This version of the form is not currently in use and is provided for reference only. Download this version of
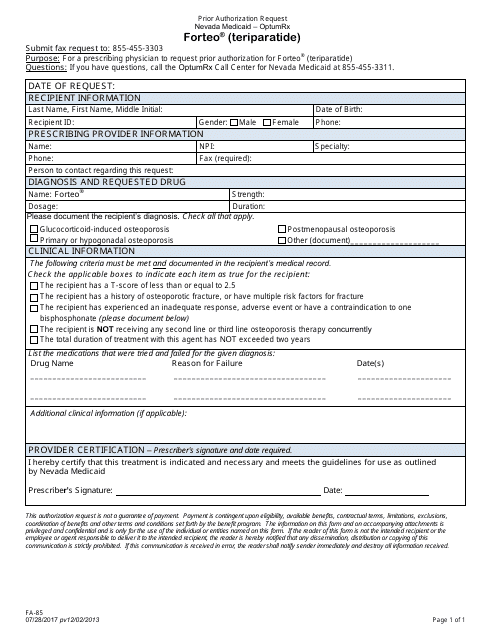
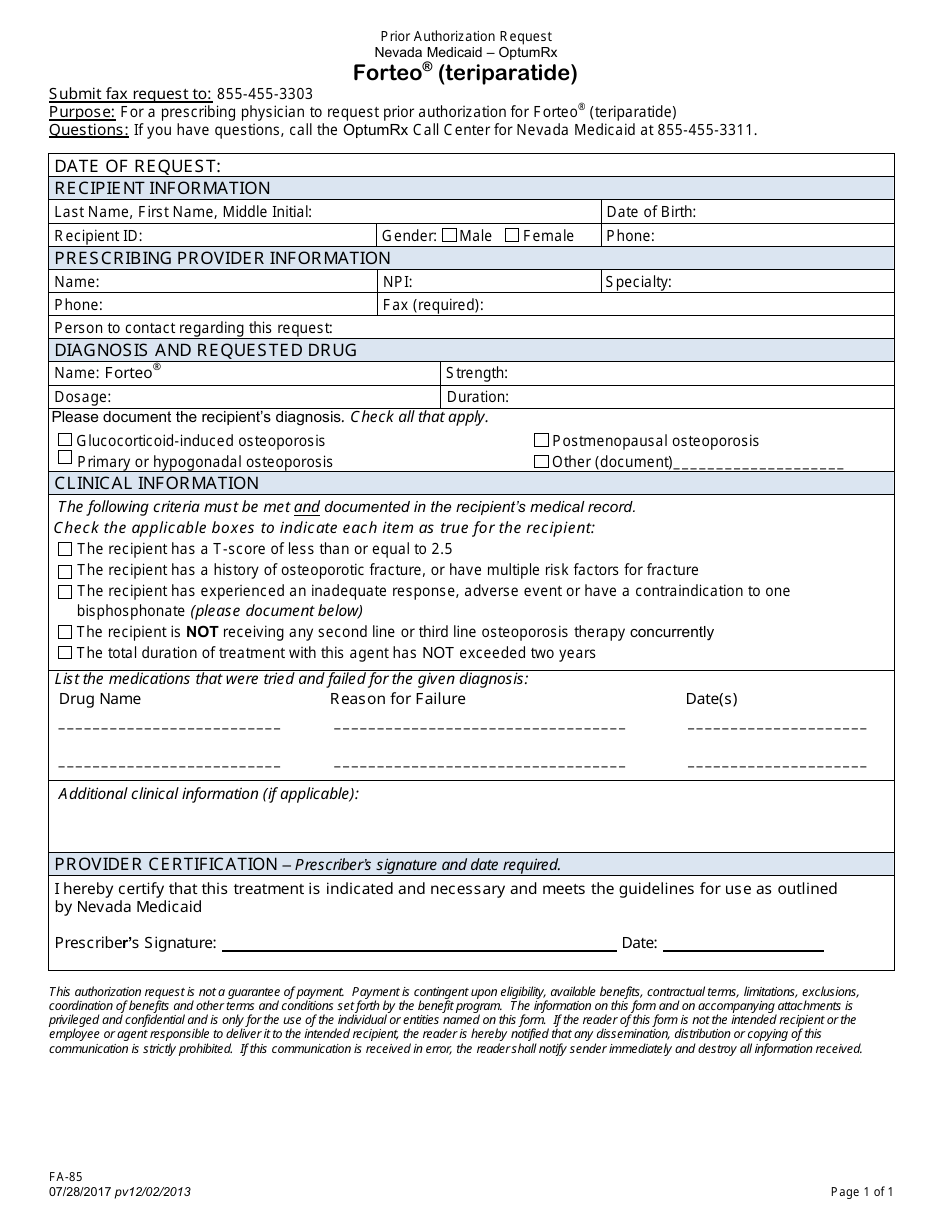
Form FA-85
for the current year.
