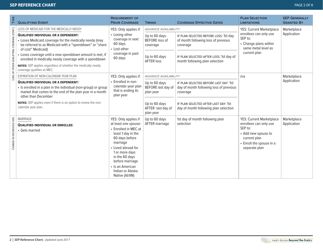
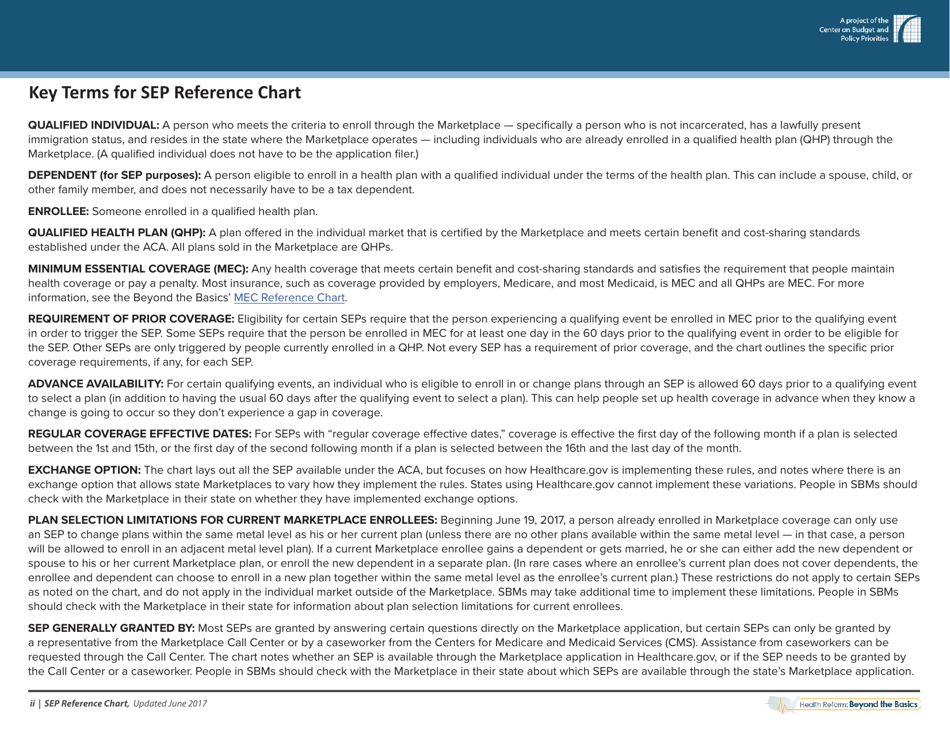
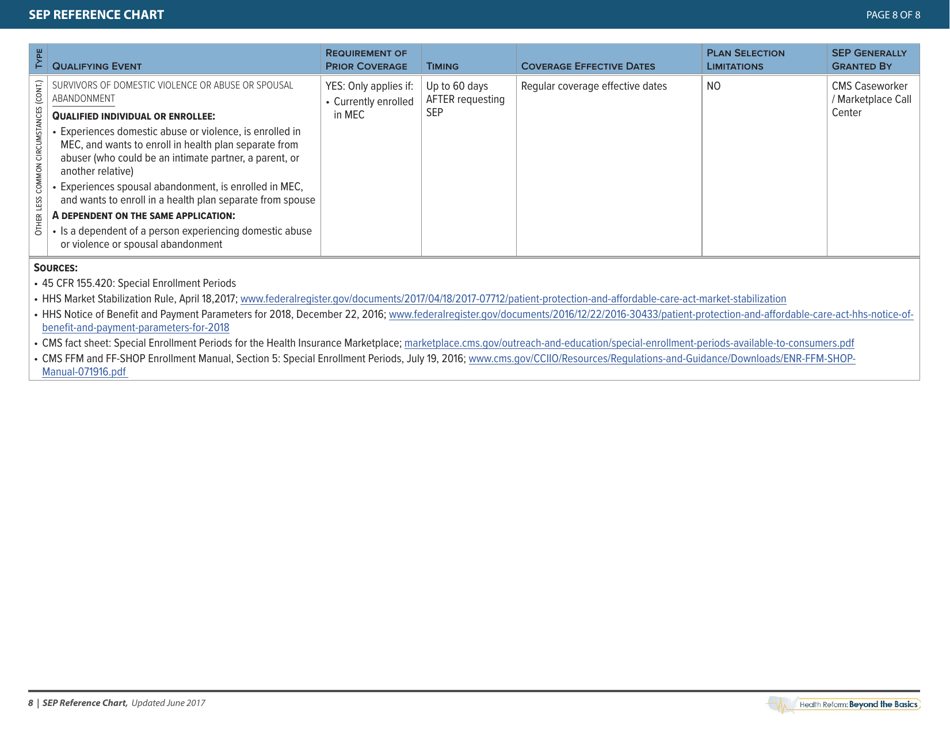
Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics
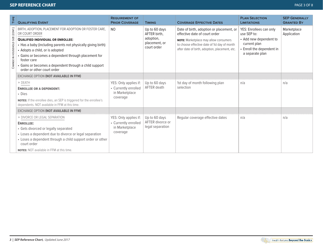
