This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
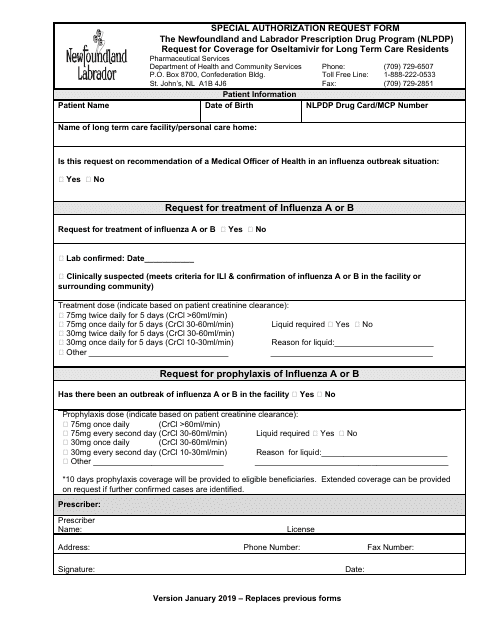
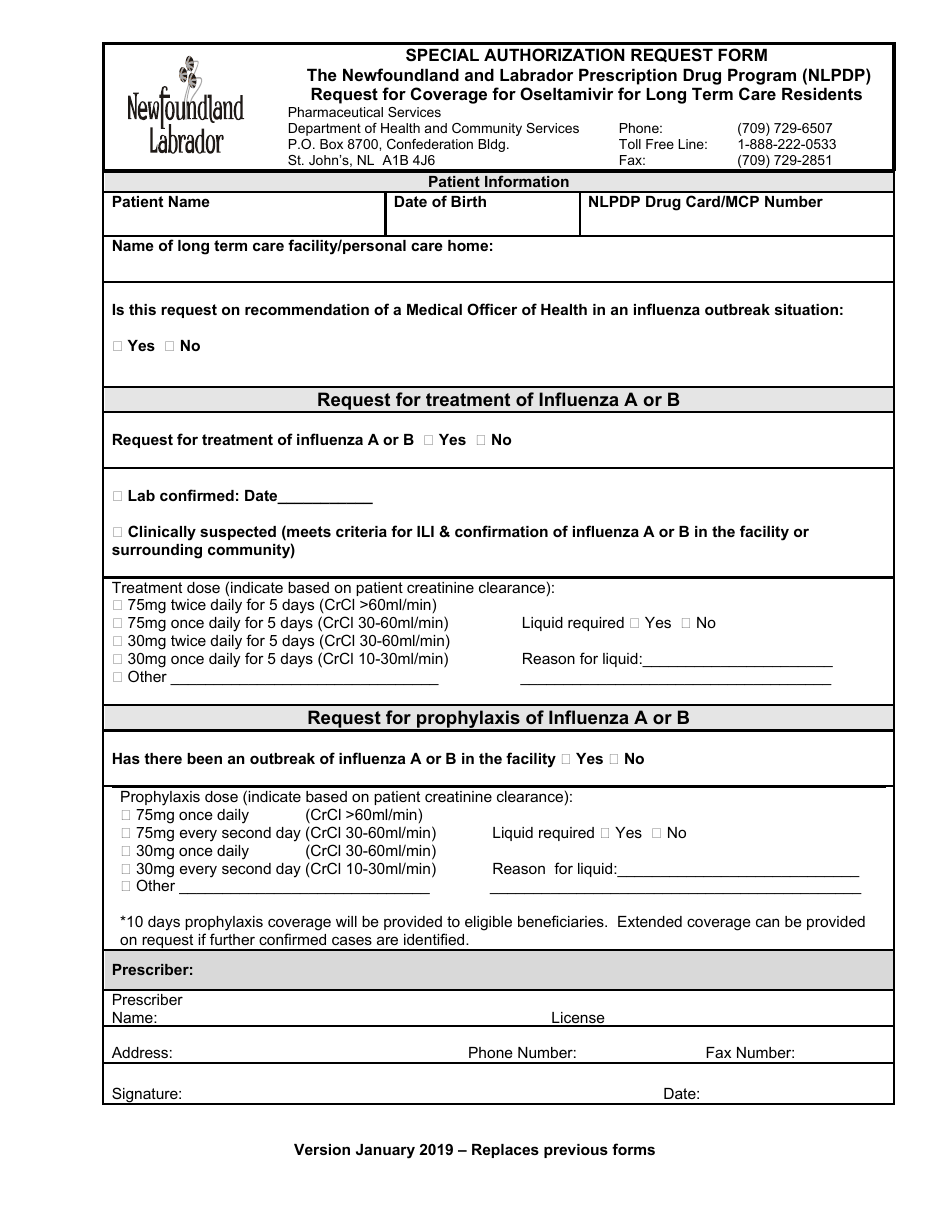
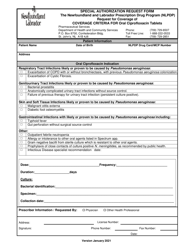
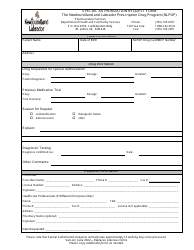
Special Authorization Request Form - Request for Coverage for Oseltamivir for Long Term Care Residents - Newfoundland and Labrador, Canada
The Special Authorization Request Form - Request for Coverage for Oseltamivir for Long Term Care Residents in Newfoundland and Labrador, Canada is used to request coverage for the medication called Oseltamivir for long-term care residents. This medication is commonly used for the treatment of influenza (flu) and this form helps to determine if the medication will be covered by the provincial healthcare system.
The Special Authorization Request Form for coverage of Oseltamivir for long-term care residents in Newfoundland and Labrador, Canada is typically filed by the healthcare provider or the prescribing physician.
FAQ
Q: What is the Special Authorization Request Form?
A: The Special Authorization Request Form is a document used to request coverage for Oseltamivir for Long Term Care residents in Newfoundland and Labrador, Canada.
Q: Who can use the Special Authorization Request Form?
A: The Special Authorization Request Form can be used by healthcare providers or facilities requesting coverage for Oseltamivir for their Long Term Care residents.
Q: What is Oseltamivir?
A: Oseltamivir is a medication used to treat and prevent influenza (flu) virus infections.
Q: Why is a special authorization required for coverage of Oseltamivir?
A: A special authorization is required for coverage of Oseltamivir to ensure appropriate and necessary use of the medication in Long Term Care residents.
Q: How can the Special Authorization Request Form be obtained?
A: The Special Authorization Request Form can be obtained from the healthcare provider or facility requesting coverage for Oseltamivir, or from the appropriate government agency in Newfoundland and Labrador, Canada.
Q: Are there any specific eligibility criteria for coverage of Oseltamivir?
A: Yes, there may be specific eligibility criteria for coverage of Oseltamivir for Long Term Care residents in Newfoundland and Labrador, Canada. These criteria may include age, medical condition, and other factors.
Q: What should be included in the Special Authorization Request Form?
A: The Special Authorization Request Form should include relevant patient information, medical history, reason for requesting coverage, and any supporting documentation or test results.
Q: How long does the special authorization process take?
A: The length of the special authorization process can vary. It is recommended to submit the Special Authorization Request Form well in advance of when coverage is needed.
Q: What happens after the Special Authorization Request Form is submitted?
A: After the Special Authorization Request Form is submitted, it will be reviewed by the appropriate agency or committee. A decision will be made regarding coverage and the requester will be notified.
Q: Is there an appeal process if the Special Authorization Request is denied?
A: Yes, there may be an appeal process available if the Special Authorization Request is denied. The specific process and requirements may vary depending on the jurisdiction.