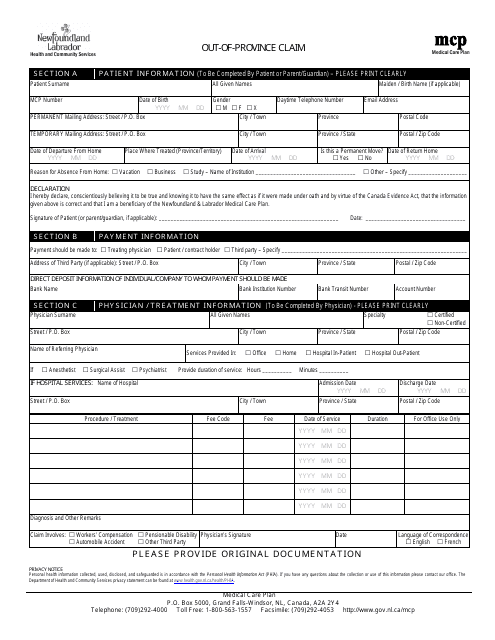
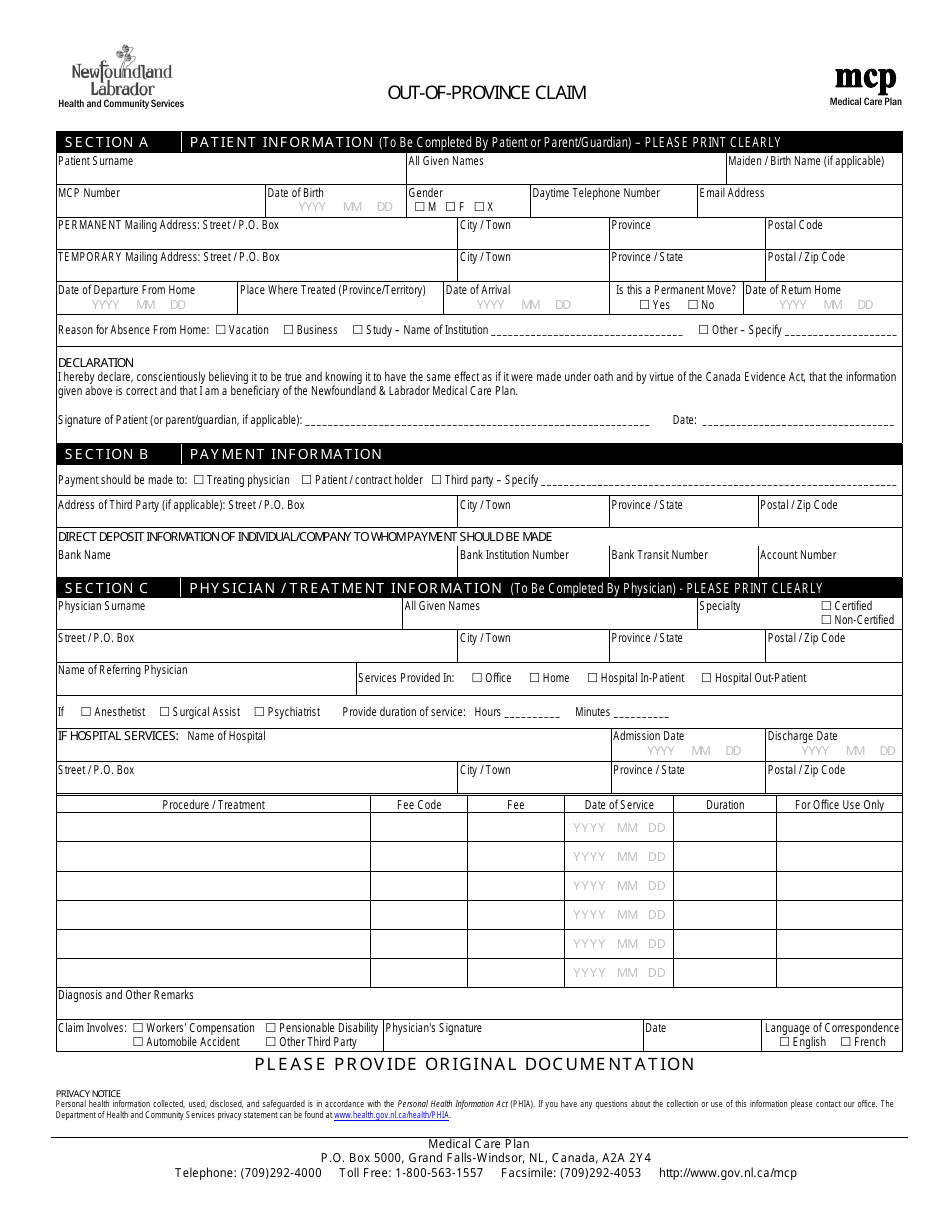
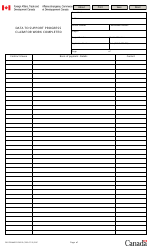
Out-Of-Province Claim - Newfoundland and Labrador, Canada
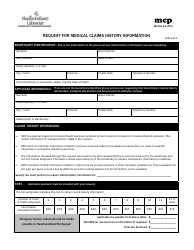
An Out-Of-Province Claim in Newfoundland and Labrador, Canada is a claim made by residents of the province when they receive medical services in another Canadian province or territory. This allows them to be reimbursed for the eligible expenses they incur while receiving healthcare outside of Newfoundland and Labrador.
