Form ICN006973 Medicare Claim Review Programs
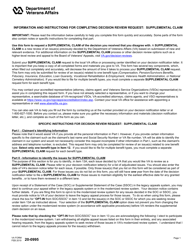
What Is Form ICN006973?
This is a legal form that was released by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services on September 1, 2016 and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is ICN006973?
A: ICN006973 is the document that provides information about Medicare Claim Review Programs.
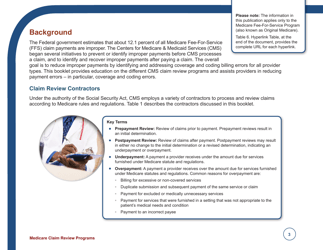
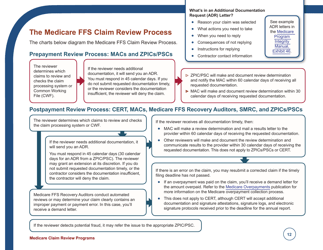
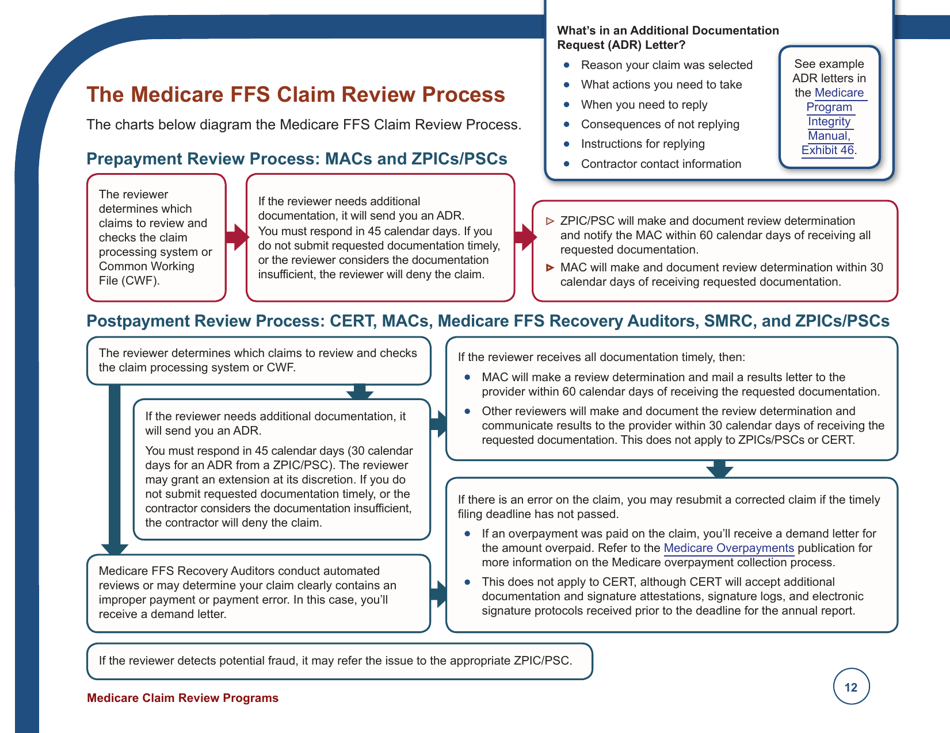
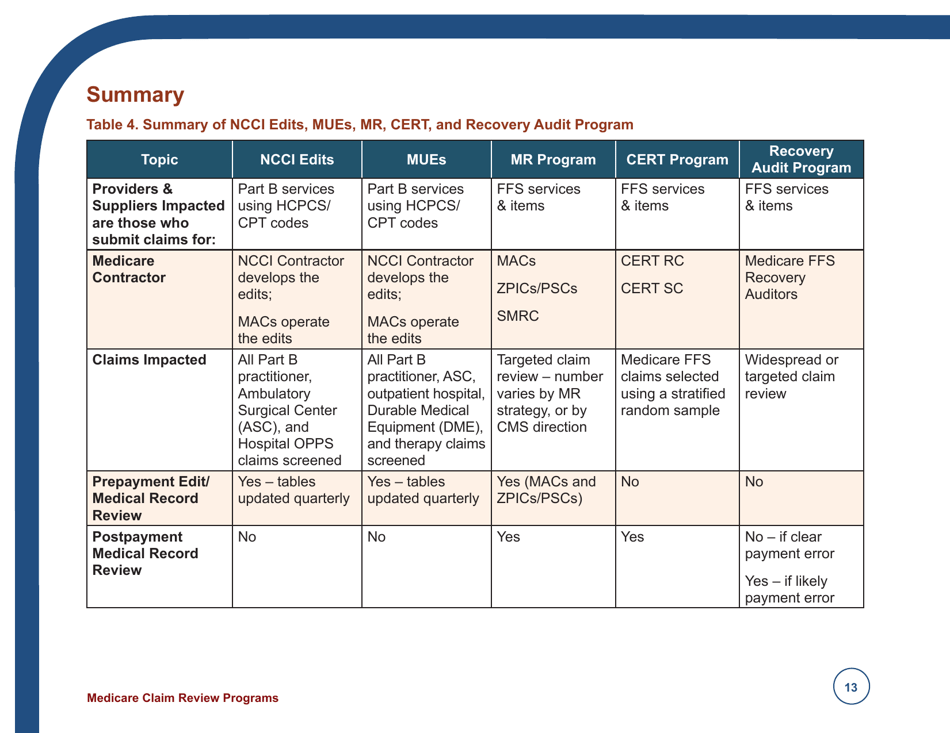
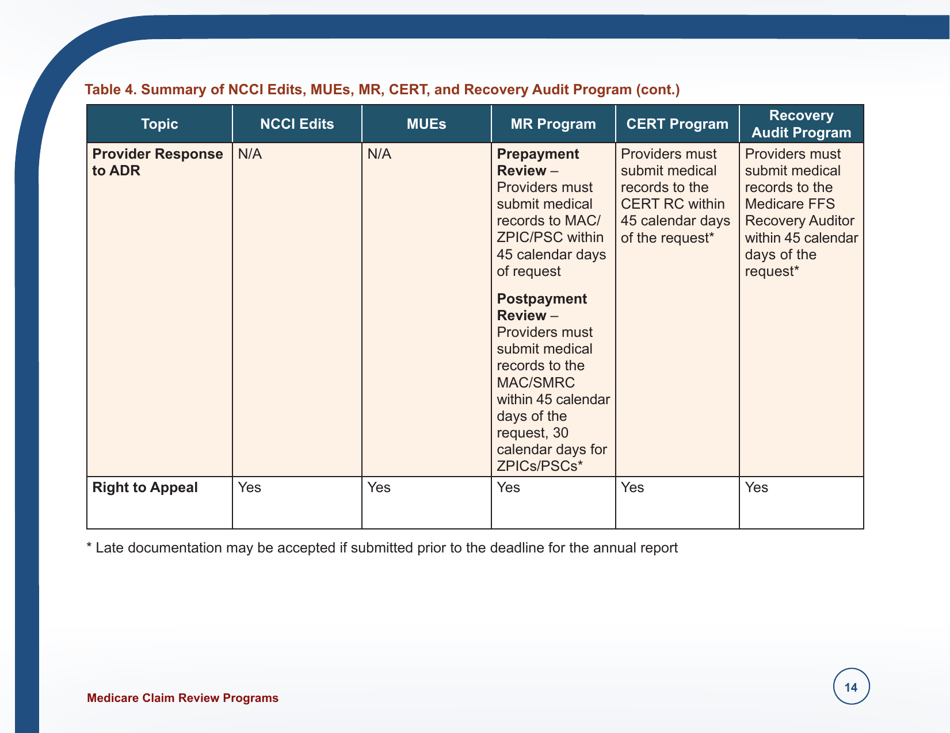
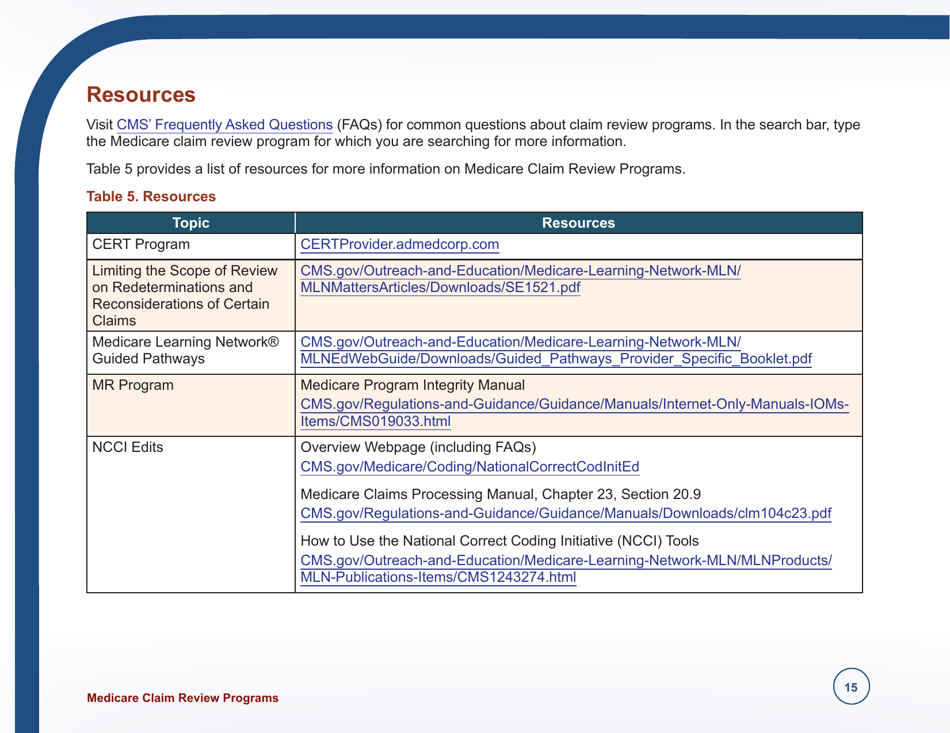
Q: What are Medicare Claim Review Programs?
A: Medicare Claim Review Programs are programs that help ensure the accuracy and appropriateness of Medicare claims.
