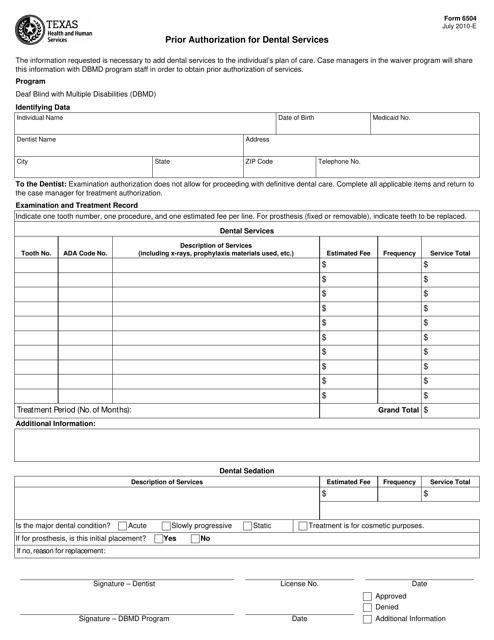
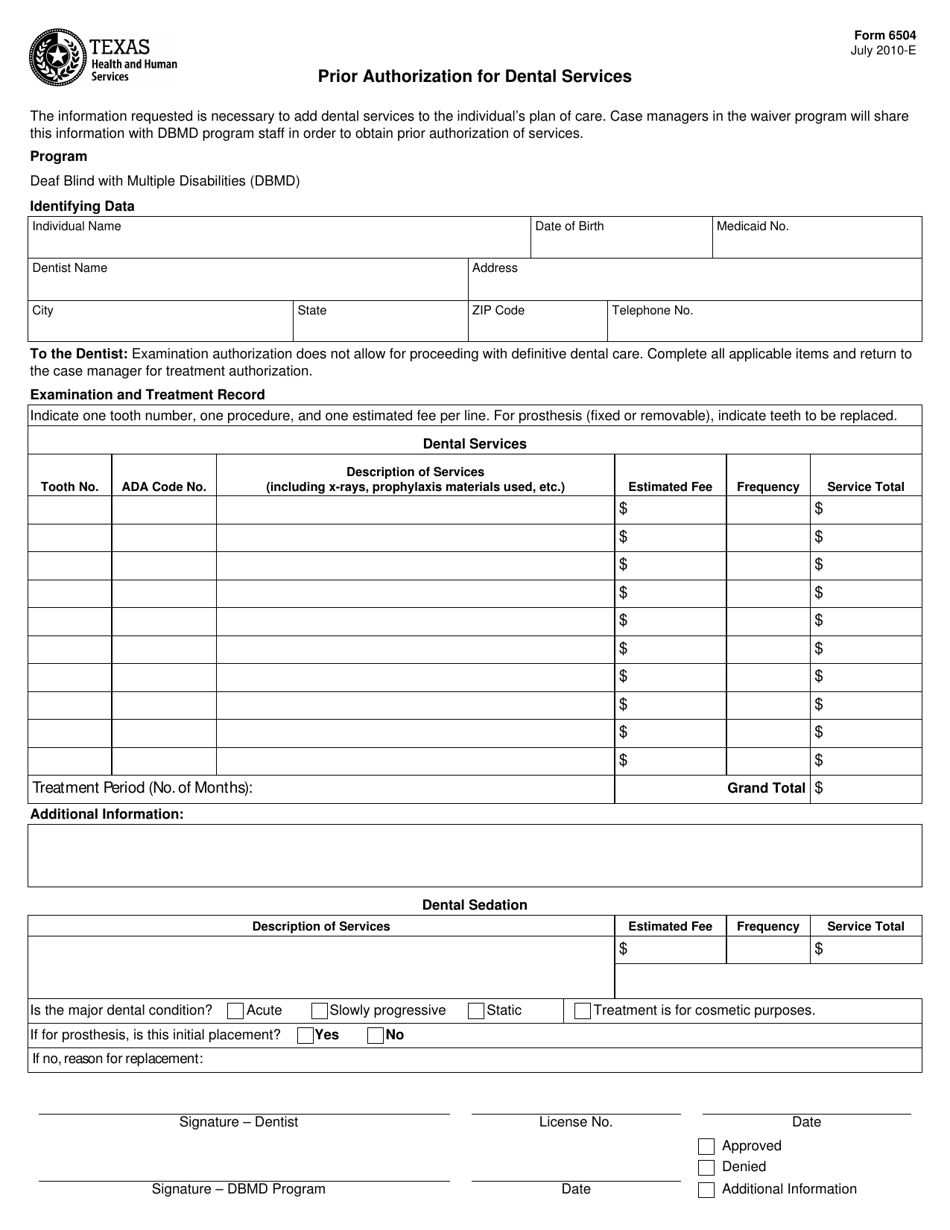
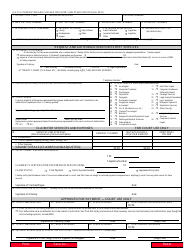
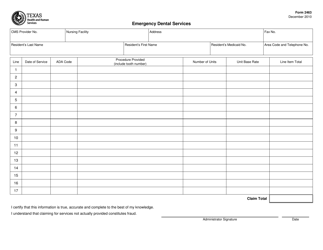
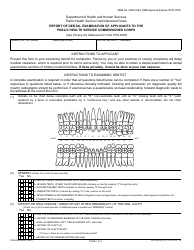
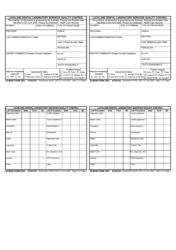
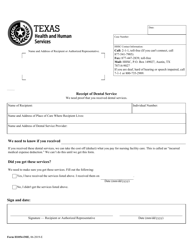
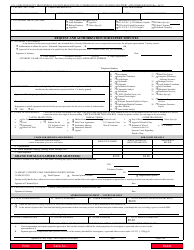
Form 6504 Prior Authorization for Dental Services - Texas
What Is Form 6504?
This is a legal form that was released by the Texas Health and Human Services - a government authority operating within Texas. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form 6504?
A: Form 6504 is a Prior Authorization for Dental Services form used in Texas.
Q: Why is a prior authorization required for dental services?
A: Prior authorization is required to ensure that dental services meet specific criteria and are medically necessary.
Q: Who needs to complete Form 6504?
A: Dentists or dental providers in Texas need to complete Form 6504.
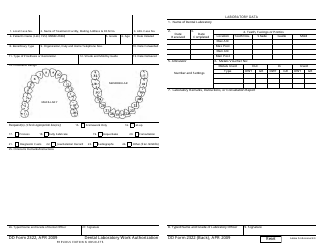
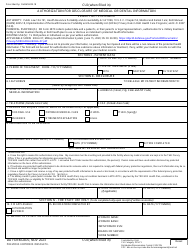
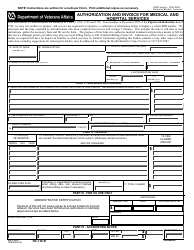
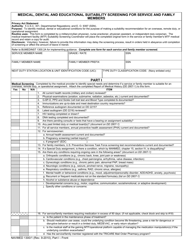
Q: What information is required on Form 6504?
A: Form 6504 requires information about the patient, the requested dental services, and supporting documentation.
Q: How long does it take to process a prior authorization?
A: The processing time for a prior authorization can vary, but it is typically within 14 calendar days.
Q: What happens after Form 6504 is submitted?
A: After Form 6504 is submitted, it will be reviewed by the dental benefits administrator to determine if prior authorization is granted.
Q: Can Form 6504 be submitted electronically?
A: Yes, Form 6504 can be submitted electronically through the TMHP provider portal.
Q: What should I do if my prior authorization request is denied?
A: If your prior authorization request is denied, you have the right to appeal the decision and provide additional supporting documentation.
Q: Is prior authorization required for all dental services?
A: No, not all dental services require prior authorization. Only certain procedures or treatments specified by the dental benefits administrator may require prior authorization.
Form Details:
- Released on July 1, 2010;
- The latest edition provided by the Texas Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form 6504 by clicking the link below or browse more documents and templates provided by the Texas Health and Human Services.