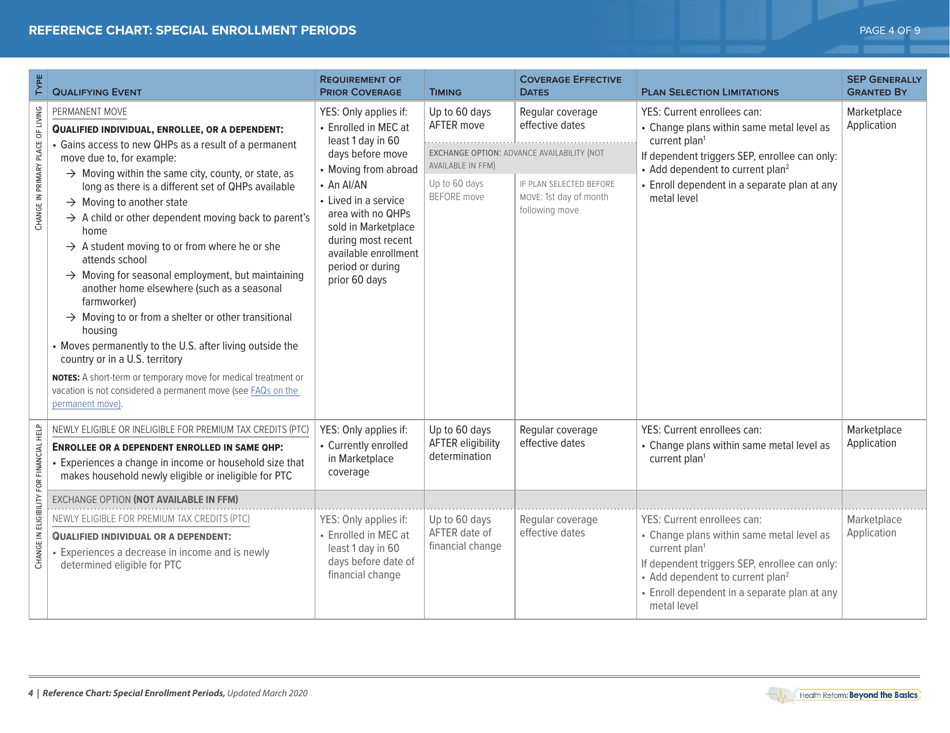
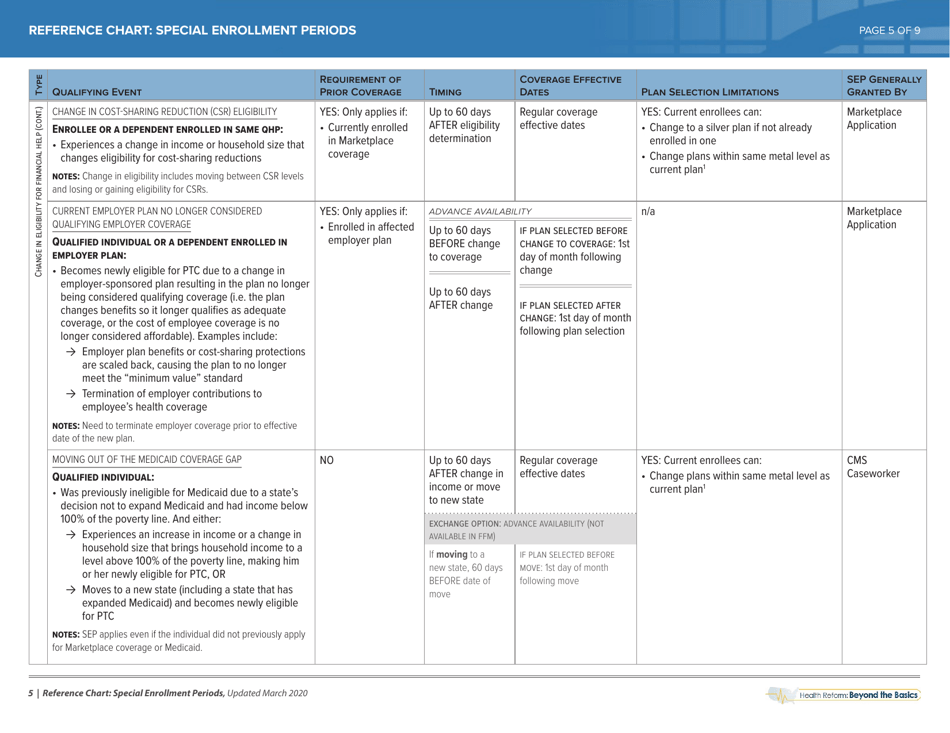
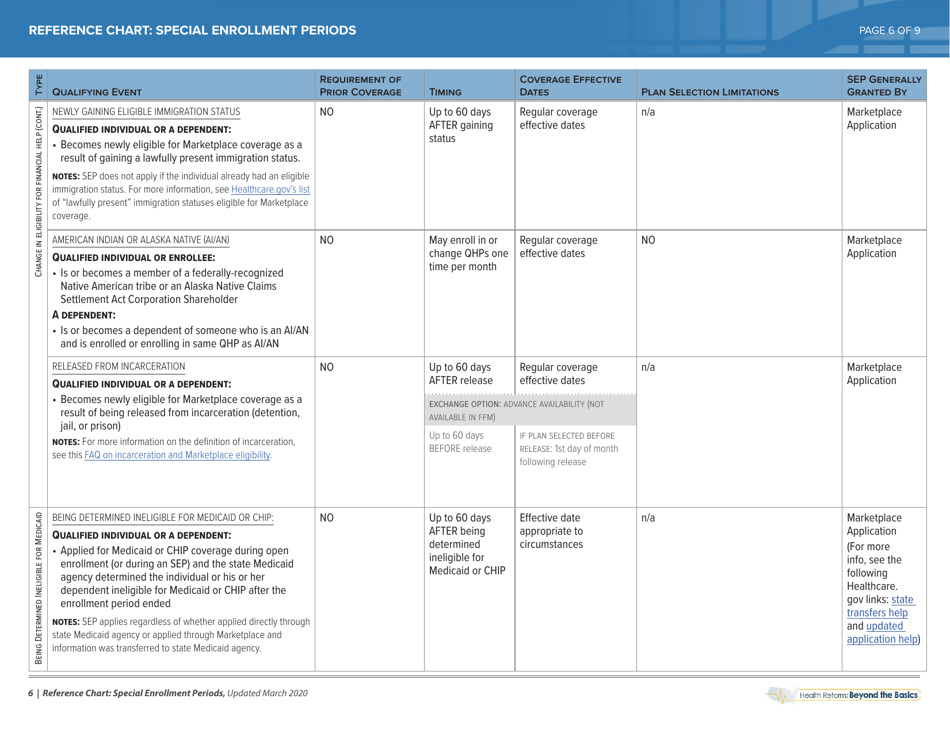
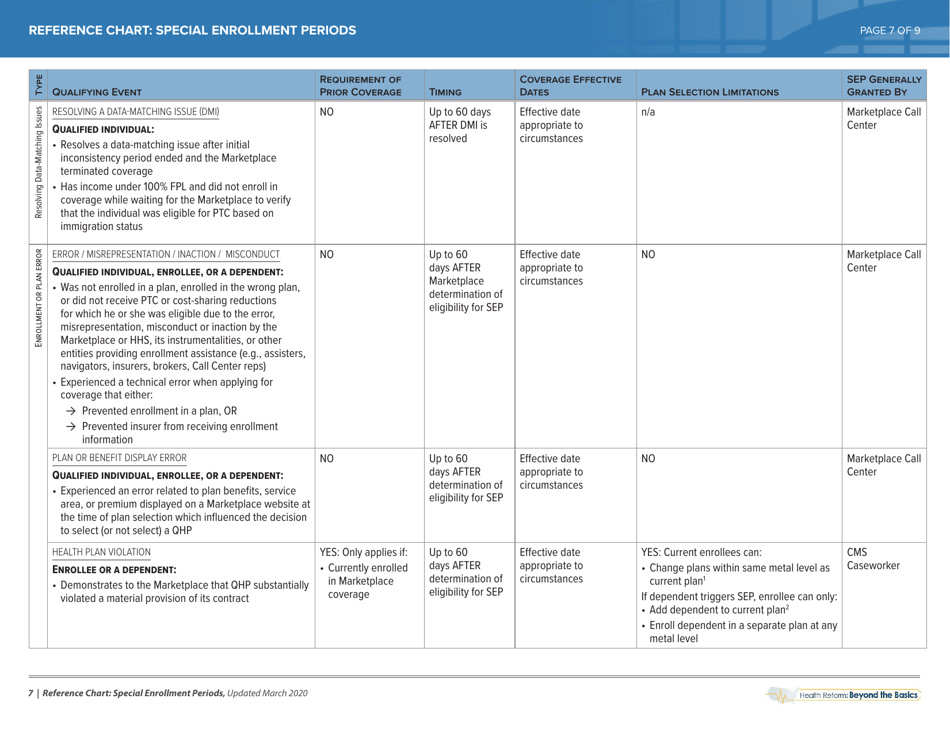
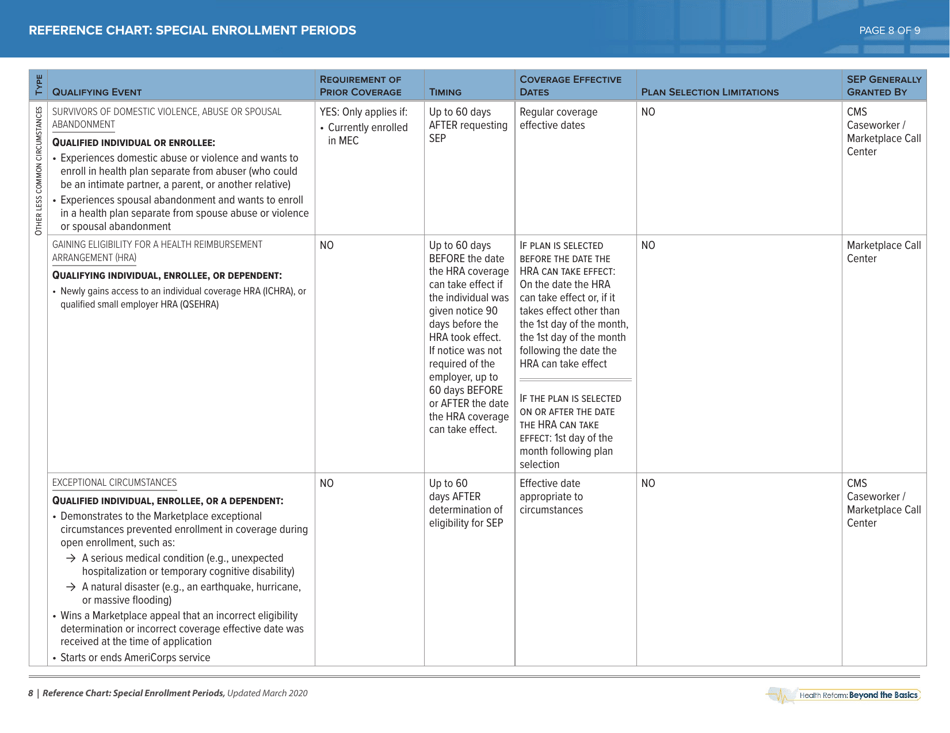
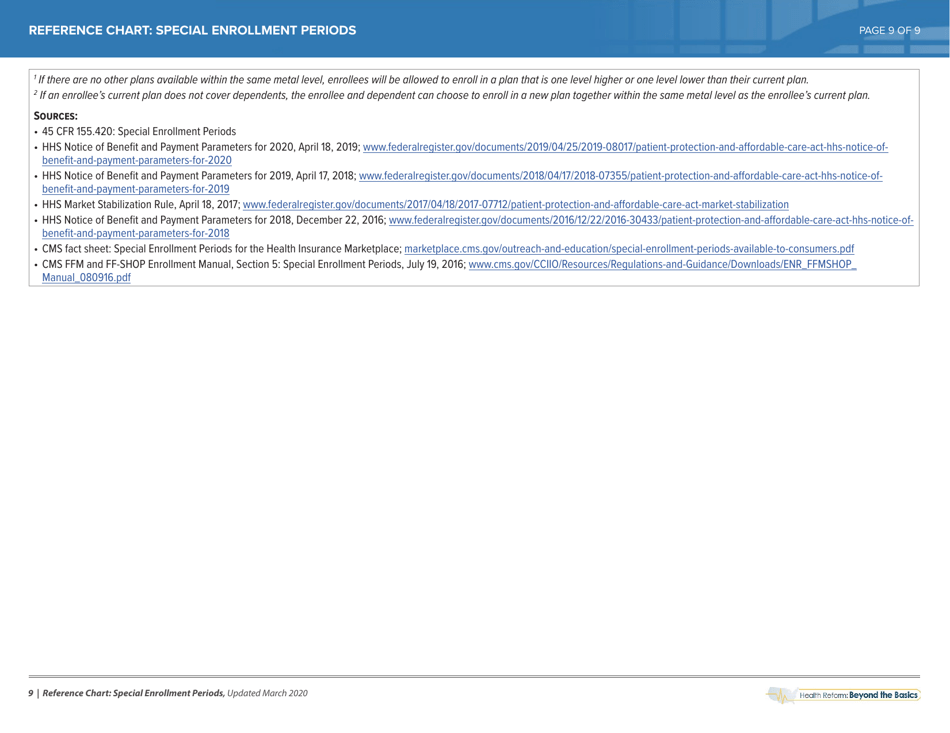
The Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics is a resource that provides information about the circumstances that might qualify individuals for a Special Enrollment Period (SEP) in the health insurance marketplace. SEPs allow people to enroll in or change their health insurance plans outside of the regular open enrollment period.
The Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics is typically filed by the Centers for Medicare and Medicaid Services (CMS).
FAQ
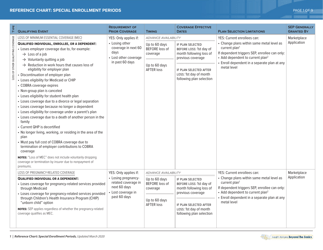
Q: What is the Special Enrollment Period?
A: The Special Enrollment Period is a time outside of the regular Open Enrollment period when individuals can sign up for health insurance.
Q: Who is eligible for the Special Enrollment Period?
A: Various life events such as losing health coverage, getting married, or having a baby can make you eligible for the Special Enrollment Period.
Q: When can I enroll in health insurance during the Special Enrollment Period?
A: You typically have 60 days from the qualifying life event to enroll in health insurance during the Special Enrollment Period.
Q: How do I prove my eligibility for the Special Enrollment Period?
A: You may need to provide documentation such as a termination letter from your previous health coverage, marriage certificate, or birth certificate to prove your eligibility for the Special Enrollment Period.
Q: Can I apply for the Special Enrollment Period if I don't have a qualifying life event?
A: No, you can only apply for the Special Enrollment Period if you have a qualifying life event. Otherwise, you will have to wait for the next Open Enrollment period to sign up for health insurance.