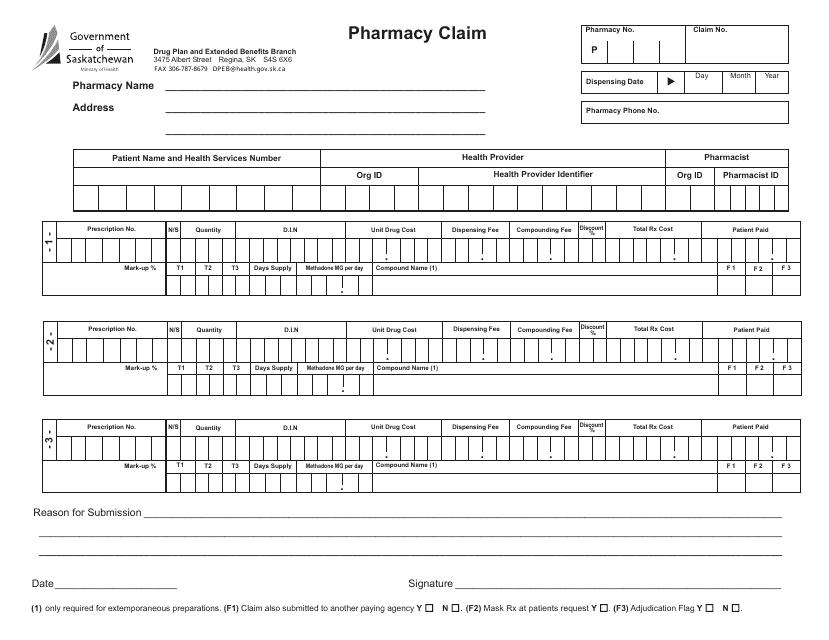
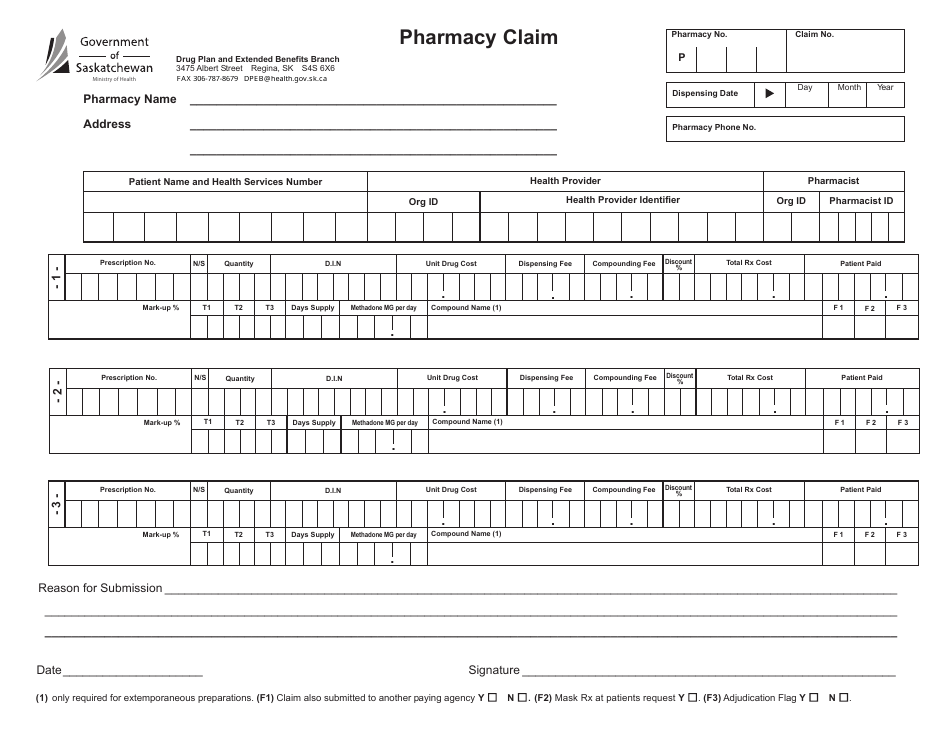
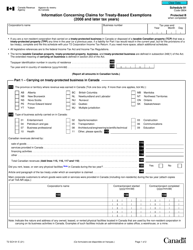
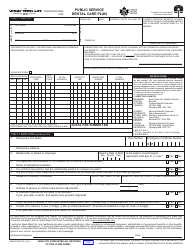
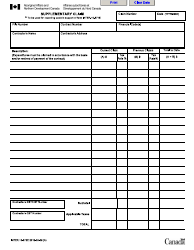
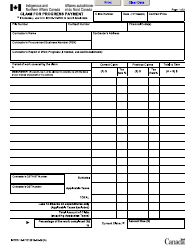
Pharmacy Claim - in Province - Saskatchewan, Canada
In Saskatchewan, Canada, a pharmacy claim is a document used to request reimbursement for prescription medications. It is typically submitted by a pharmacy on behalf of a patient to the provincial health insurance program, known as Saskatchewan Health. The claim includes details of the medication dispensed, the patient's personal information, and the amount being requested for reimbursement. The purpose of the pharmacy claim is to ensure that eligible individuals can access necessary medications while minimizing out-of-pocket expenses.