Q: Why are Medicare Claim Review Programs important?
A: Medicare Claim Review Programs are important as they help prevent fraud, waste, and abuse in the Medicare system.
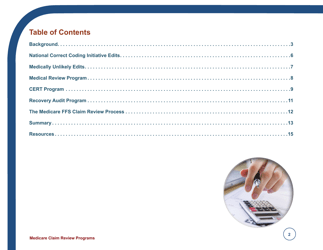
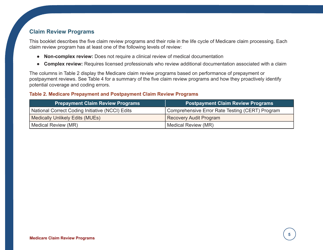
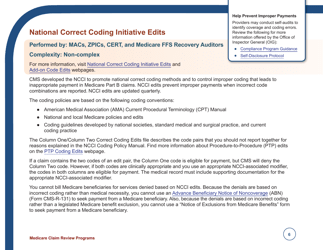
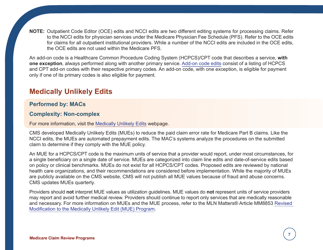
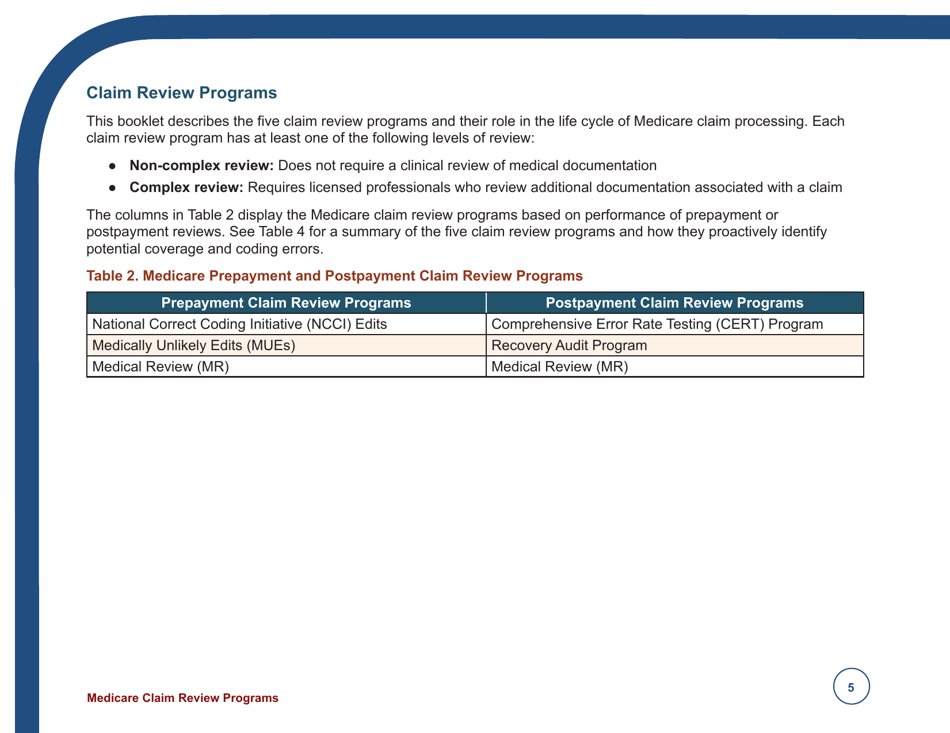
