Health Partners Prior Authorization Form Templates
Health Partners Prior Authorization Form is a document used to request authorization for certain healthcare services or treatments. Prior authorization is a process utilized by health insurance companies to ensure that the recommended medical services or procedures meet the necessary criteria for coverage and are medically necessary. By submitting a prior authorization form, healthcare providers seek approval from the insurance company before proceeding with the requested services. This form allows providers to outline the details of the proposed treatment or service, including the diagnosis, the rationale for the request, and supporting medical documentation. The insurance company then reviews this information to make an informed decision regarding coverage and reimbursement for the requested healthcare service.
Documents:
1
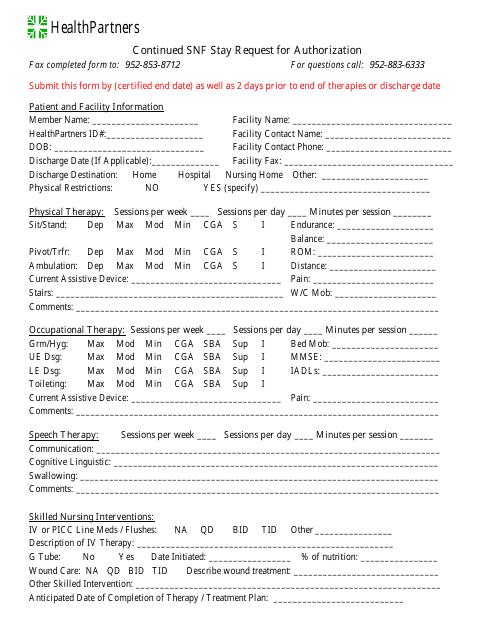
This form is used for requesting authorization for a continued stay at a skilled nursing facility (SNF) through Healthpartners.