This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
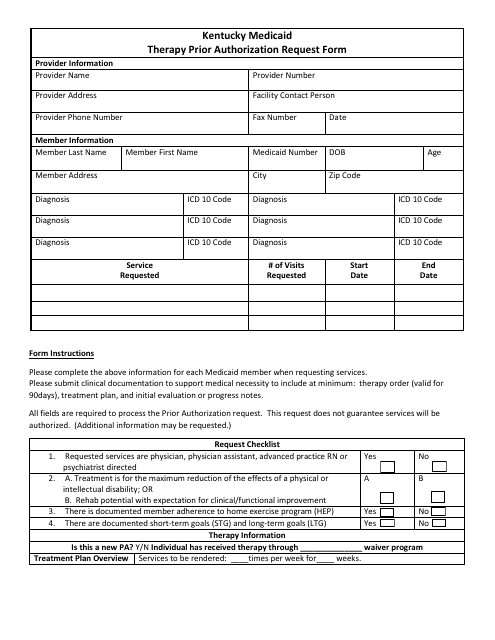
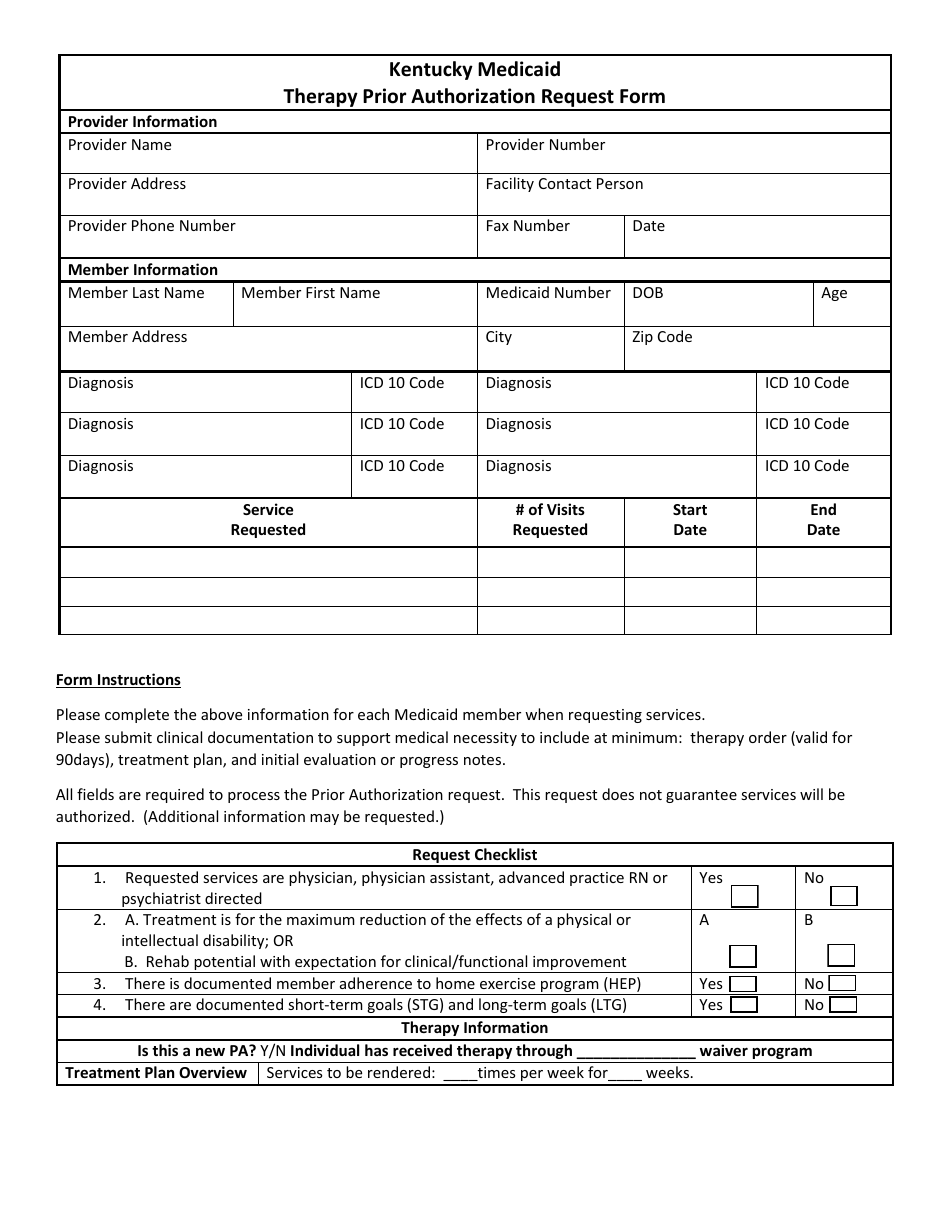
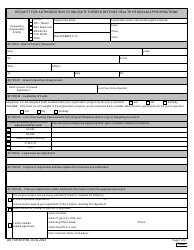
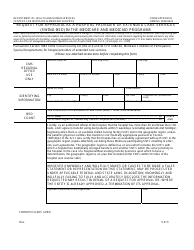
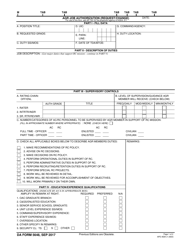
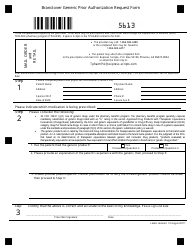
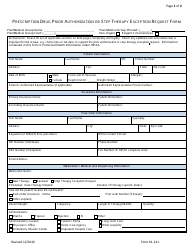
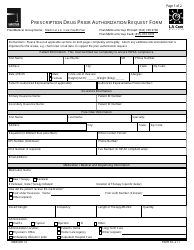
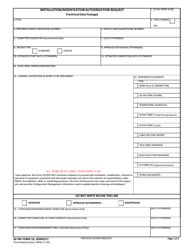
Kentucky Medicaid Therapy Prior Authorization Request Form - Kentucky
Kentucky Medicaid Therapy Prior Authorization Request Form is a legal document that was released by the Kentucky Department for Medicaid Services - a government authority operating within Kentucky.
FAQ
Q: What is the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: The Kentucky Medicaid Therapy Prior Authorization Request Form is a form that needs to be filled out to request prior authorization for therapy services under Kentucky Medicaid.
Q: Why do I need to fill out the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: You need to fill out the Kentucky Medicaid Therapy Prior Authorization Request Form to obtain approval for therapy services and ensure that they will be covered by Kentucky Medicaid.
Q: Who is eligible to fill out the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: Healthcare providers or their designated representatives can fill out the Kentucky Medicaid Therapy Prior Authorization Request Form on behalf of the Medicaid recipients.
