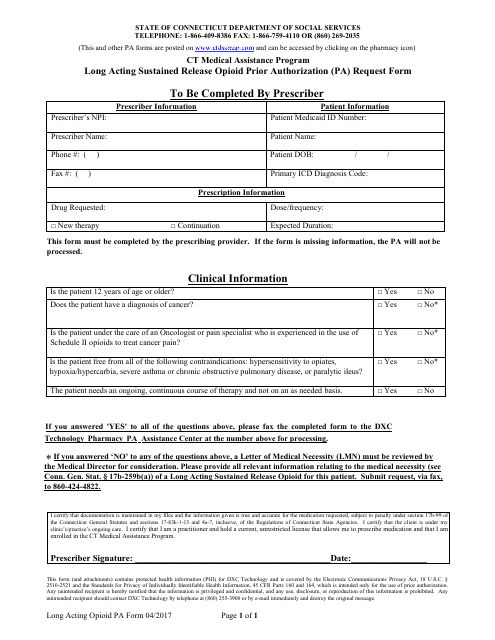
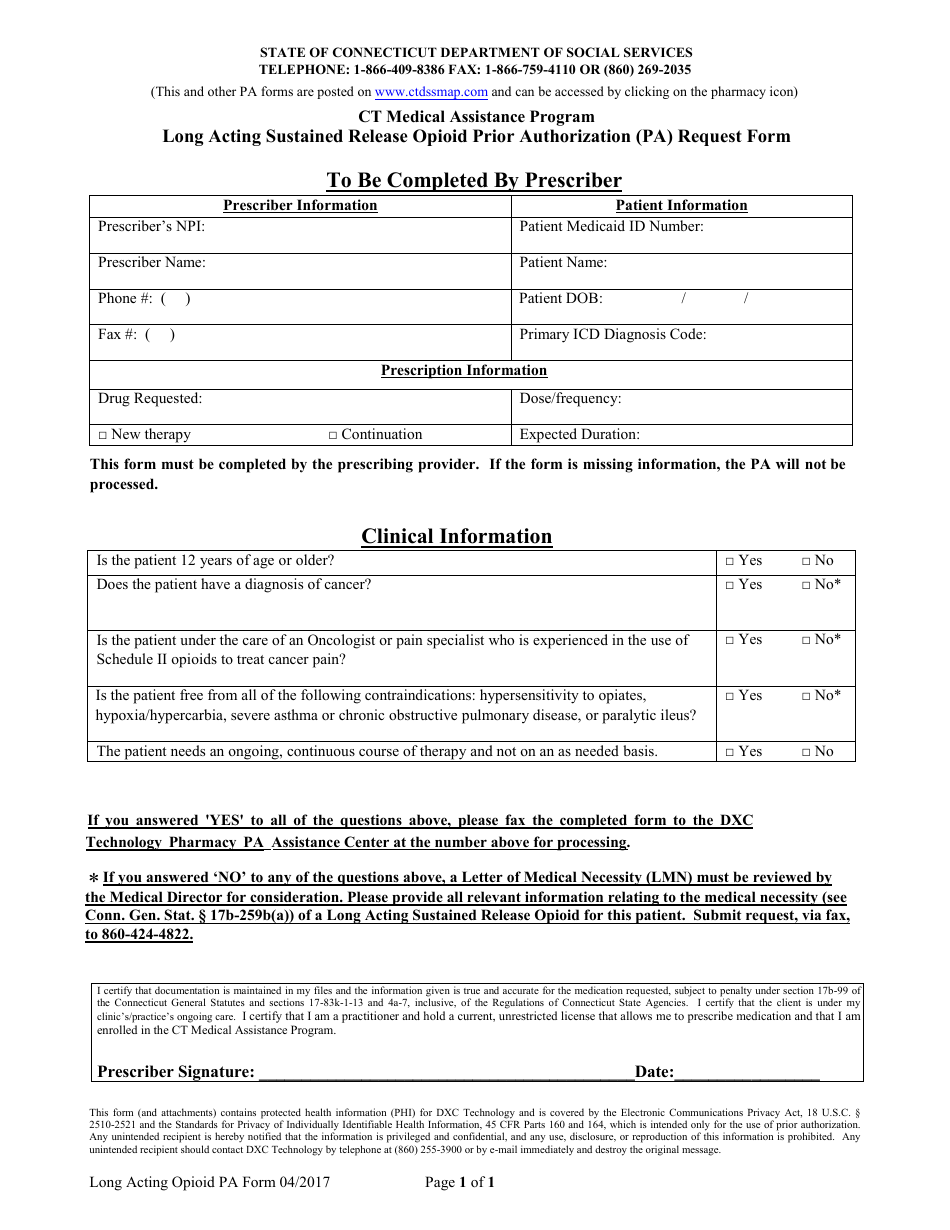
Long Acting Sustained Release Opioid Prior Authorization (Pa) Request Form - Ct Medical Assistance Program - Connecticut
Long Acting Sustained Release Opioid Prior Authorization (Pa) Request Form - Ct Medical Assistance Program is a legal document that was released by the Connecticut State Department of Social Services - a government authority operating within Connecticut.
FAQ
Q: What is the Long Acting Sustained Release Opioid Prior Authorization (PA) Request Form?
A: It is a form used in the Connecticut Medical Assistance Program to request prior authorization for long acting sustained release opioids.
Q: What is prior authorization?
A: It is a process in which healthcare providers must obtain approval from the insurance company or government program before prescribing certain medications or treatments.
Q: Why is prior authorization required for long acting sustained release opioids?
A: Prior authorization helps ensure appropriate and safe use of opioids and prevents misuse or overuse.
Q: Who uses the Long Acting Sustained Release Opioid Prior Authorization (PA) Request Form?
A: Healthcare providers who participate in the Connecticut Medical Assistance Program use this form.
Q: What information is required on the Long Acting Sustained Release Opioid Prior Authorization (PA) Request Form?
A: The form typically requires information about the patient, healthcare provider, diagnosis, and rationale for prescribing the long acting sustained release opioid.
Q: Is prior authorization always required for long acting sustained release opioids?
A: Yes, in the Connecticut Medical Assistance Program, prior authorization is required for these medications.
Q: How long does it take to get a prior authorization for long acting sustained release opioids?
A: The time frame for obtaining a prior authorization can vary, but it typically takes a few days to a week.
Q: What happens if a prior authorization for long acting sustained release opioids is denied?
A: If the prior authorization is denied, the healthcare provider may need to explore alternative treatment options or submit an appeal to reconsider the decision.
Q: Can patients submit the Long Acting Sustained Release Opioid Prior Authorization (PA) Request Form themselves?
A: No, the form must be completed and submitted by the healthcare provider.
Form Details:
- Released on April 1, 2017;
- The latest edition currently provided by the Connecticut State Department of Social Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Connecticut State Department of Social Services.