Pharmacy Benefits Templates
Pharmacy Benefits - Your Guide to Affordable Medications
Welcome to our comprehensive resource on pharmacy benefits, also known as pharmacy benefit management (PBM) programs. Whether you're a healthcare provider, a payer or a consumer, understanding pharmacy benefits is crucial in maximizing the value of your healthcare services.
Pharmacy benefits refer to the range of services and discounts offered to individuals and organizations to help them afford necessary prescription medications. Also known as pharmacy benefit management or pharmacy benefit programs, these initiatives ensure access to affordable drugs while maintaining the highest quality of care.
Our website serves as your one-stop-shop for all things related to pharmacy benefits. From understanding the complex world of pharmacy benefit managers to navigating prior authorization processes, we provide you with the information you need to make informed decisions about your healthcare.
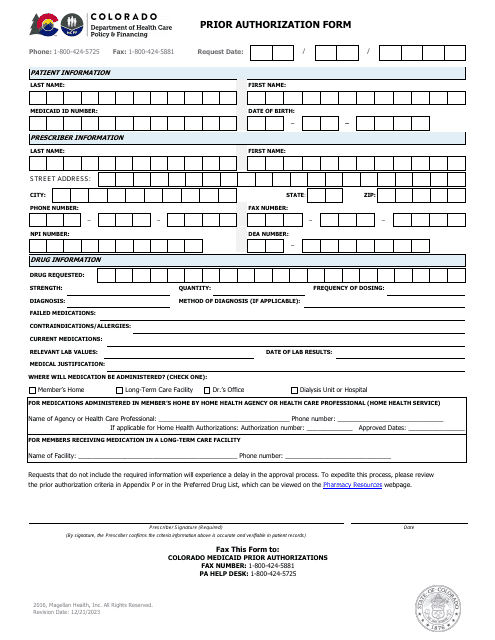
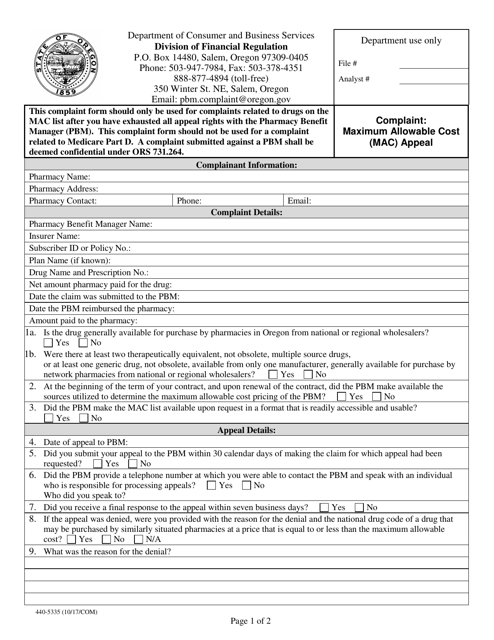
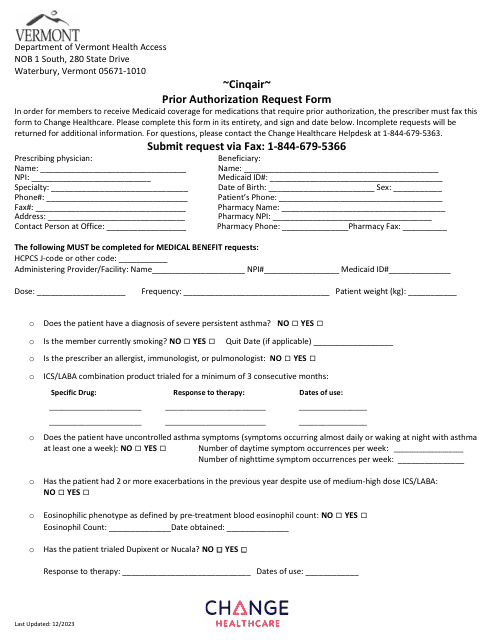
Explore our extensive collection of documents, such as the Form 440-5335 Pharmacy Benefit Manager Complaint: Maximum Allowable Cost (Mac) Appeal - Oregon or the Cinqair Prior Authorization Request Form - Vermont. These resources will help you understand the intricacies of pharmacy benefit management and empower you to take control of your prescription drug needs.
Pharmacy benefits are commonly referred to by various names, including pharmacy benefit programs or simply pharmacy benefits. We've curated a vast range of documents under these alternate names to ensure you find the information you need easily and efficiently.
At our website, you'll find a wealth of information, including tips on cost-saving strategies, guidance on navigating prior authorization processes, and insights into the latest developments in pharmacy benefits. We aim to empower you with the knowledge and resources required to optimize your healthcare experience.