Q: Are there any fees associated with the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: No, there are no fees associated with the Kentucky Medicaid Therapy Prior Authorization Request Form. It is a free service provided by Kentucky Medicaid.
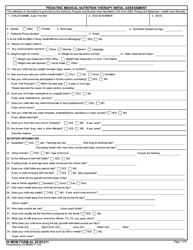
Q: What information do I need to provide on the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: You will need to provide information such as the Medicaid recipient's name, Medicaid ID number, diagnosis, requested therapy services, and supporting documentation.
Q: How long does it take to process the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: The processing time for the Kentucky Medicaid Therapy Prior Authorization Request Form varies, but it typically takes a few business days to review and respond to the request.
Q: What happens after I submit the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: After you submit the Kentucky Medicaid Therapy Prior Authorization Request Form, it will be reviewed by Kentucky Medicaid to determine if the therapy services are medically necessary and meet the coverage criteria.
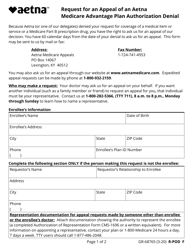
Q: What do I do if my Kentucky Medicaid Therapy Prior Authorization Request Form is denied?
A: If your Kentucky Medicaid Therapy Prior Authorization Request Form is denied, you have the right to appeal the decision and request a reconsideration by providing additional information or documentation to support the request.
Form Details:
- The latest edition currently provided by the Kentucky Department for Medicaid Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Kentucky Department for Medicaid Services.