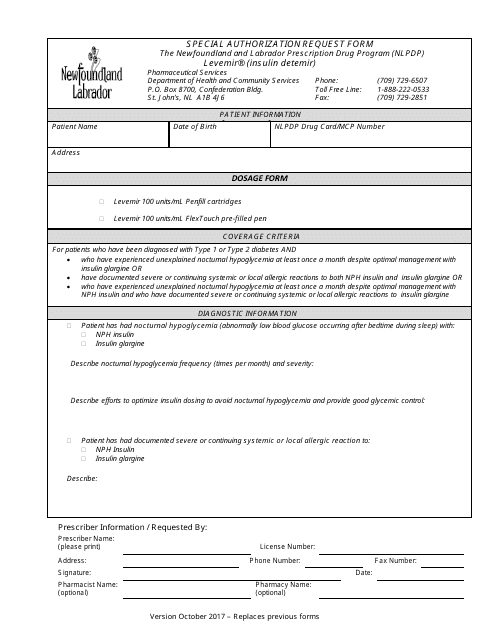
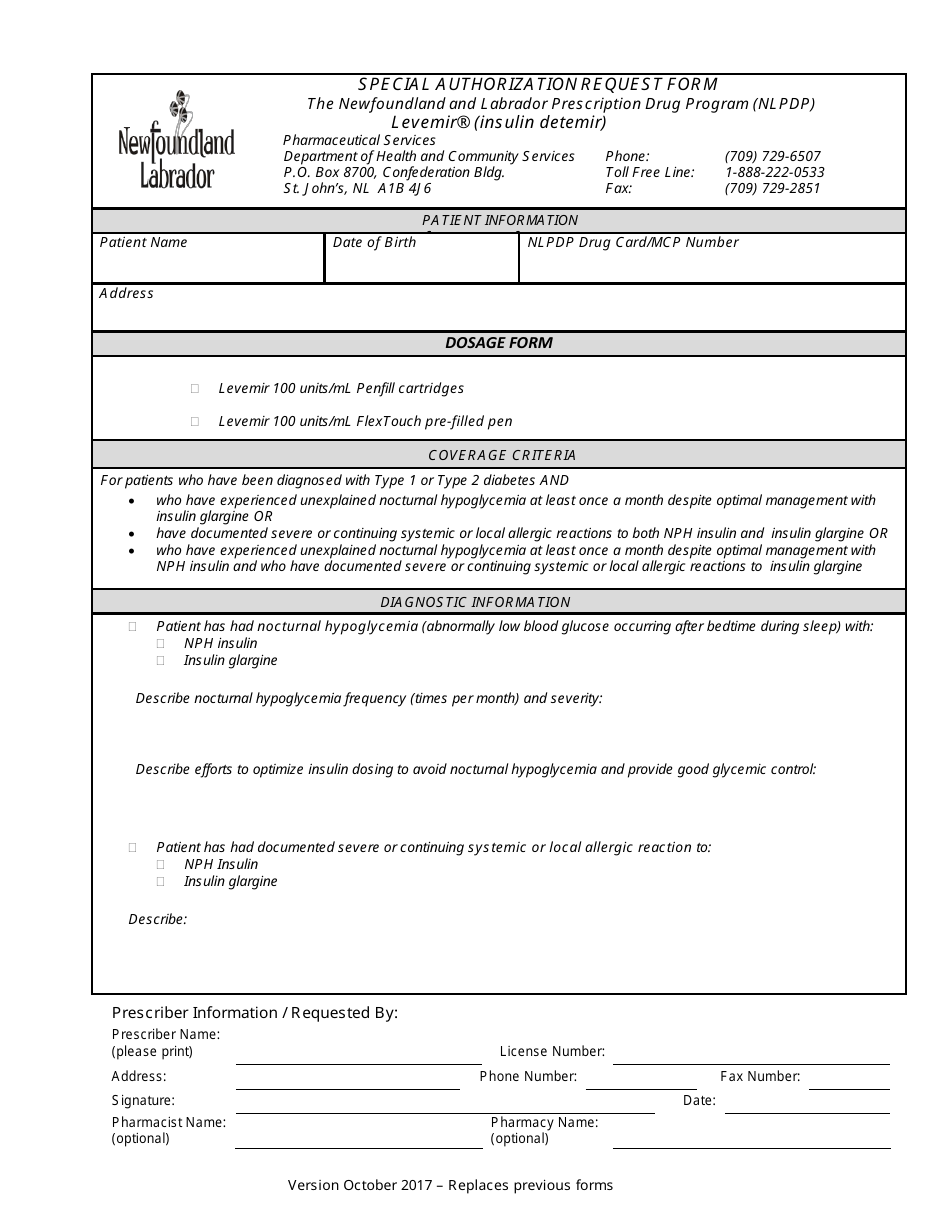
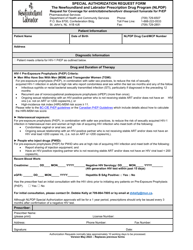
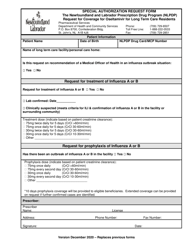
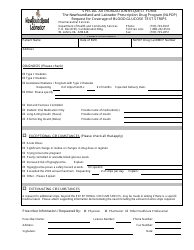
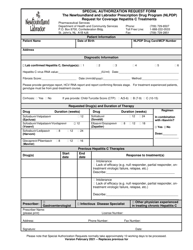
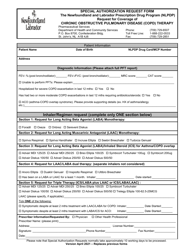
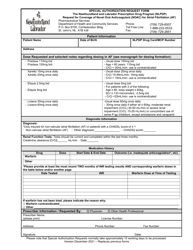
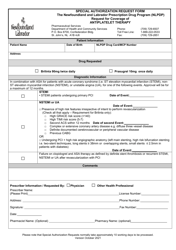
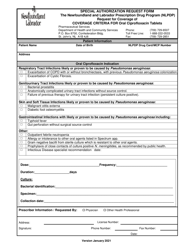
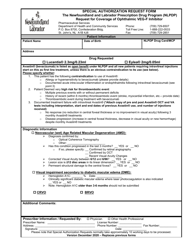
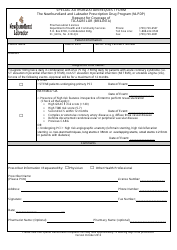
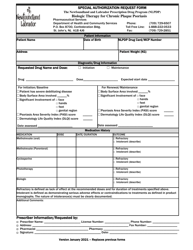
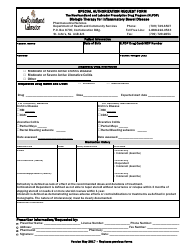
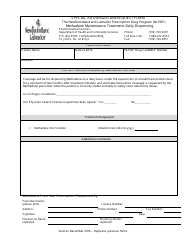
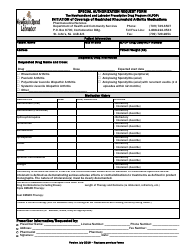
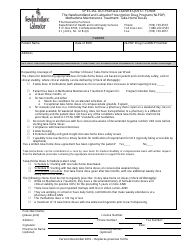
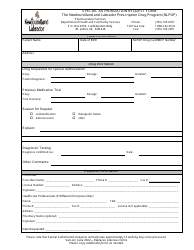
Special Authorization Request Form - Levemir (Insulin Detemir) - Newfoundland and Labrador, Canada
The Special Authorization Request Form for Levemir (Insulin Detemir) in Newfoundland and Labrador, Canada is used to request approval from the provincial government for coverage of this specific medication. It is required for individuals who need access to Levemir and want it to be covered under their healthcare plan in Newfoundland and Labrador.
The Special Authorization Request Form for Levemir (Insulin Detemir) in Newfoundland and Labrador, Canada is typically filed by the healthcare provider or physician for the patient.
FAQ
Q: What is a Special Authorization Request Form?
A: A Special Authorization Request Form is a document used to request coverage for a medication that may not be automatically covered by your insurance or government healthcare plan.
Q: What is Levemir (Insulin Detemir)?