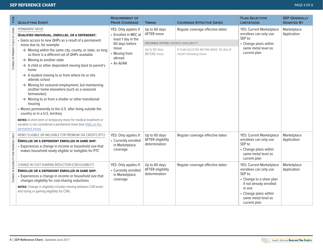
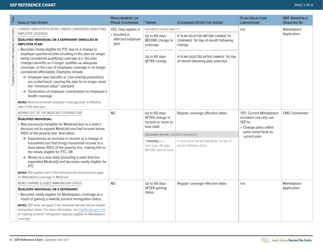
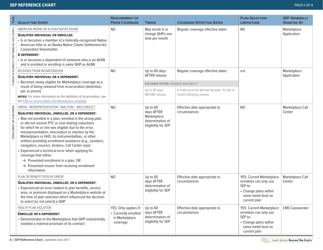
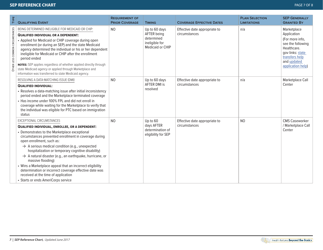
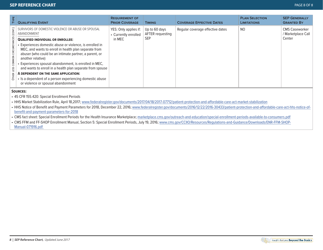
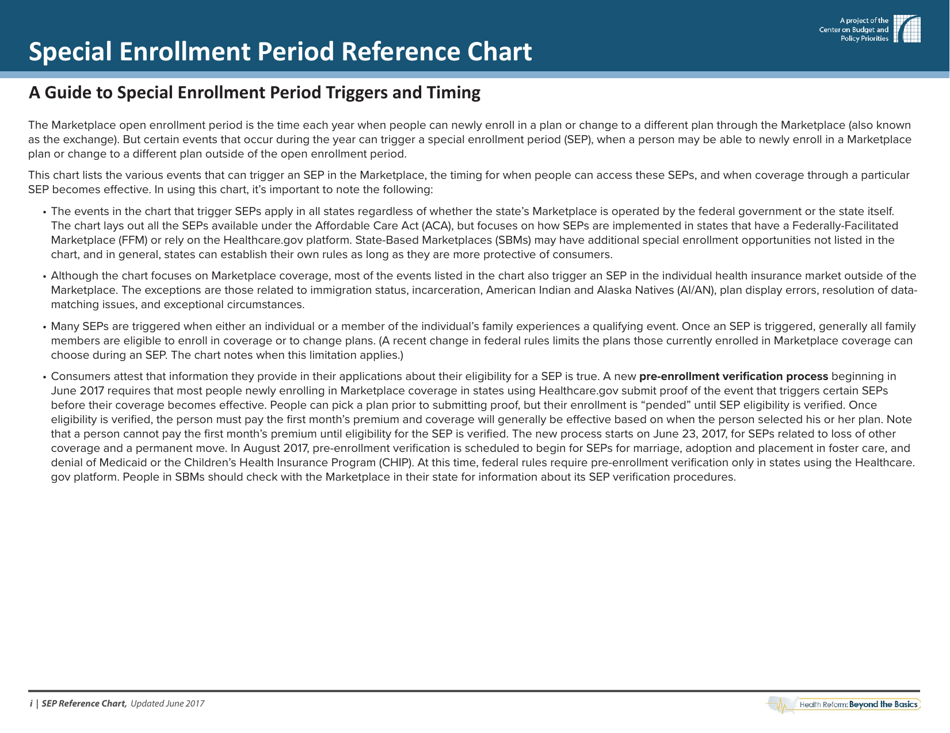
