Insurance Appeal Letter Templates and Samples
An Insurance Appeal Letter is a formal letter prepared by an insurance policyholder and sent to their insurer to ask the latter to review their request for compensation or coverage again, schedule a hearing to let the insured individual present their case, and file documents that shed new light on the insurance claim that may lead to a decision favorable for the claimant. Whether your health coverage was terminated or the insurance provider has denied you a payment for a claim, an Appeal Letter to an Insurance Company is the best way to protect your interests as a patient, request the recipient to review their decision, or at the very least to provide you with a better explanation of the issue so that in the future you avoid the same mistake and do not lose more money or time.
Insurance Appeal Letter Types
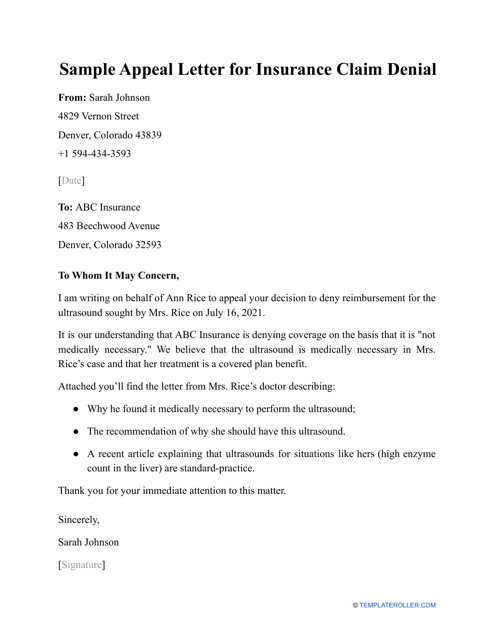
- Sample Appeal Letter for Insurance Claim Denial. This is a generic Appeal Letter for Insurance that can be used in a variety of circumstances - you have not disclosed the information that was requested, you have reached the limit of your existing coverage, or your medical evaluation was not comprehensive enough;
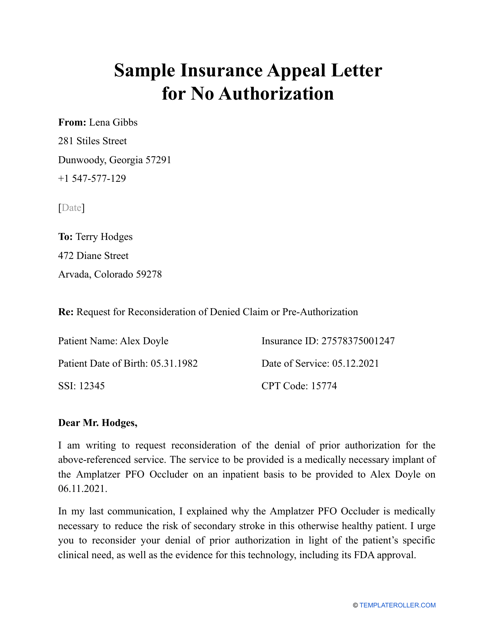
- Sample Insurance Appeal Letter for No Authorization. Fill out this template to contest the denial of insurance coverage in case your claim was turned down because the prescription, procedure, or treatment needed prior authorization from the insurer, not just the medical professional;
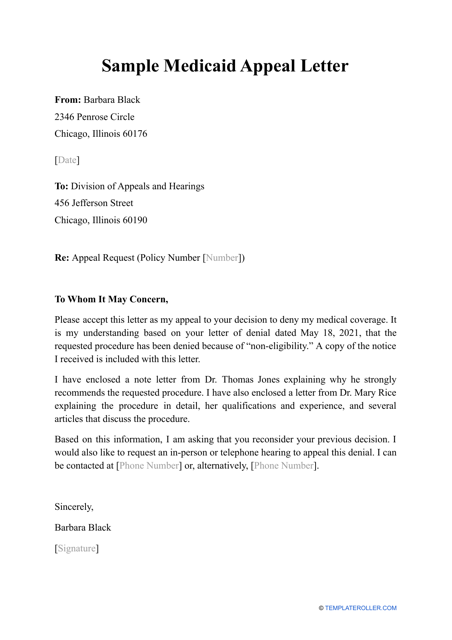
- Sample Medicaid Appeal Letter. If your Medicaid claim was denied, your income is low, and you are unable to cover medical expenses, you still have a chance to finance your treatment and qualify for this program for the first time or enroll again using this Insurance Claim Appeal Letter;
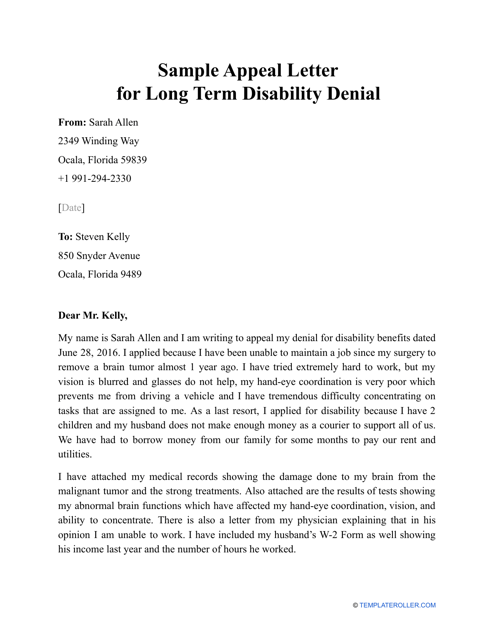
- A Sample Appeal Letter for Long Term Disability Denial can be drafted to dispute the denial of insurance policy coverage in case you are incapable of carrying out your regular job duties for three months or longer;
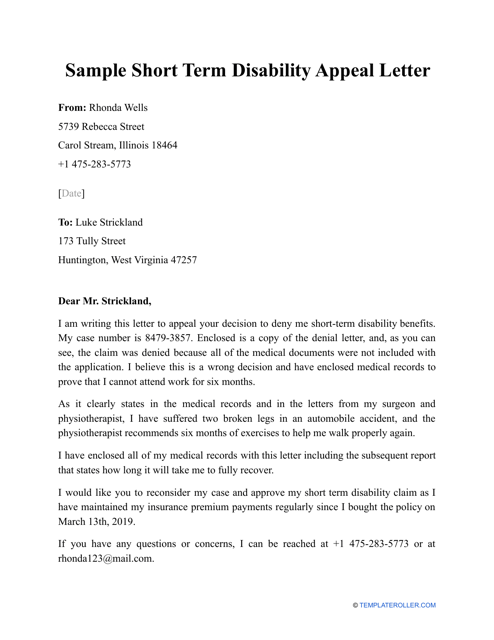