In Newfoundland and Labrador, Canada, the individual who files the out-of-province claim is typically the patient themselves. They would need to submit the necessary documentation and information to their provincial health insurance plan in order to initiate the claim process.
FAQ
Q: What is an out-of-province claim?
A: An out-of-province claim is a claim for medical services or treatment received outside of your home province or territory.
Q: Am I eligible for an out-of-province claim in Newfoundland and Labrador?
A: Yes, if you are a resident of Newfoundland and Labrador and your medical services or treatment is not available within the province or requires specialized care that is not available locally.
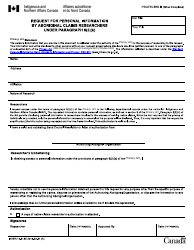
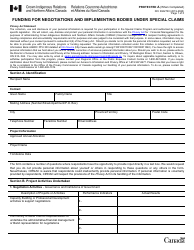
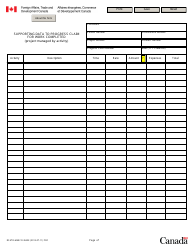
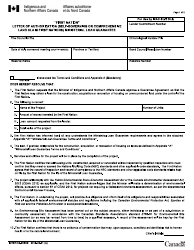
Q: What do I need to do to submit an out-of-province claim?
A: You need to obtain a referral from a healthcare provider in Newfoundland and Labrador, provide all necessary documentation, and submit your claim to the Medical Care Plan (MCP) office.
Q: What documents are required for an out-of-province claim?
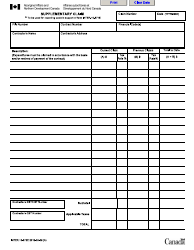
A: You need to provide the original itemized receipts for the medical services received, proof of out-of-province travel, a referral from a healthcare provider, and any other relevant supporting documentation.
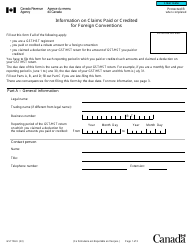
Q: How long does it take to process an out-of-province claim?
A: The processing time varies, but it typically takes around 30 business days for the Medical Care Plan (MCP) office to process and reimburse out-of-province claims.
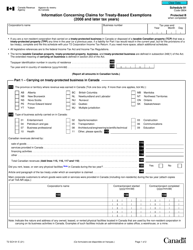
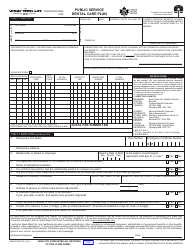
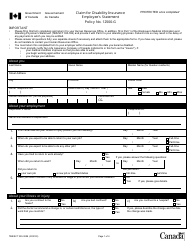
Q: What expenses are covered under an out-of-province claim?
A: The Medical Care Plan (MCP) office covers eligible medically necessary services and treatments received outside of Newfoundland and Labrador, subject to certain limitations and conditions.
Q: Are there any restrictions or limitations on out-of-province claims?
A: Yes, there are certain restrictions and limitations on out-of-province claims, including maximum reimbursement amounts, specified eligible services, and the requirement for prior approval in some cases.
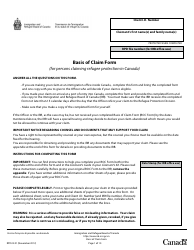
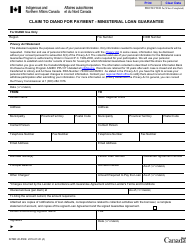
Q: Can I appeal a decision on my out-of-province claim?
A: Yes, if your claim is denied or if you disagree with the decision, you have the right to appeal the decision. You can contact the Medical Care Plan (MCP) office for more information on the appeals process.