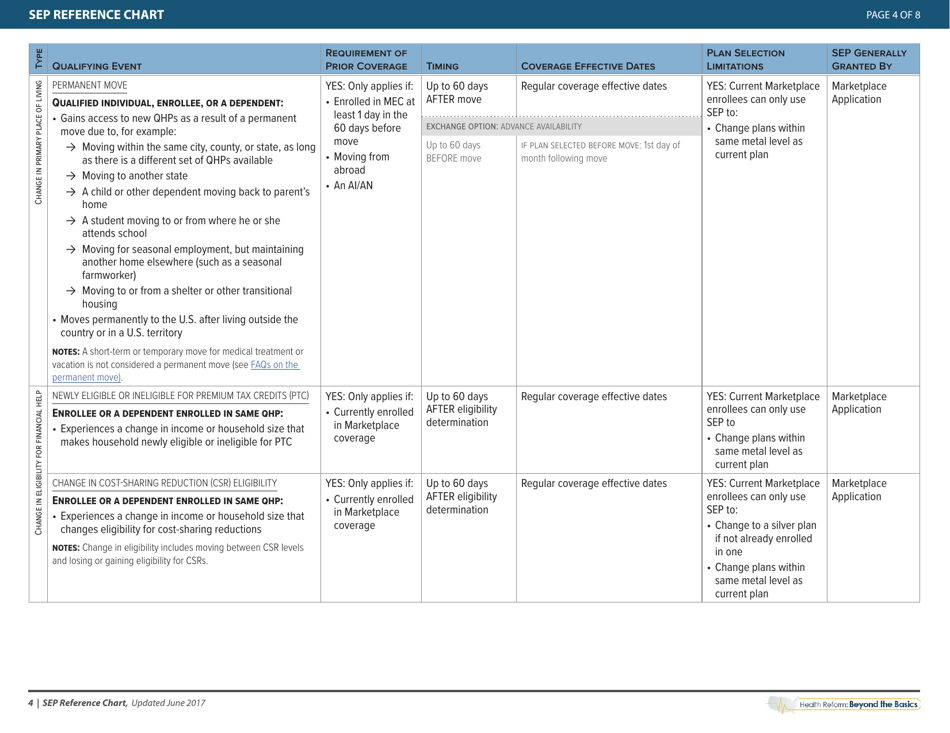
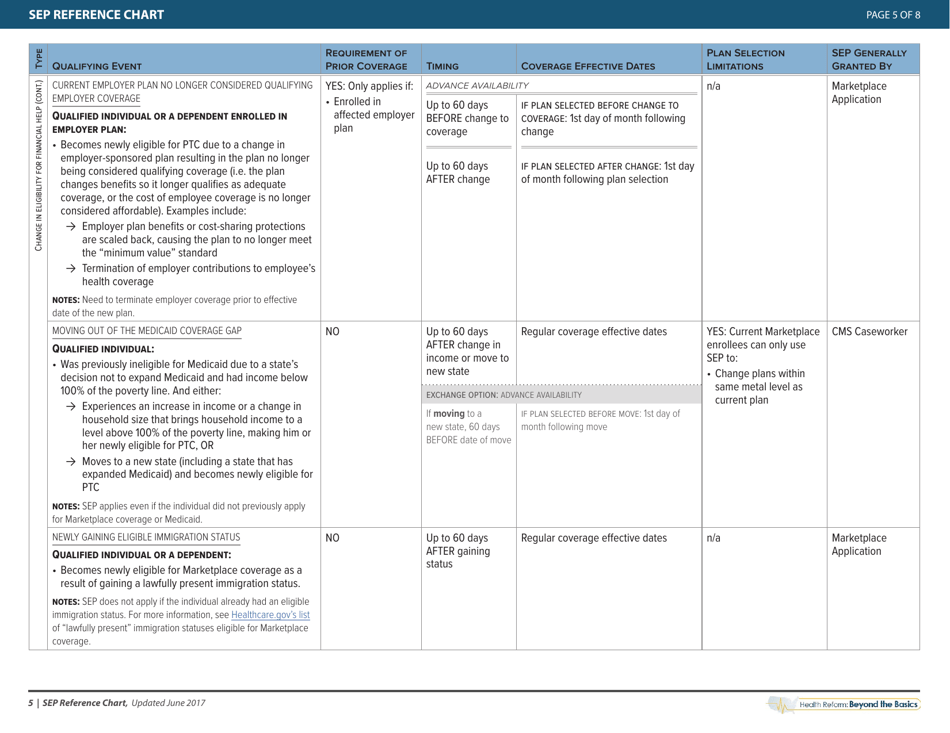
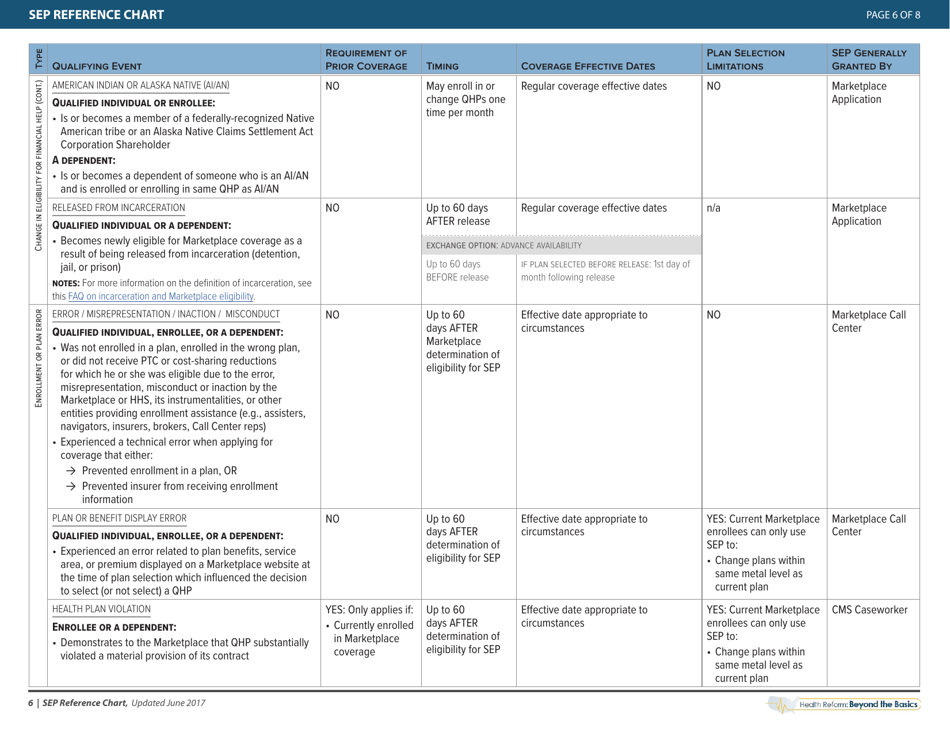
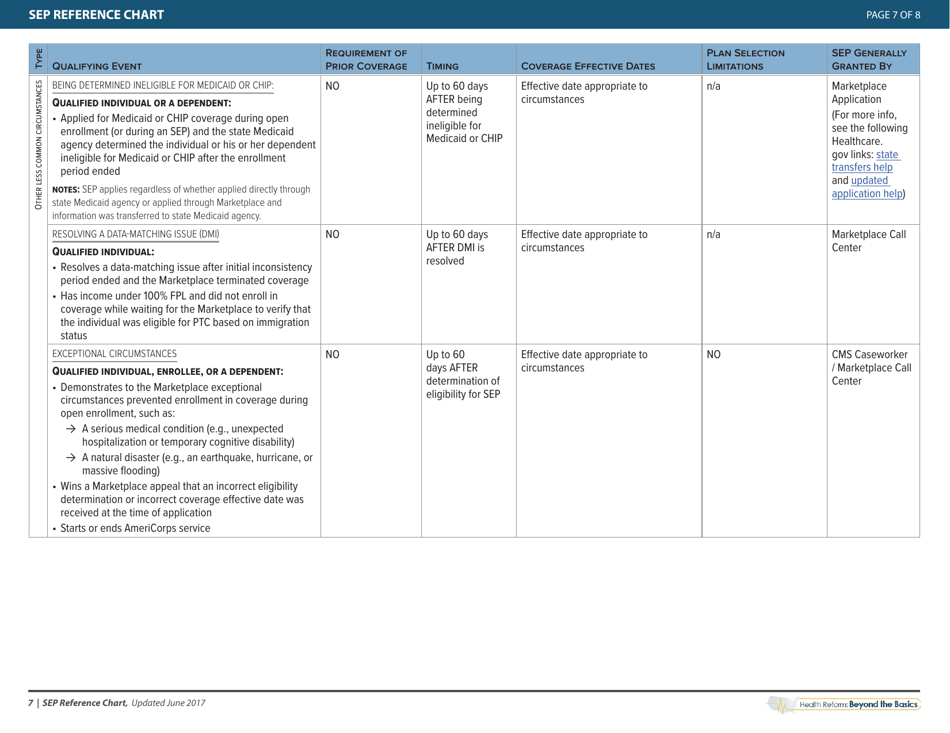
The Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics is a resource that provides information on when individuals are eligible to enroll in or make changes to their health insurance coverage outside of the regular enrollment periods. It outlines the specific life events or circumstances that may qualify an individual for a Special Enrollment Period.
The Centers for Medicare & Medicaid Services (CMS) files the Special Enrollment Period Reference Chart - Health Reform: Beyond the Basics.