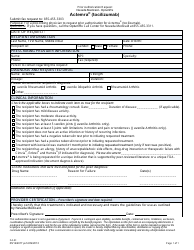
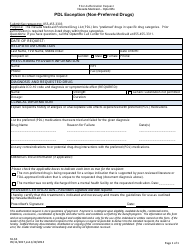
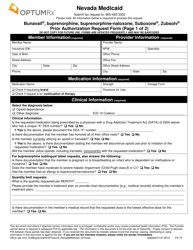
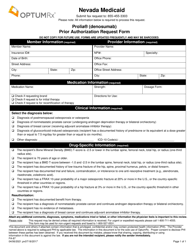
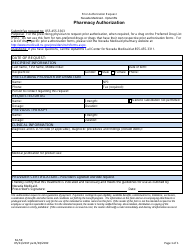
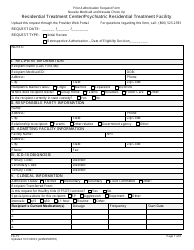
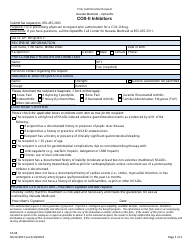
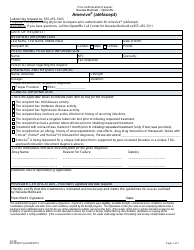
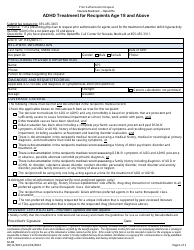
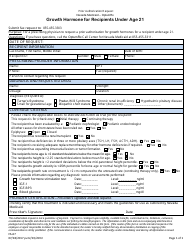
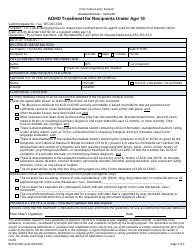
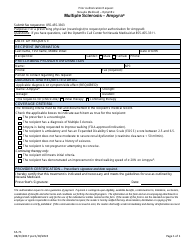
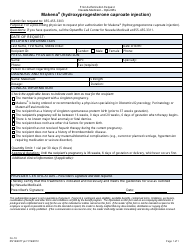
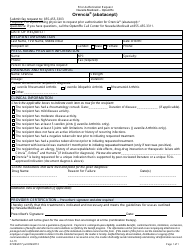
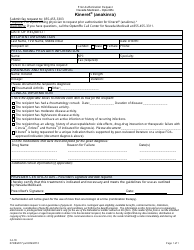
Form FA-85 Prior Authorization Reques - Forteo (Teriparatide) - Nevada
What Is Form FA-85?
This is a legal form that was released by the Nevada Department of Health and Human Services - a government authority operating within Nevada. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form FA-85?
A: Form FA-85 is a Prior Authorization Request form.
Q: What is Prior Authorization?
A: Prior Authorization is a process where the insurance company must approve the use of a specific medication before it is covered under the insurance plan.
Q: What is Forteo (Teriparatide)?
A: Forteo (Teriparatide) is a medication used to treat osteoporosis in women and men who are at high risk for bone fractures.
Q: Why do I need Prior Authorization for Forteo?
A: You need Prior Authorization for Forteo because it is a specialty medication that may require specific criteria to be met before it is covered.
Q: What information is needed on Form FA-85?
A: Form FA-85 requires information such as the patient's name, insurance information, prescribing physician, and medical justification for the use of Forteo.
Q: How long does the Prior Authorization process take?
A: The timeframe for Prior Authorization review varies, but it is typically completed within a few business days.
Q: What happens after Prior Authorization is approved?
A: After Prior Authorization is approved, the insurance company will cover the cost of Forteo as outlined in your insurance plan.
Q: What should I do if Prior Authorization is denied?
A: If Prior Authorization is denied, you may be able to appeal the decision by providing additional supporting documentation or discussing alternative treatment options with your prescribing physician.
Form Details:
- Released on July 28, 2017;
- The latest edition provided by the Nevada Department of Health and Human Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form FA-85 by clicking the link below or browse more documents and templates provided by the Nevada Department of Health and Human Services.