Unlock the potential of pharmacy benefits and discover a world of affordable medications. Start exploring our extensive collection of documents and take control of your pharmacy benefit experience today.
Documents:
10
This document is a form used in Oregon for filing a complaint against a Pharmacy Benefit Manager regarding Maximum Allowable Cost (MAC) appeals.
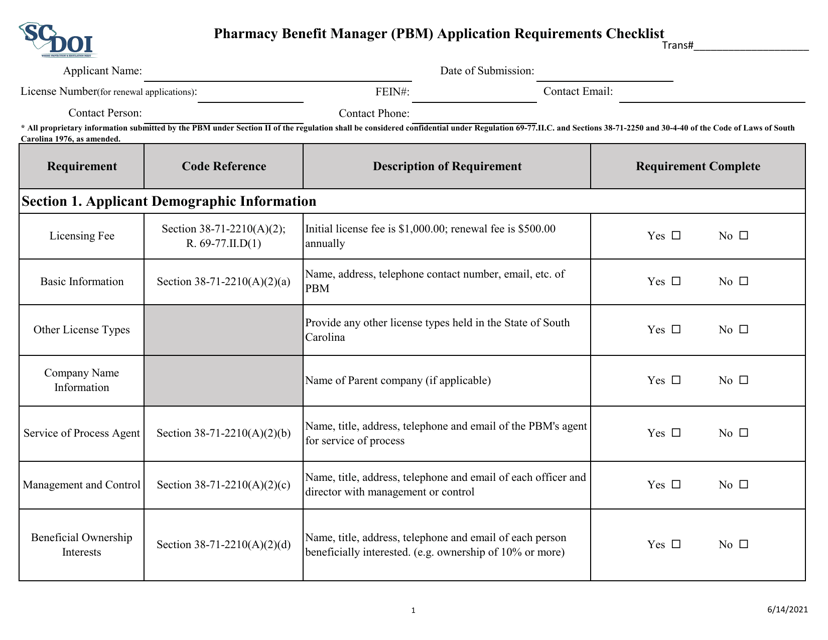
This document is a checklist outlining the application requirements for becoming a Pharmacy Benefit Manager (PBM) in South Carolina. It contains the necessary information and steps that need to be followed to apply for PBM licensure in the state.
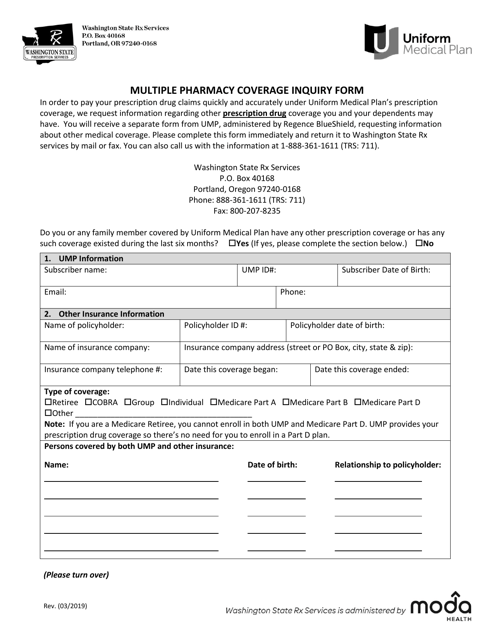
This form is used for inquiring about multiple pharmacy coverage in the state of Washington.
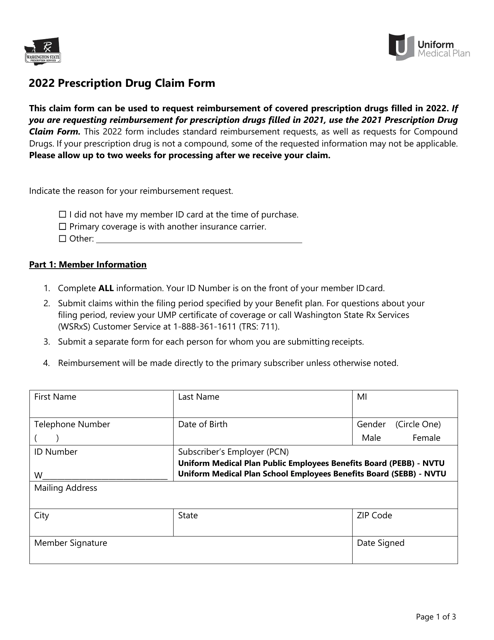
This form is used for filing prescription drug claims in the state of Washington. It allows individuals to seek reimbursement for the cost of prescribed medications.
