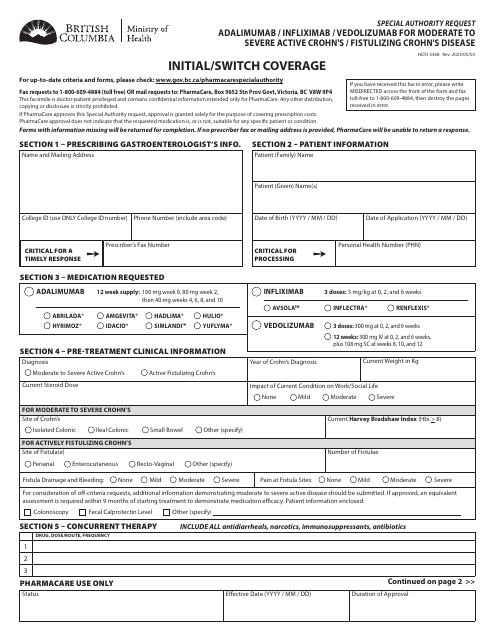
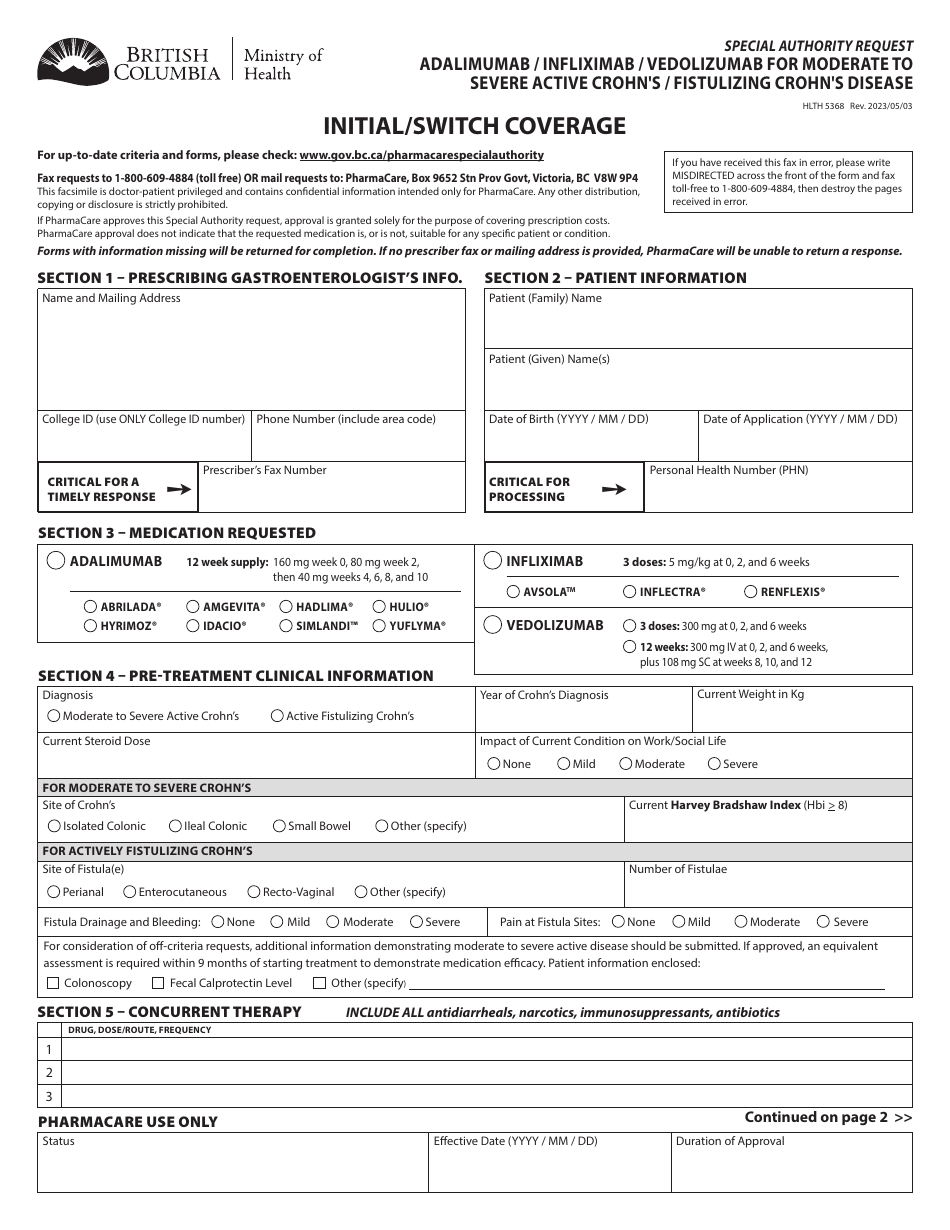
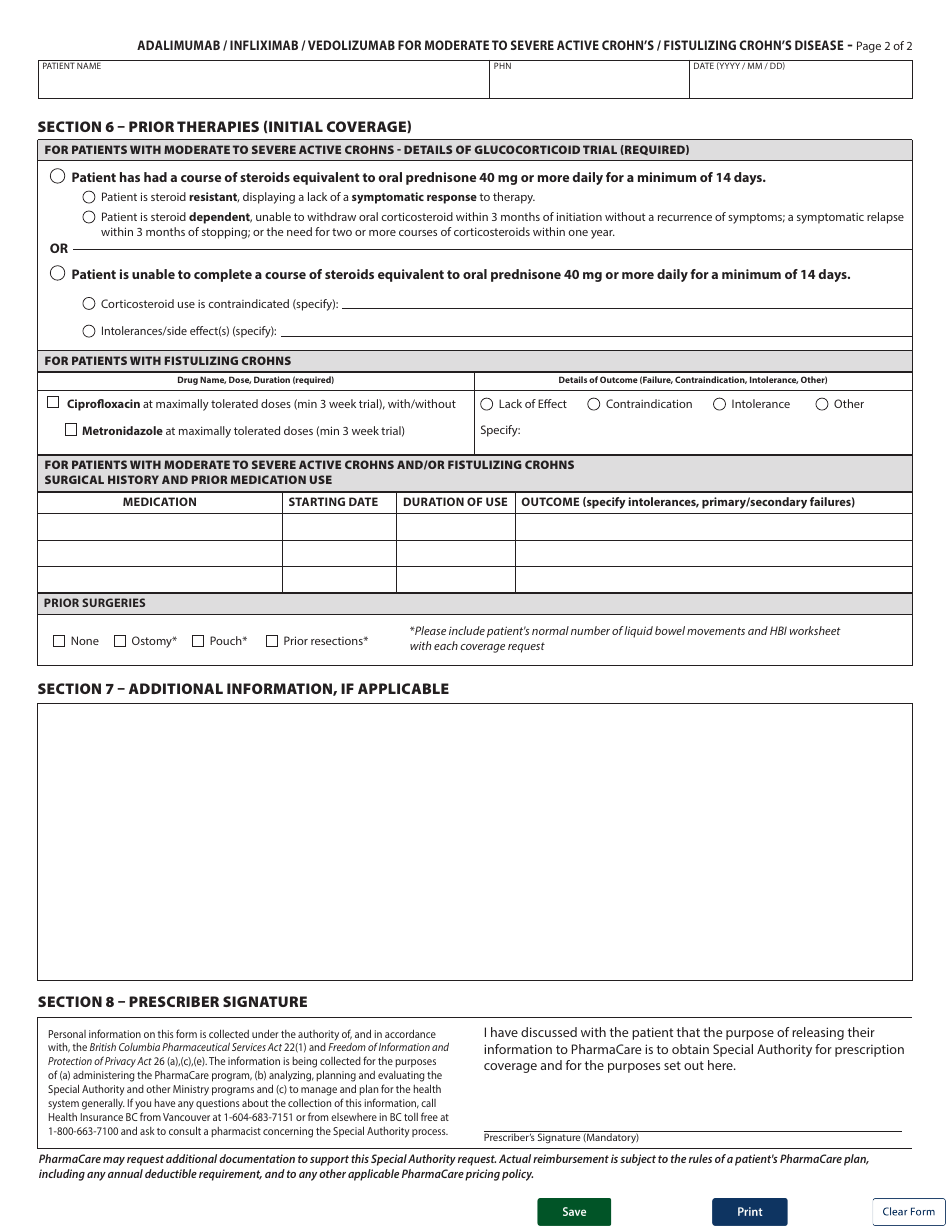
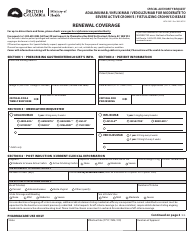
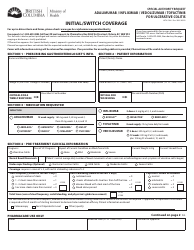
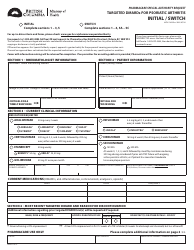
Form HLTH5368 Special Authority Request - Adalimumab / Infliximab / Vedolizumab for Moderate to Severe Active Crohn's / Fistulizing Crohn's Disease: Initial / Switch Coverage - British Columbia, Canada
Form HLTH5368 Special Authority Request - Adalimumab/Infliximab/Vedolizumab for Moderate to Severe Active Crohn's/Fistulizing Crohn's Disease: Initial/Switch Coverage is a document used in British Columbia, Canada to request special authorization for coverage of medications (Adalimumab, Infliximab, or Vedolizumab) for the treatment of moderate to severe active Crohn's disease or fistulizing Crohn's disease. It is used when initiating treatment or when switching medications for this condition.
The Form HLTH5368 is typically filed by the patient or their authorized representative, with the support of their healthcare provider, in British Columbia, Canada.