In Saskatchewan, Canada, the pharmacy usually files the claim with the provincial insurance program, known as the Saskatchewan Prescription Drug Plan (SPDP).
FAQ
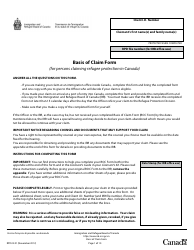
Q: What is a pharmacy claim?
A: A pharmacy claim is the process of submitting a request for reimbursement to the insurance company or government health program for the cost of medication purchased at a pharmacy.
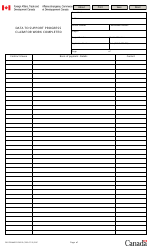
Q: How does a pharmacy claim work in Saskatchewan?
A: In Saskatchewan, pharmacy claims are processed through the Saskatchewan Prescription Drug Plan (SPDP). Eligible residents present their prescription and SPDP card at a participating pharmacy, and the pharmacy submits the claim electronically.
Q: Who is eligible for the Saskatchewan Prescription Drug Plan?
A: All residents of Saskatchewan are eligible for the Saskatchewan Prescription Drug Plan, regardless of their income or age.
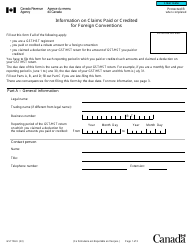
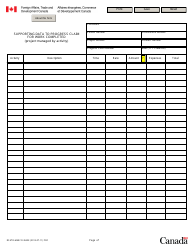
Q: Is there a cost to the patient for pharmacy claims in Saskatchewan?
A: Yes, patients are required to pay a portion of the cost of their medications through deductibles and co-payments. The amount varies depending on the individual's income and other factors.
Q: What information is required for a pharmacy claim in Saskatchewan?
A: To submit a pharmacy claim in Saskatchewan, the pharmacy needs information such as the patient's name, health card number, prescription details, and the pharmacy's information.
Q: How long does it take for a pharmacy claim to be processed in Saskatchewan?
A: Typically, pharmacy claims submitted through the SPDP are processed within a few business days, and reimbursement is issued directly to the pharmacy.
Q: Are all medications covered by the Saskatchewan Prescription Drug Plan?
A: No, not all medications are covered by the Saskatchewan Prescription Drug Plan. The plan has a formulary, which is a list of medications that are covered. Some medications may require special authorization or be subject to additional criteria.
Q: What should I do if my pharmacy claim is denied in Saskatchewan?
A: If your pharmacy claim is denied in Saskatchewan, you can contact the SPDP or your insurance company to inquire about the reason for denial and explore any possible appeals process.
Q: Can I use the Saskatchewan Prescription Drug Plan outside of the province?
A: The Saskatchewan Prescription Drug Plan is specific to residents of Saskatchewan and is not typically applicable outside the province. However, there may be exceptions or provisions for emergency situations.
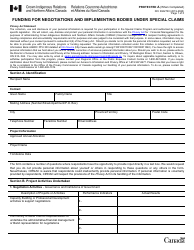
Q: Are there any exceptions for certain groups of people under the Saskatchewan Prescription Drug Plan?
A: Yes, certain groups such as seniors, children, and social assistance recipients may have different coverage and benefits under the Saskatchewan Prescription Drug Plan.