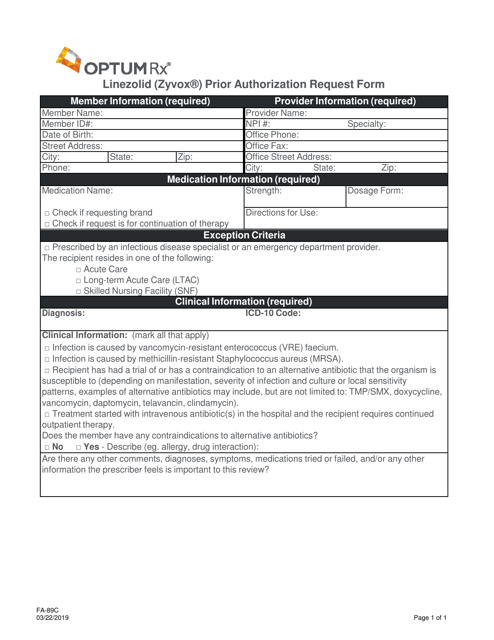
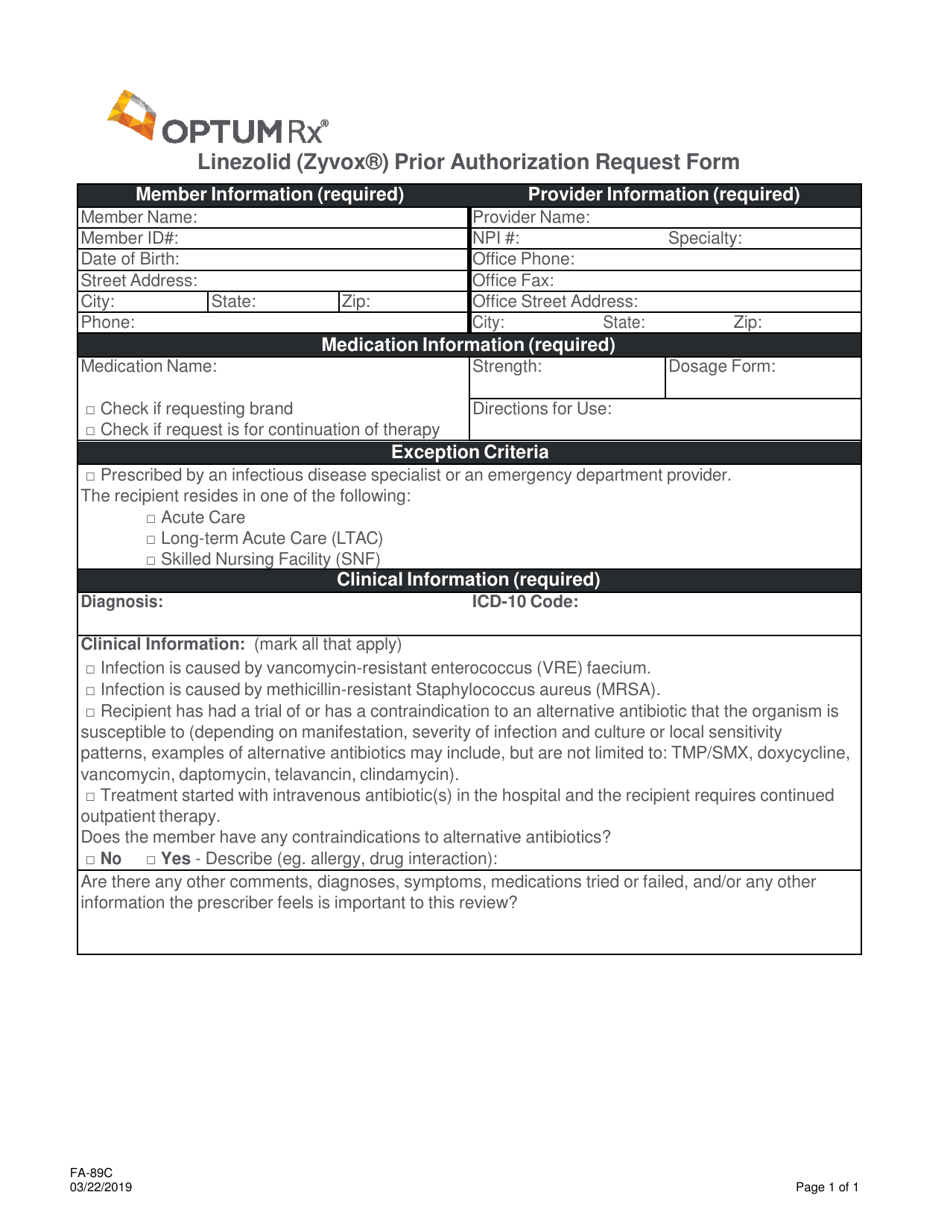
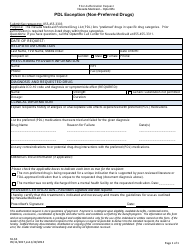
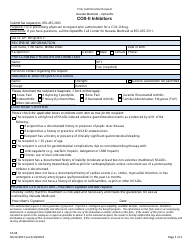
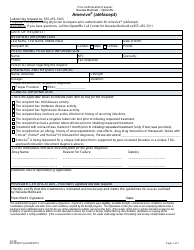
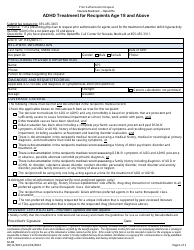
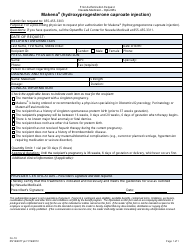
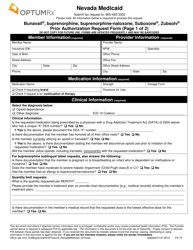
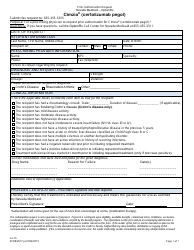
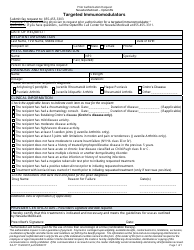
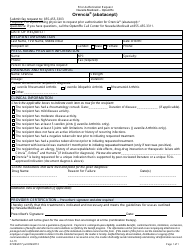
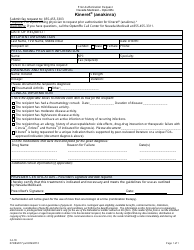
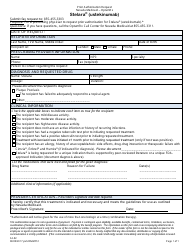
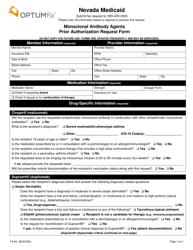
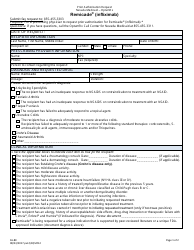
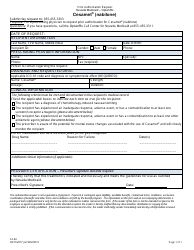
Form FA-89C Linezolid (Zyvox) Prior Authorization Request Form - Nevada
What Is Form FA-89C?
This is a legal form that was released by the Nevada Department of Health and Human Services - a government authority operating within Nevada. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form FA-89C?
A: Form FA-89C is a prior authorization request form for Linezolid (Zyvox).
Q: What is Linezolid (Zyvox)?
A: Linezolid (Zyvox) is a medication used to treat certain bacterial infections.
Q: Why do I need to fill out this form?
A: You need to fill out this form to request prior authorization for Linezolid (Zyvox) in Nevada.
Q: What is prior authorization?
A: Prior authorization is a process where your healthcare provider obtains approval from your insurance company before they will cover the cost of certain medications.
Q: What should I include in the form?
A: You should include your personal information, healthcare provider details, and medical justification for the need of Linezolid (Zyvox) treatment.
Q: How long does the prior authorization process take?
A: The length of the prior authorization process can vary, but it typically takes a few business days to a week.
Q: Can I appeal if my prior authorization request is denied?
A: Yes, you have the right to appeal the decision if your prior authorization request is denied.
Q: Who can help me with the prior authorization process?
A: Your healthcare provider or insurance company can assist you with the prior authorization process.
Form Details:
- Released on March 22, 2019;
- The latest edition provided by the Nevada Department of Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form FA-89C by clicking the link below or browse more documents and templates provided by the Nevada Department of Health and Human Services.