- Sample Short Term Disability Appeal Letter. If your insurance company has notified you about their decision not to award you benefits in the event of a temporary illness or injury, you have a right to argue their resolution within the established deadline;
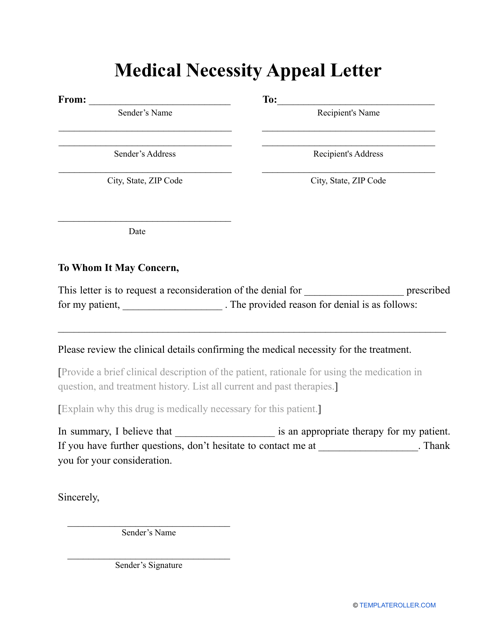
- Medical Necessity Appeal Letter Template. One of the most common reasons insurance providers decline applications to receive required coverage is the lack of medical necessity - meaning the treatment or medication was considered not justified in a certain scenario for a particular patient. If you believe this decision was unfair, you can ask for reconsideration with this Denial Insurance Appeal Letter;
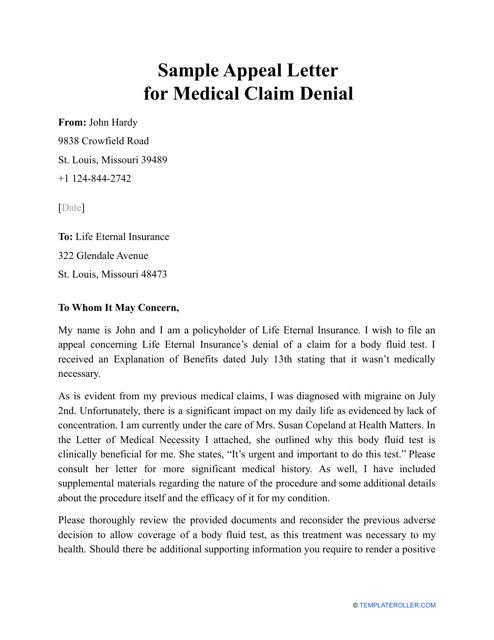
- Sample Appeal Letter for Medical Claim Denial. Often an insurance provider refuses to satisfy the demands of the insured individual listed in the Letter to Insurance Company for Claim, there are usually several weeks to file an internal appeal and ask them to change their mind whether you attach new evidence to your letter or try to elaborate on the documentation you have submitted already.
Haven't found the template you're looking for? Take a look at the related templates and samples below:
Documents:
7
This is a written statement sent to an insurance company to contest their refusal to provide a patient with funds to cover healthcare costs.
Individuals may use this type of document as a reference when they would like to request their insurance company to review the denial of their insurance claim.
This is a document that can be used when individuals would like to appeal a decision by their insurance company to deny authorization.
Individuals may use this type of document as a reference to dispute an unsatisfactory ruling of an insurance company regarding a long-term disability.
An employee who was denied proper insurance coverage to protect their financial standing during a temporary inability to do their job as a result of injury or illness may use this sample as a reference.
This is a document that you can use if you would like to appeal a decision made by your insurance company to deny your medical claim.
This is a document that individuals can use when they would like to appeal a decision about a medical necessity by their insurance company.