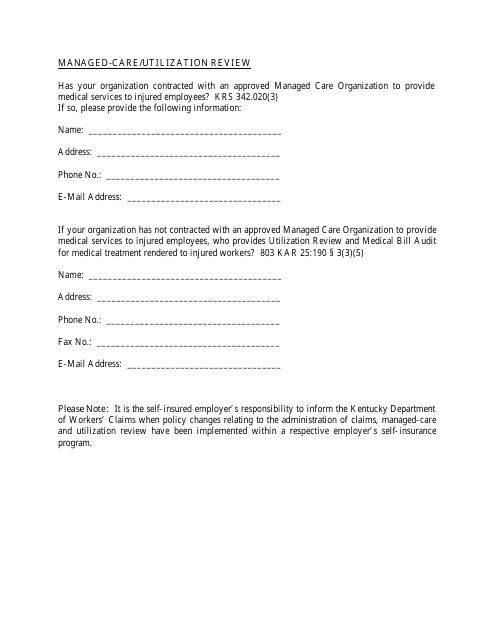
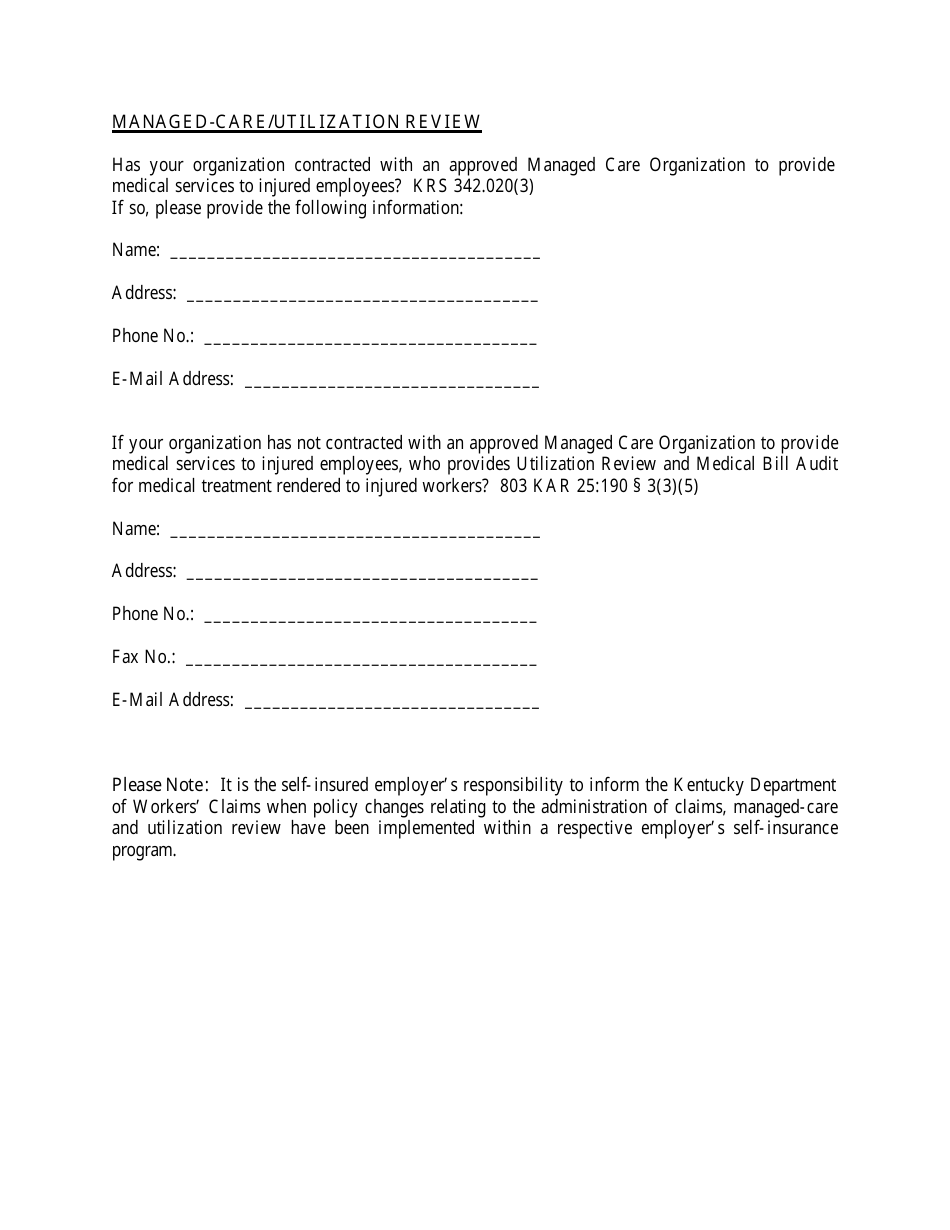
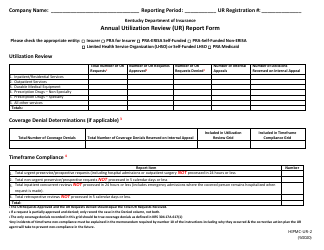
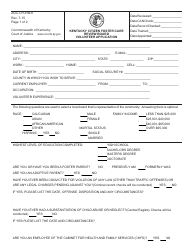
Managed-Care / Utilization Review - Kentucky
Managed-Care/Utilization Review is a legal document that was released by the Kentucky Labor Cabinet - a government authority operating within Kentucky.
FAQ
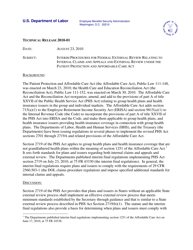
Q: What is managed care?
A: Managed care is a system of healthcare delivery where insurance companies or organizations manage and coordinate healthcare services for their members.
Q: What is utilization review?
A: Utilization review is a process used by insurance companies to evaluate the appropriateness and necessity of medical treatments and services.
Q: Why is utilization review important?
A: Utilization review helps ensure that healthcare services are provided in the most effective and cost-efficient manner.
Q: Who conducts utilization review in Kentucky?
A: Utilization review in Kentucky is typically conducted by insurance companies or organizations contracted by the insurance companies.
Q: What happens during the utilization review process?
A: During utilization review, medical professionals review medical records and treatment plans to determine if they meet established criteria for coverage.
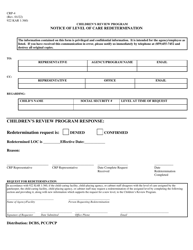
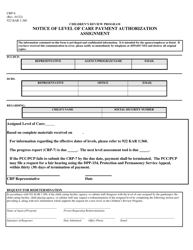
Q: Can utilization review result in denial of coverage?
A: Yes, utilization review can result in denial of coverage if the requested treatment or service is deemed not medically necessary or appropriate.
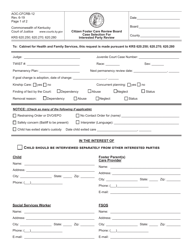
Q: Can patients appeal a denial of coverage?
A: Yes, patients have the right to appeal a denial of coverage and can follow the established appeals process with their insurance company.
Form Details:
- The latest edition currently provided by the Kentucky Labor Cabinet;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Kentucky Labor Cabinet.