A: Levemir (Insulin Detemir) is a type of insulin used to treat diabetes.
Q: Why would I need a Special Authorization Request Form for Levemir?
A: You may need a Special Authorization Request Form for Levemir if it is not automatically covered by your insurance or government healthcare plan.
Q: How can I obtain a Special Authorization Request Form for Levemir?
A: You can obtain a Special Authorization Request Form for Levemir from your healthcare provider or insurance company.
Q: What information is typically required on a Special Authorization Request Form?
A: A Special Authorization Request Form typically requires information such as the medication name, dosage, medical condition, and supporting documentation from your healthcare provider.
Q: What happens after I submit a Special Authorization Request Form for Levemir?
A: After you submit a Special Authorization Request Form for Levemir, it will be reviewed by your insurance or government healthcare plan to determine if coverage will be approved.
Q: How long does it take to get a response to a Special Authorization Request Form?
A: The response time for a Special Authorization Request Form can vary, but it is typically within a few weeks.
Q: What should I do if my Special Authorization Request Form is denied?
A: If your Special Authorization Request Form is denied, you can discuss alternative treatment options with your healthcare provider or appeal the decision with your insurance or government healthcare plan.
Q: Are there any fees associated with submitting a Special Authorization Request Form?
A: Fees may vary depending on your insurance or government healthcare plan. It is best to check with your provider for any associated fees.