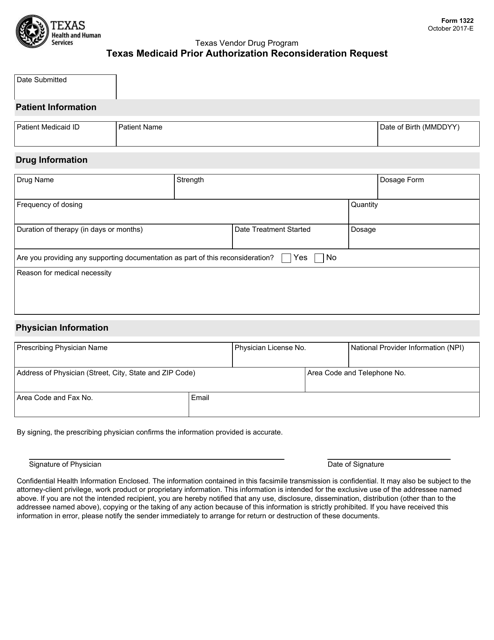
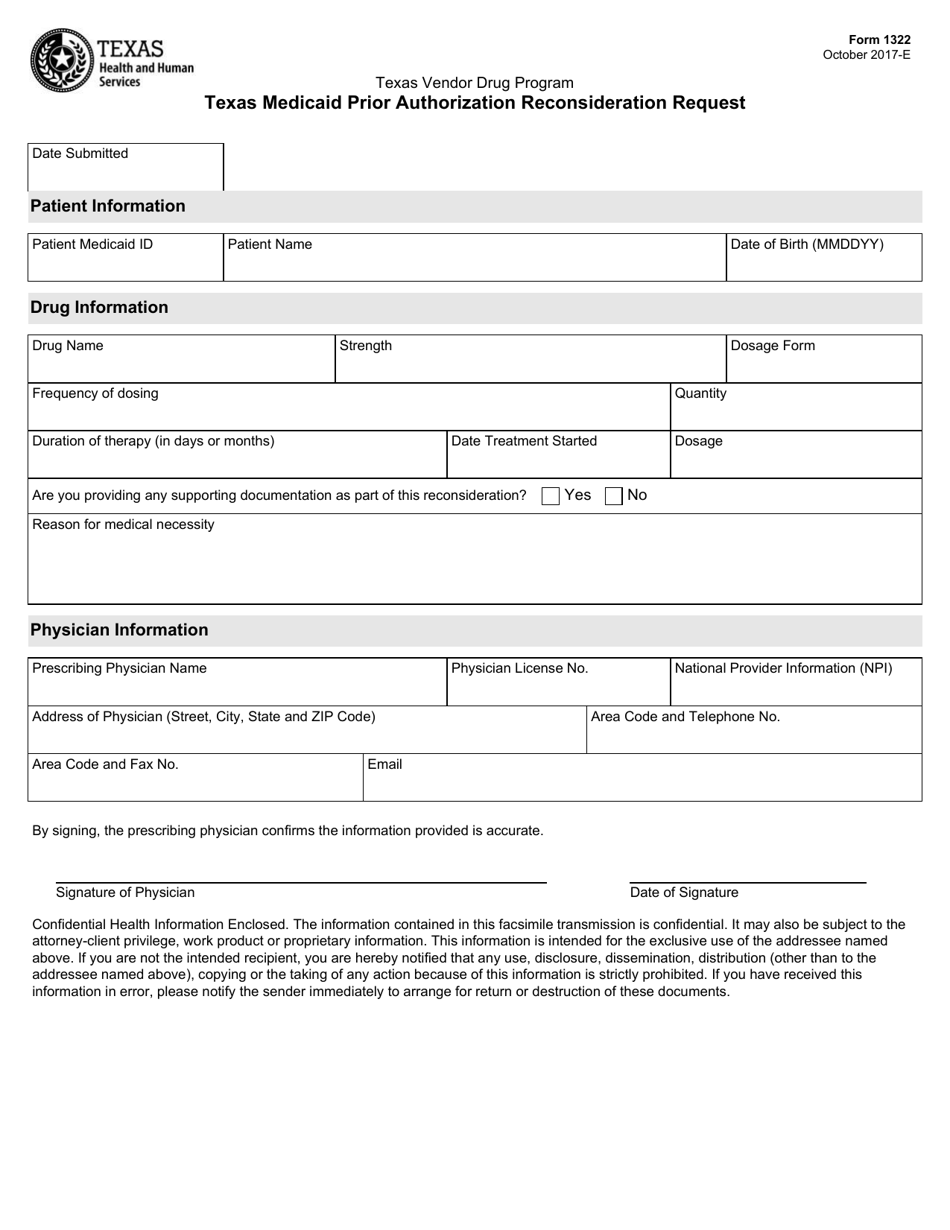
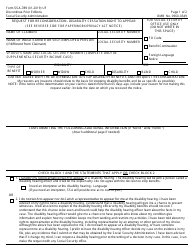
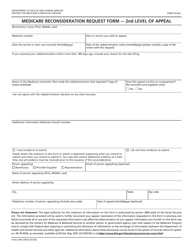
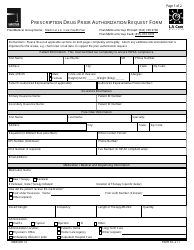
Form 1322 Texas Medicaid Prior Authorization Reconsideration Request - Texas
What Is Form 1322?
This is a legal form that was released by the Texas Health and Human Services - a government authority operating within Texas. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form 1322?
A: Form 1322 is the Texas Medicaid Prior Authorization Reconsideration Request form.
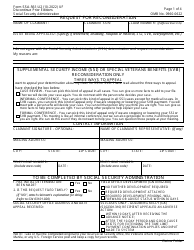
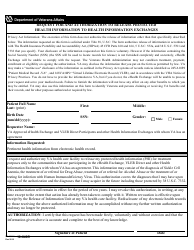
Q: What is the purpose of Form 1322?
A: The purpose of Form 1322 is to request a reconsideration for prior authorization denials for Medicaid services in Texas.
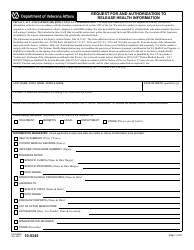
Q: Who can use Form 1322?
A: Form 1322 can be used by providers and practitioners who need to appeal a prior authorization denial for Medicaid services in Texas.
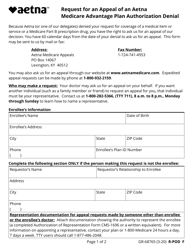
Q: How do I submit Form 1322?
A: Form 1322 should be submitted to the appropriate Texas Medicaid & Healthcare Partnership (TMHP) address as specified on the form.
Q: What information is required on Form 1322?
A: Form 1322 requires the provider's information, recipient's information, details of the denied service, reasons for the reconsideration, and any supporting documentation.
Q: Is there a deadline for submitting Form 1322?
A: Yes, Form 1322 must be submitted within 120 calendar days from the date of the denial notice.
Q: Can I submit additional documentation with Form 1322?
A: Yes, additional documentation that supports the request for reconsideration can be included with Form 1322.
Q: How long does it take to receive a decision on a reconsideration request?
A: The TMHP will make a determination on the reconsideration request within 45 calendar days of receiving all necessary information.
Q: What should I do if my reconsideration request is denied?
A: If the reconsideration request is denied, the provider can pursue further appeals through the TMHP's appeals process.
Form Details:
- Released on October 1, 2017;
- The latest edition provided by the Texas Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form 1322 by clicking the link below or browse more documents and templates provided by the Texas Health and Human Services.