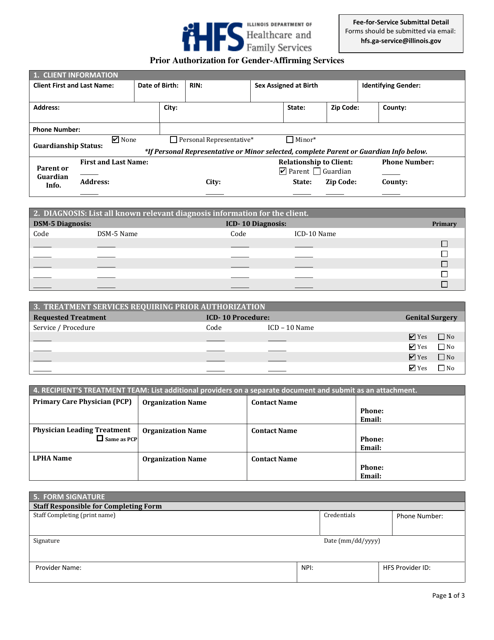
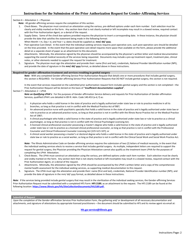
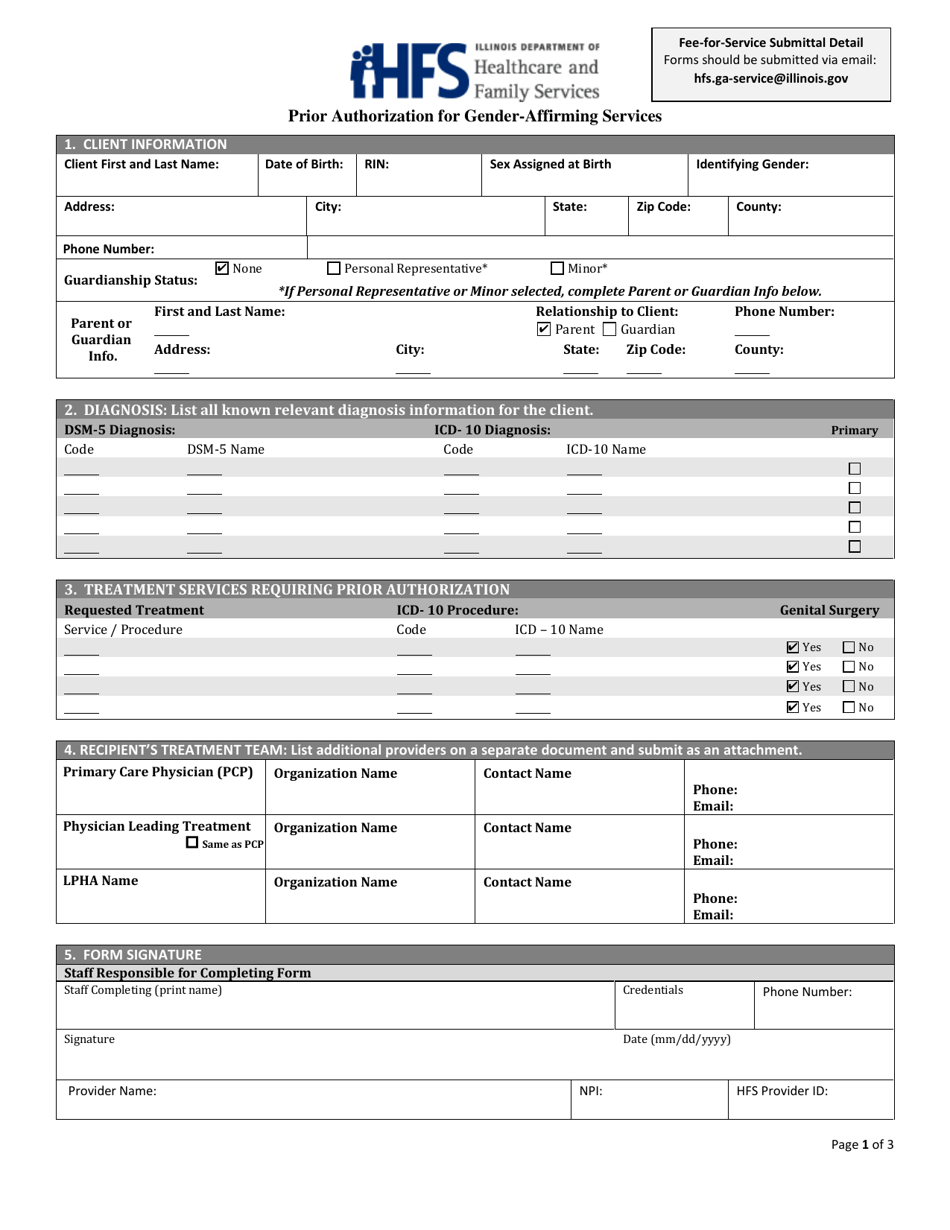
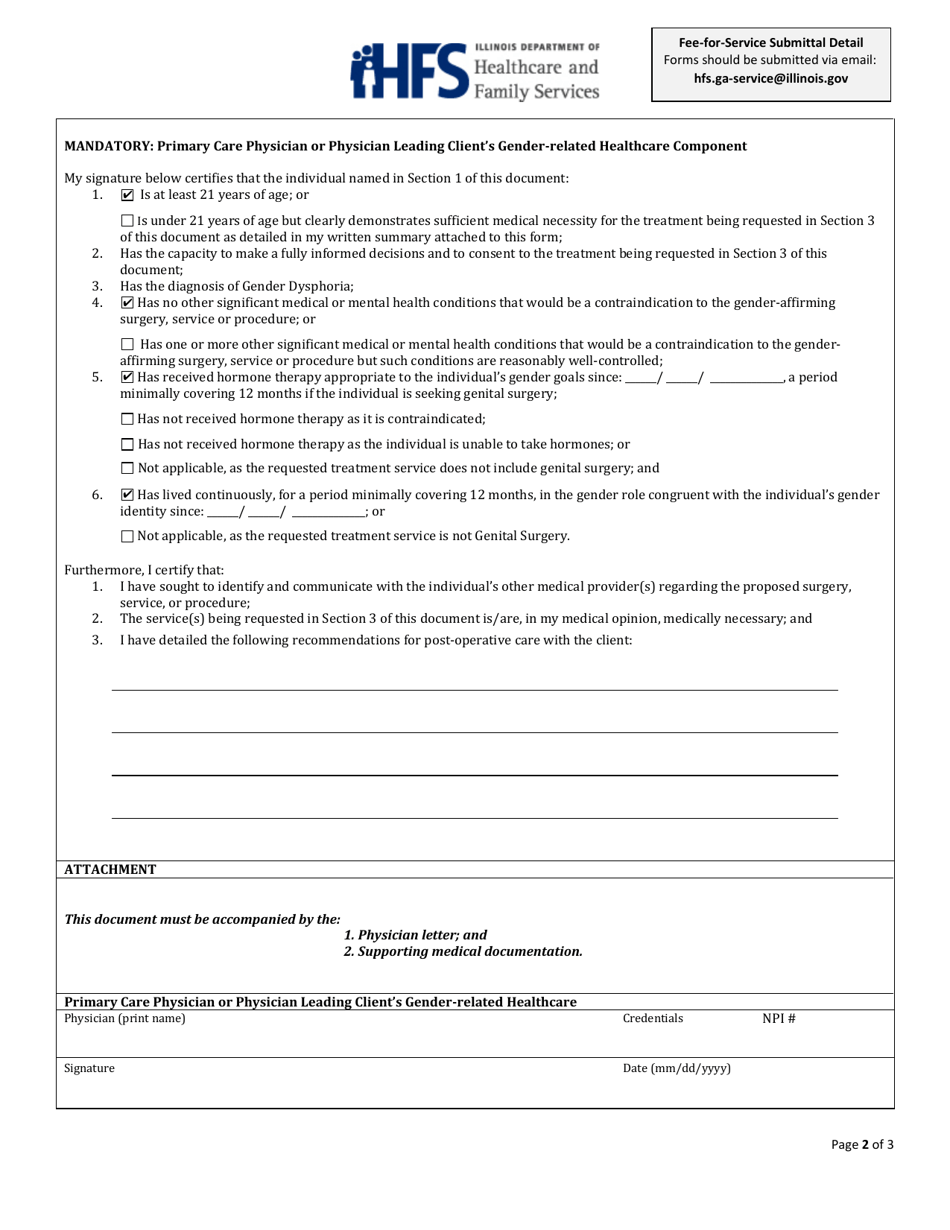
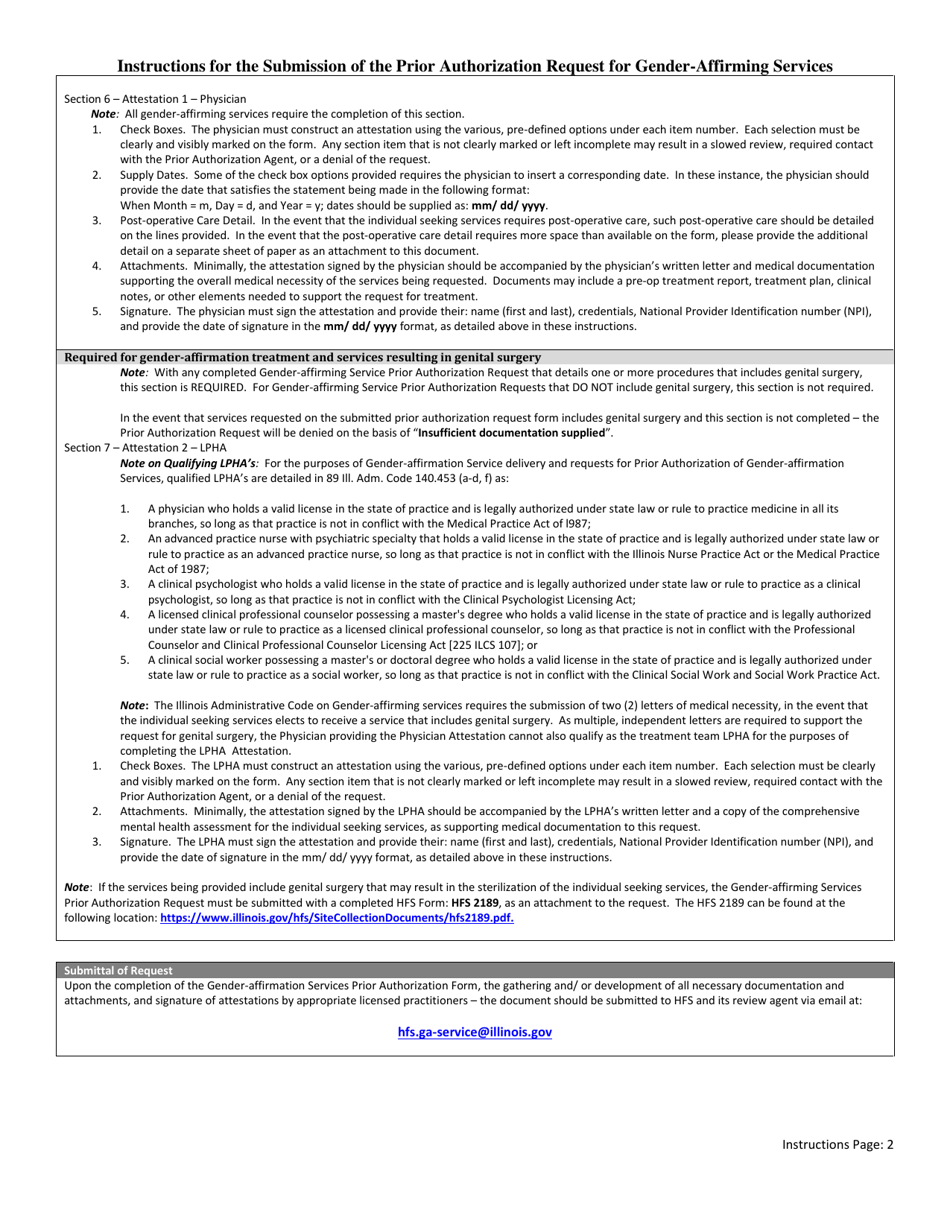
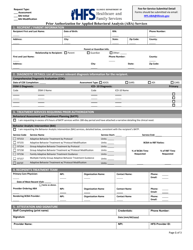
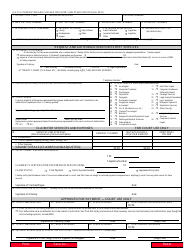
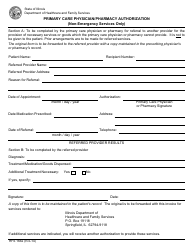
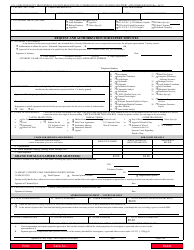
Prior Authorization for Gender-Affirming Services - Illinois
Prior Authorization for Gender-Affirming Services is a legal document that was released by the Illinois Department of Healthcare and Family Services - a government authority operating within Illinois.
FAQ
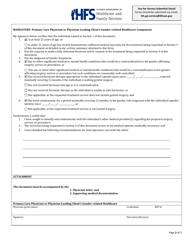