FAQ
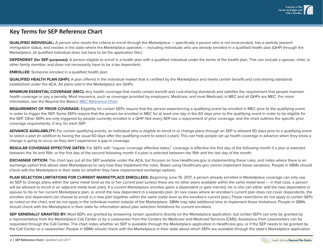
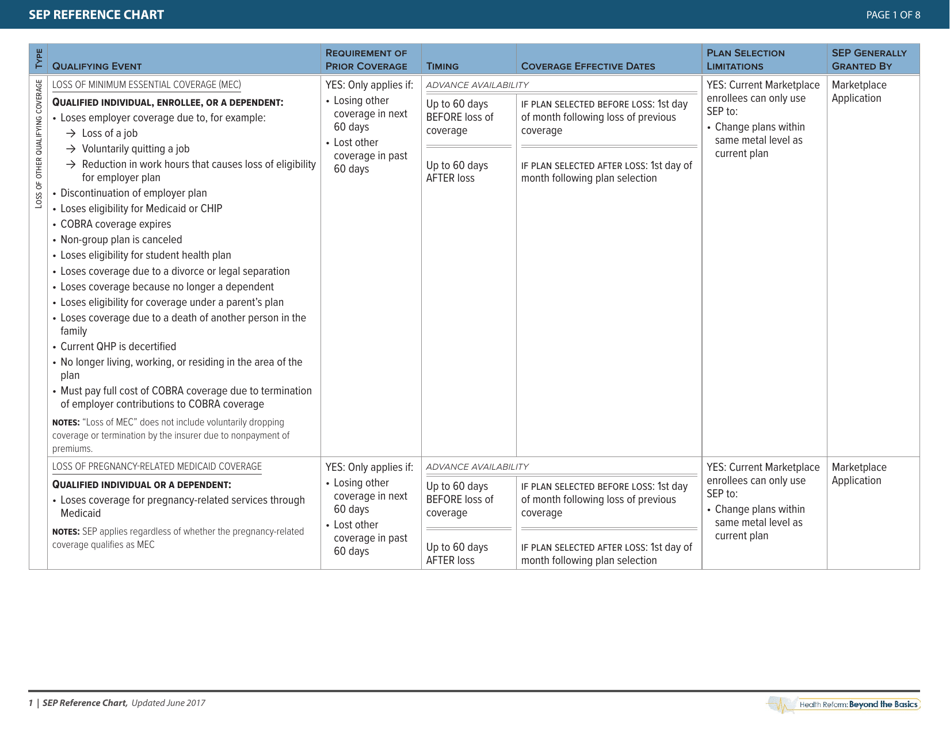
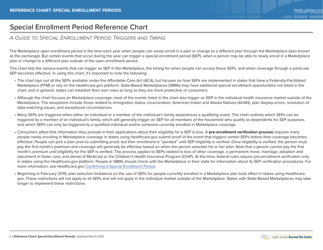
Q: What is a Special Enrollment Period (SEP)?
A: A Special Enrollment Period (SEP) is a time outside of the yearly Open Enrollment Period when you can sign up for health insurance.
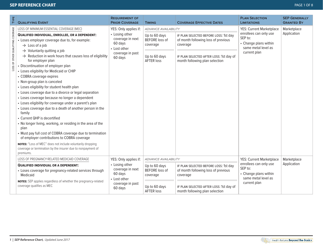
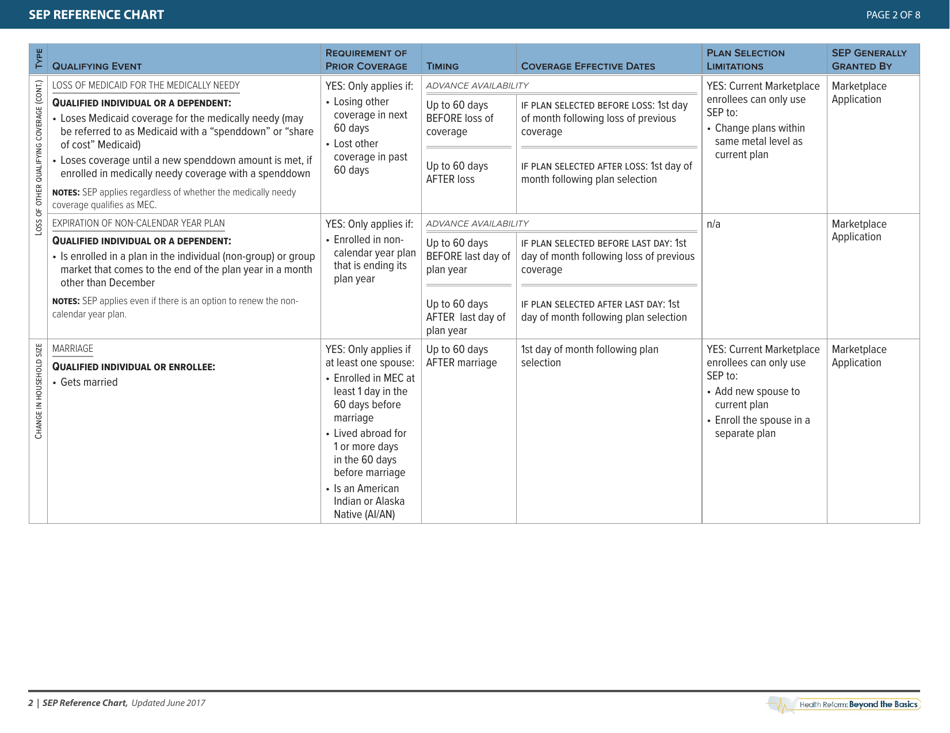
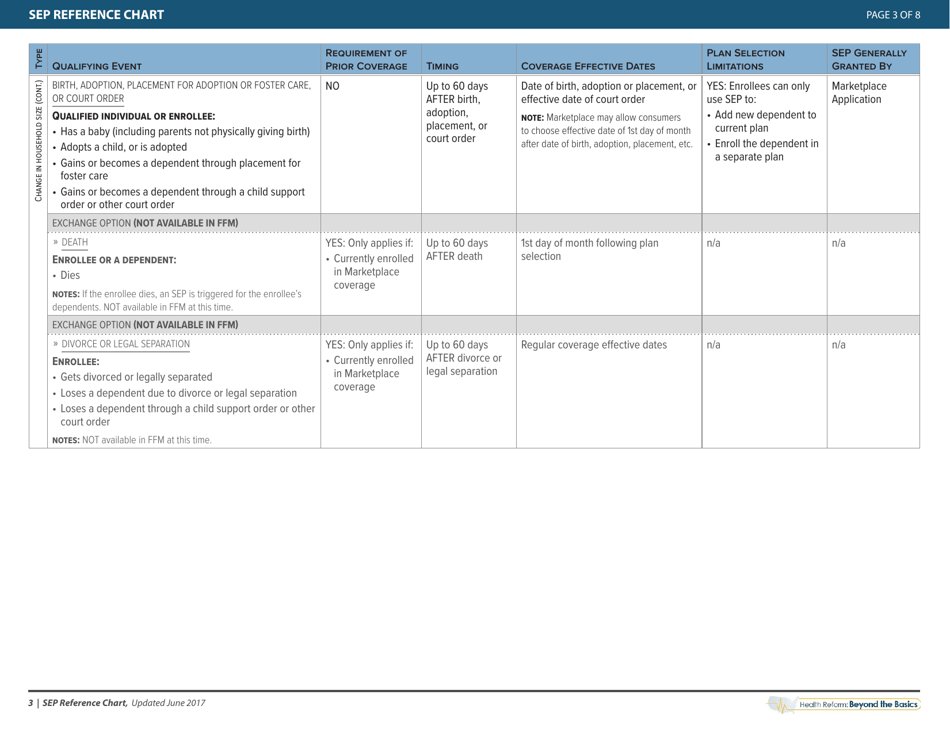
Q: When can I qualify for a Special Enrollment Period?
A: You can qualify for a Special Enrollment Period if you experience certain life events, such as getting married, having a baby, or losing other health coverage.
Q: How long do I have to enroll during a Special Enrollment Period?
A: Generally, you have 60 days from the date of the qualifying life event to enroll in a health insurance plan.
Q: Is there a penalty for not enrolling during the Open Enrollment Period?
A: Yes, if you do not have health insurance during the Open Enrollment Period and do not qualify for a Special Enrollment Period, you may have to pay a penalty when you file your taxes.
Q: Can I apply for Medicaid or the Children's Health Insurance Program (CHIP) at any time?
A: Generally, you can apply for Medicaid or CHIP at any time, as these programs have year-round enrollment.