Form HLTH5368 Special Authority Request - Adalimumab/Infliximab/Vedolizumab for Moderate to Severe Active Crohn's/Fistulizing Crohn's Disease: Initial/Switch Coverage - British Columbia, Canada - Frequently Asked Questions (FAQ)
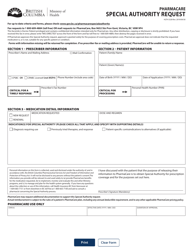
Q: What is the Special Authority Request form for?
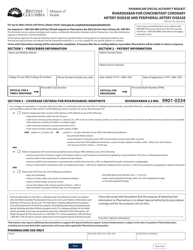
A: The Special Authority Request form is for requesting coverage of Adalimumab, Infliximab, or Vedolizumab for Moderate to Severe Active Crohn's/Fistulizing Crohn's Disease.
Q: Who is eligible to use this Special Authority Request form?
A: Patients in British Columbia, Canada with Moderate to Severe Active Crohn's/Fistulizing Crohn's Disease who require coverage for Adalimumab, Infliximab, or Vedolizumab.
Q: What conditions are covered by this Special Authority Request?
A: This Special Authority Request form is for coverage of Adalimumab, Infliximab, or Vedolizumab for Moderate to Severe Active Crohn's Disease or Fistulizing Crohn's Disease.
Q: What is the purpose of the Special Authority Request?
A: The purpose of the Special Authority Request is to request coverage for Adalimumab, Infliximab, or Vedolizumab in the treatment of Moderate to Severe Active Crohn's Disease or Fistulizing Crohn's Disease.
Q: What do I need to include when submitting the Special Authority Request?
A: When submitting the Special Authority Request, you will need to include relevant medical documentation, such as diagnosis, previous treatment history, and clinical rationale for the requested medication.
Q: Who can assist me with completing the Special Authority Request?
A: Your healthcare provider, such as your physician or specialist, can assist you with completing the Special Authority Request.
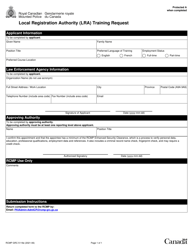
Q: How long does the Special Authority Request process take?
A: The processing time for the Special Authority Request may vary, but it typically takes several weeks to receive a decision.
Q: What happens if my Special Authority Request is approved?
A: If your Special Authority Request is approved, you will receive coverage for Adalimumab, Infliximab, or Vedolizumab as prescribed by your healthcare provider.
Q: What happens if my Special Authority Request is denied?
A: If your Special Authority Request is denied, you may wish to discuss alternative treatment options with your healthcare provider or appeal the decision if you believe it was made in error.