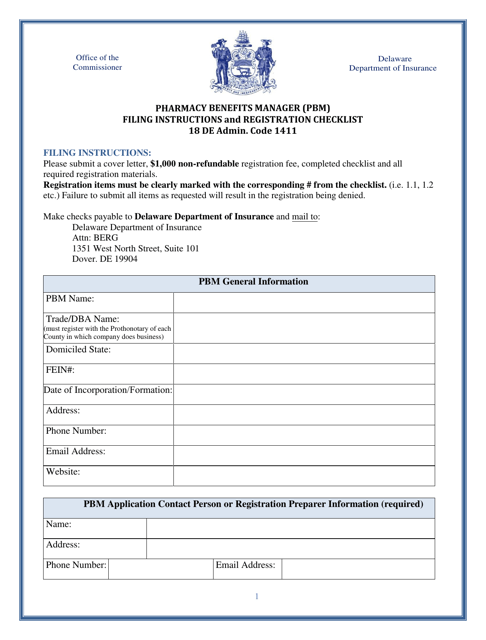
This document is for the registration of Pharmacy Benefits Managers in the state of Delaware. It includes a checklist of requirements that must be completed for the registration process.
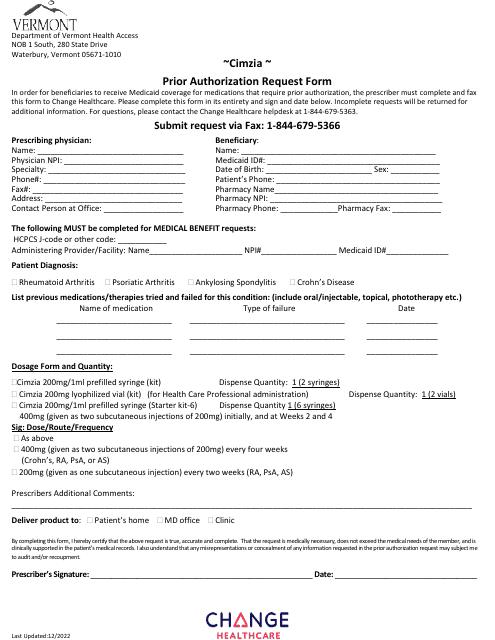
This Form is used for submitting a prior authorization request for Cimzia medication in the state of Vermont.
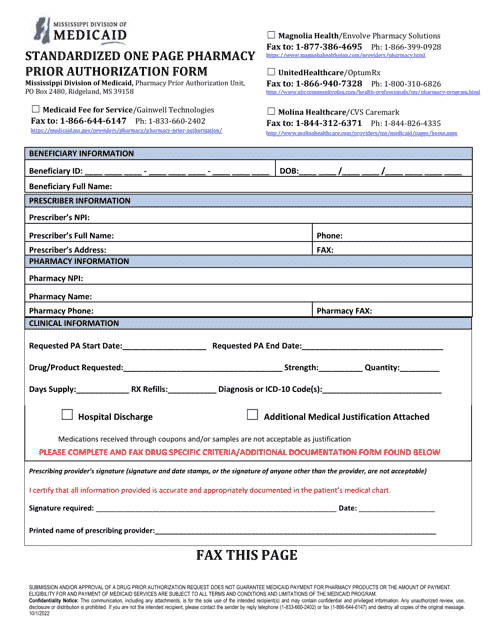
This document is used for obtaining prior authorization for opioids in the state of Mississippi. It includes the necessary paperwork and information required to request approval for the use of these medications.
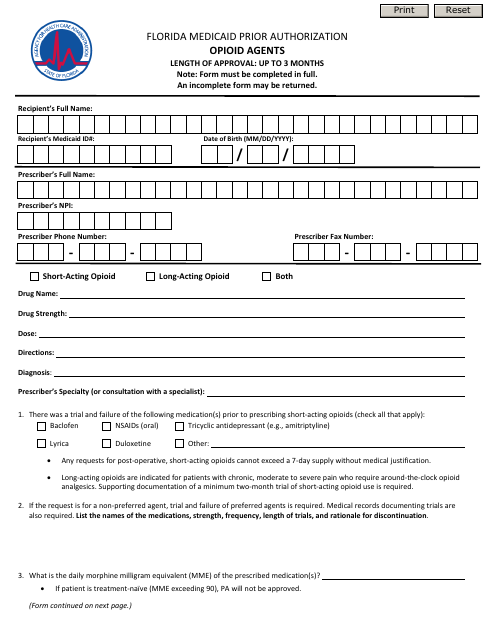
This form is used for obtaining prior authorization for opioid agents under Florida Medicaid in the state of Florida.