This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
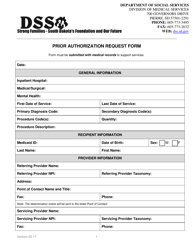
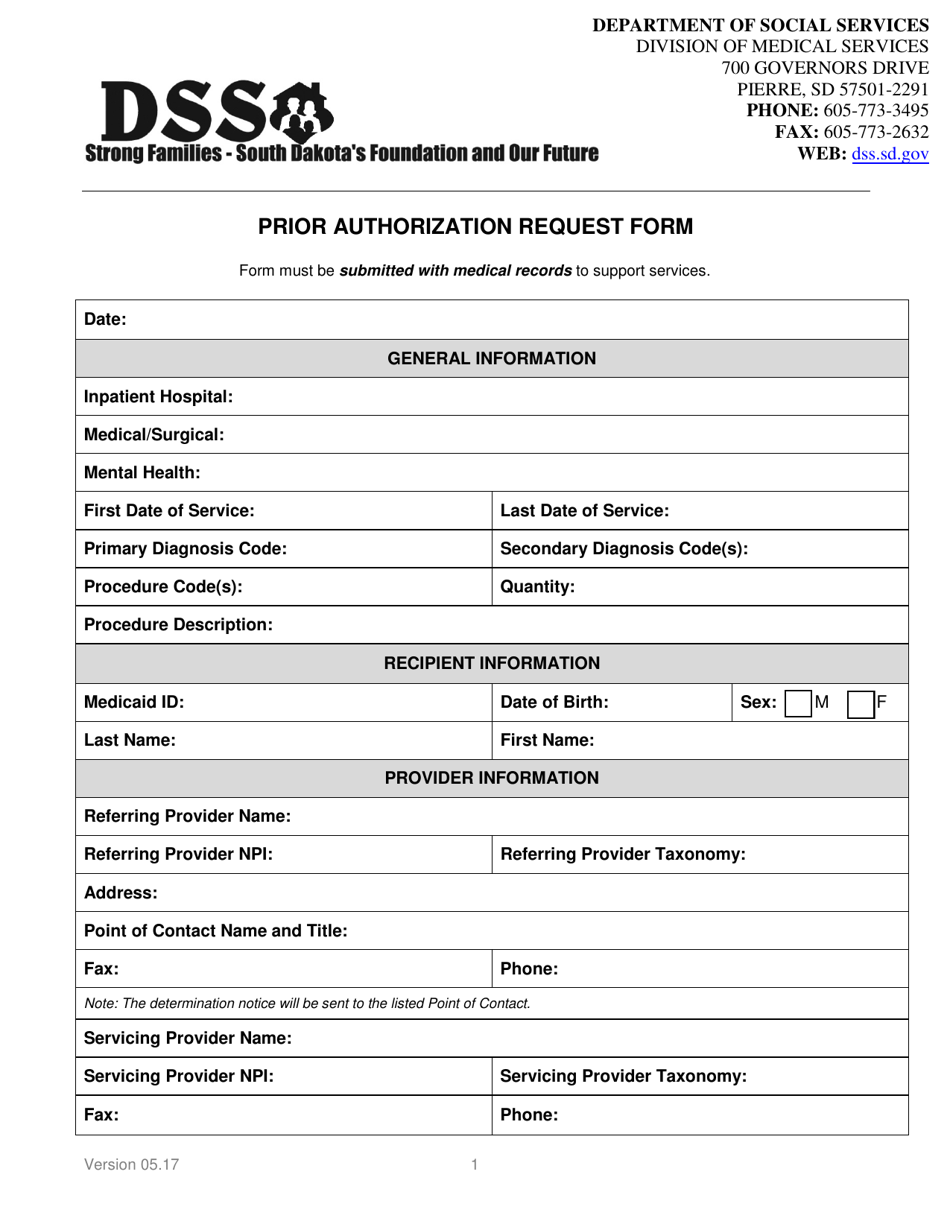
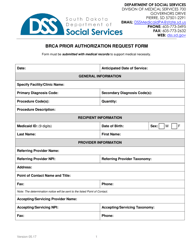
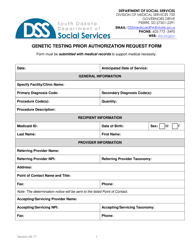
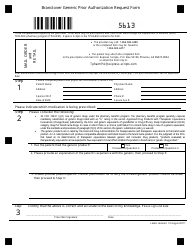
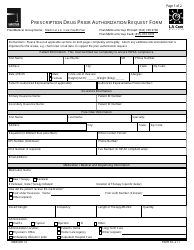
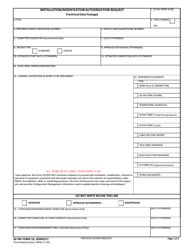
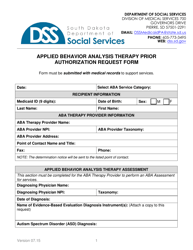
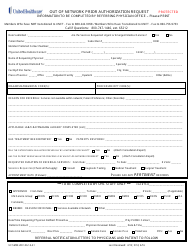
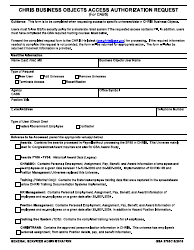
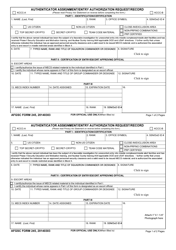
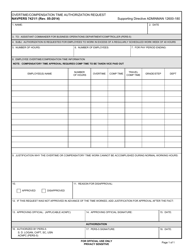
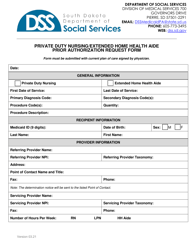
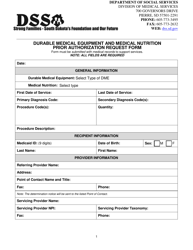
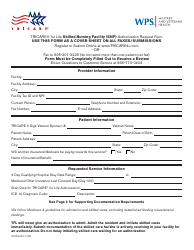
Prior Authorization Request Form - South Dakota
Prior Authorization Request Form is a legal document that was released by the South Dakota Department of Social Services - a government authority operating within South Dakota.
FAQ
Q: What is a Prior Authorization Request Form?
A: A Prior Authorization Request Form is a form used to obtain approval from an insurance company or healthcare provider before receiving certain medical treatments or services.
Q: Why do I need to fill out a Prior Authorization Request Form?
A: You may need to fill out a Prior Authorization Request Form to ensure that the treatment or service you are seeking will be covered by your insurance plan.
Q: What information do I need to provide on a Prior Authorization Request Form?
A: You will typically need to provide your personal information, details about the treatment or service you are requesting, and any supporting documentation that may be required.
Q: How long does it take to get a decision on a Prior Authorization Request?
A: The length of time to get a decision on a Prior Authorization Request can vary. It may take a few days to a few weeks depending on the complexity of the request and the insurance company's review process.
Q: What happens if my Prior Authorization Request is denied?
A: If your Prior Authorization Request is denied, you may have the option to appeal the decision. You should contact your insurance company for more information on the appeals process.
Q: Can I still receive the treatment or service if my Prior Authorization Request is denied?
A: If your Prior Authorization Request is denied, you may still be able to receive the treatment or service, but you may be responsible for the full cost.
Q: Are all medical treatments or services subject to Prior Authorization?
A: Not all medical treatments or services require Prior Authorization. It depends on your insurance plan and the specific treatment or service you are seeking.
Q: Is the Prior Authorization Request Form specific to South Dakota?
A: The Prior Authorization Request Form may vary by state and insurance company. The one specific to South Dakota will be applicable if you are a resident of South Dakota and have insurance coverage in the state.
Q: Who should I contact if I have questions about the Prior Authorization Request Form?
A: If you have questions about the Prior Authorization Request Form, you should contact your healthcare provider or insurance company for assistance.
Form Details:
- Released on May 1, 2017;
- The latest edition currently provided by the South Dakota Department of Social Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the South Dakota Department of Social Services.