Q: What are some examples of Medicare Claim Review Programs?
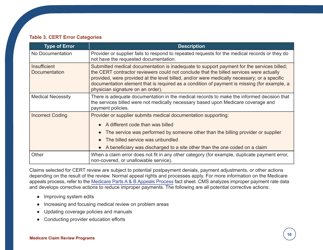
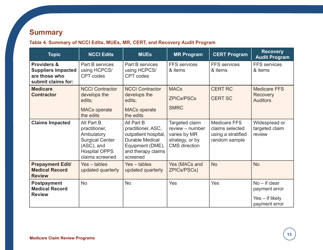
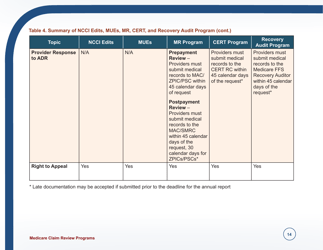
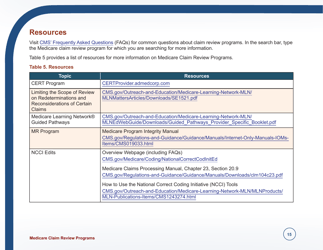
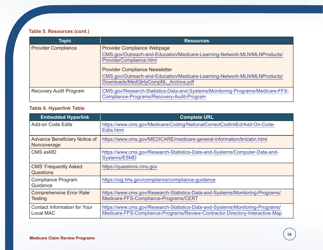
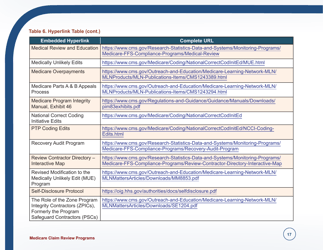
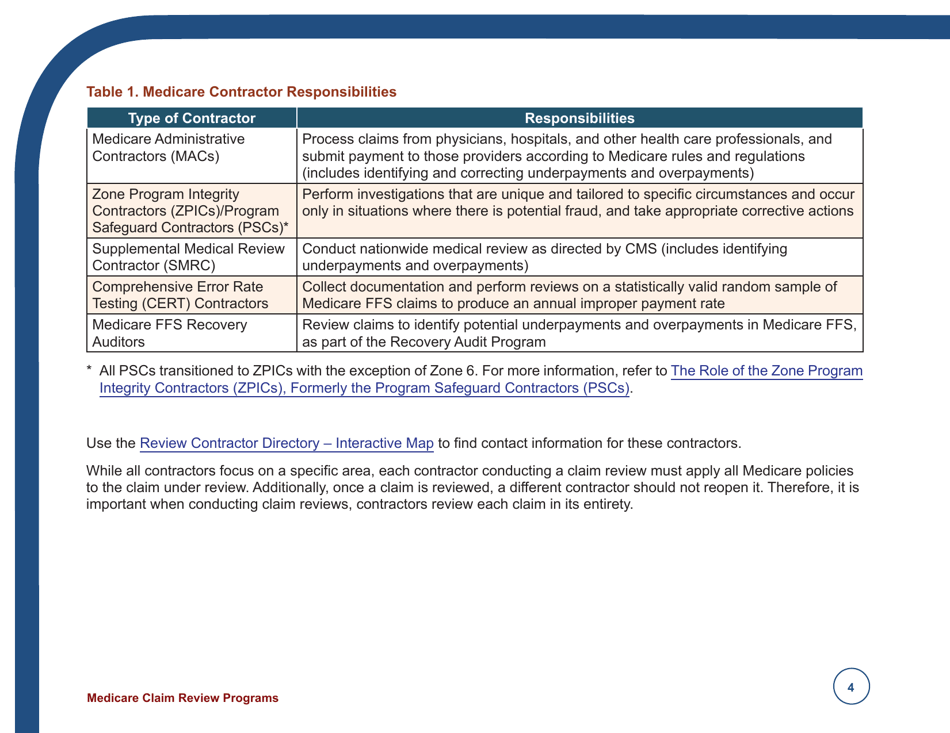
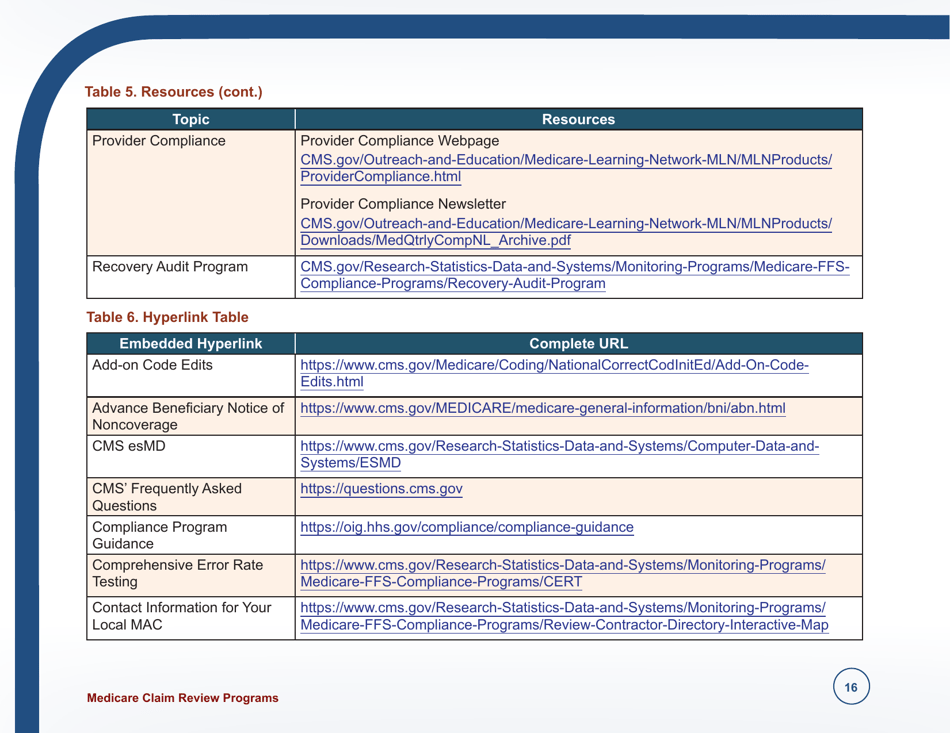
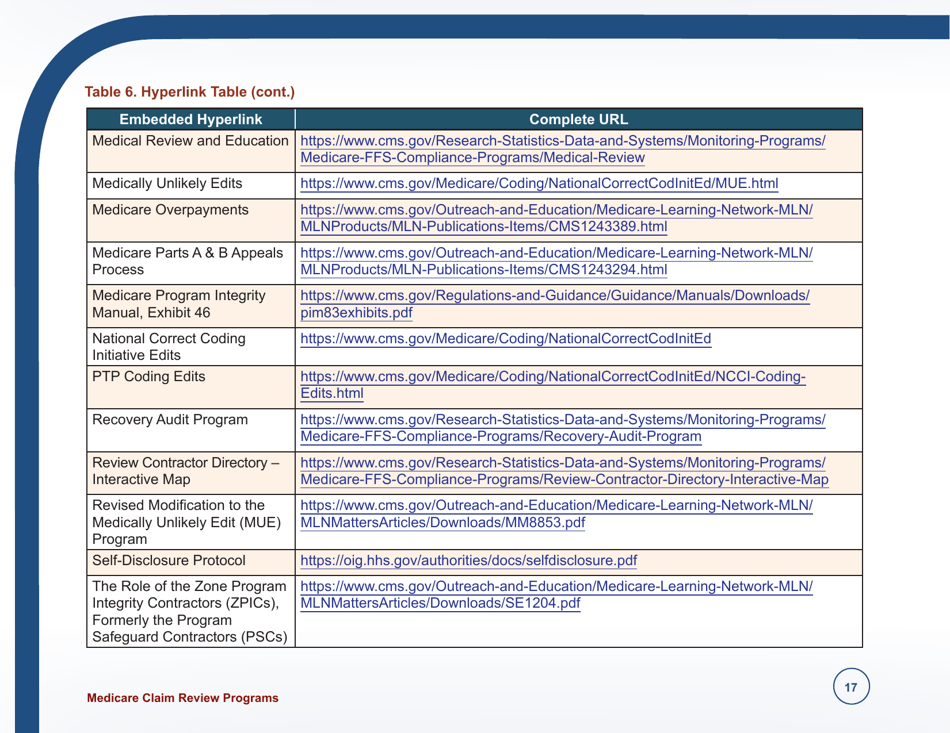
A: Some examples of Medicare Claim Review Programs include the Recovery Audit Program, the Medicare Administrative Contractor (MAC) Program, and the Comprehensive Error Rate Testing (CERT) Program.
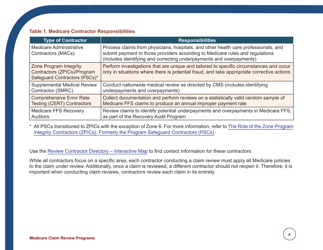
Q: Who is responsible for administering Medicare Claim Review Programs?
A: Medicare Claim Review Programs are administered by various entities, including the Centers for Medicare & Medicaid Services (CMS) and Medicare Administrative Contractors (MACs).
Form Details:
- Released on September 1, 2016;
- The latest available edition released by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of Form ICN006973 by clicking the link below or browse more documents and templates provided by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services.