Q: What is prior authorization for gender-affirming services?
A: Prior authorization is a process where healthcare providers need to get approval from insurance companies before providing certain gender-affirming services.
Q: Why is prior authorization required for gender-affirming services?
A: Insurance companies require prior authorization to ensure that the requested services are medically necessary and meet the criteria for coverage.
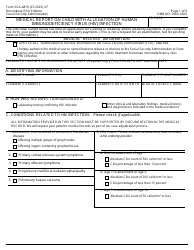
Q: What gender-affirming services may require prior authorization?
A: Gender-affirming surgeries, hormone therapies, and other related healthcare services may require prior authorization.
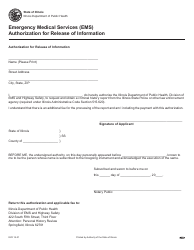
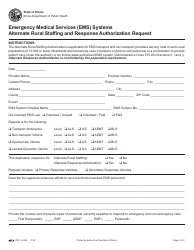
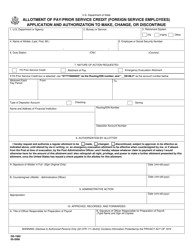
Q: How do healthcare providers obtain prior authorization?
A: Healthcare providers need to submit documentation and information to the insurance company outlining the medical necessity of the requested gender-affirming services.
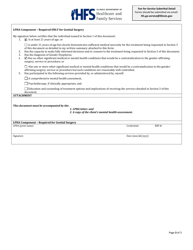
Q: Are all gender-affirming services covered by insurance?
A: Insurance coverage for gender-affirming services may vary. It is important to review your specific insurance plan to understand what services are covered.
Q: What happens if prior authorization is denied?
A: If prior authorization is denied, healthcare providers and patients can go through an appeals process to request reconsideration of the decision.
Q: Are there any laws or regulations specific to Illinois regarding prior authorization for gender-affirming services?
A: Yes, there are laws and regulations in Illinois that aim to protect individuals seeking gender-affirming services, including requirements for insurance coverage and appeals processes.
Form Details:
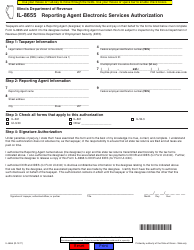
- The latest edition currently provided by the Illinois Department of Healthcare and Family Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Illinois Department of Healthcare and Family Services.